Abstract
Justification
West syndrome is one of the commonest causes of epilepsy in infants and young children and is a significant contributor to neurodevelopmental morbidity. Multiple regimens for treatment are in use.
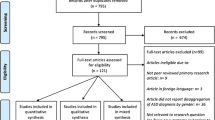
Process
An expert group consisting of pediatric neurologists and epileptologists was constituted. Experts were divided into focus groups and had interacted on telephone and e-mail regarding their group recommendations, and developed a consensus. The evidence was reviewed, and for areas where the evidence was not certain, the Delphi consensus method was adopted. The final guidelines were circulated to all experts for approval.
Recommendations
Diagnosis should be based on clinical recognition (history/home video recordings) of spasms and presence of hypsarrhythmia or its variants on electroencephalography. A magnetic resonance imaging of the brain is the preferred neuroimaging modality. Other investigations such as genetic and metabolic testing should be planned as per clinico-radiological findings. Hormonal therapy (adrenocorticotropic hormone or oral steroids) should be preferred for cases other than tuberous sclerosis complex and vigabatrin should be the first choice for tuberous sclerosis complex. Both ACTH and high dose prednisolone have reasonably similar efficacy and adverse effect profile for West syndrome. The choice depends on the preference of the treating physician and the family, based on factors of cost, availability of infrastructure and personnel for daily intramuscular injections, and monitoring side effects. Second line treatment options include anti-epileptic drugs (vigabatrin, sodium valproate, topiramate, zonisamide, nitrazepam and clobazam), ketogenic diet and epilepsy surgery.
Similar content being viewed by others
Change history
28 March 2021
An Erratum to this paper has been published: https://doi.org/10.1007/s13312-021-2185-7
References
Lux AL, Osborne JP. A Proposal for Case Definitions and Outcome Measures in Studies of Infantile Spasms and West Syndrome: Consensus Statement of the West Delphi Group. Epilepsia. 2004;45:1416–28.
Scheffer IE, Berkovic S, Capovilla G, et al. ILAE Classification of the Epilepsies: Position Paper of the ILAE Commission for Classification and Terminology. Epilepsia. 2017;58:512–21.
Kaushik JS, Patra B, Sharma S, Yadav D, Aneja S. Clinical spectrum and treatment outcome of West syndrome in children from Northern India. Seizure. 2013;22:617–621.
Surana P, Symonds, Srivastava P, et al. Infantile spasms: Etiology, lead time and treatment response in a resource limited setting. Epilespy Behav Rep. 2020 (In press)
Koutroumanidis M, Arzimanoglou A, Caraballo R, et al. The role of eeg in the diagnosis and classification of the epilepsy syndromes: A tool for clinical practice by the ilae neurophysiology task force (part 2). Epileptic Disord. 2017;19:385–437.
Kim H, Lee JH, Ryu HW, et al. Coexisting seizures in patients with infantile spasms confirmed by longterm video-electroencephalography monitoring. Epilepsy Res. 2012;101:70–5.
Hrachovy RA, Frost JD, Jr. Infantile epileptic encephalopathy with hypsarrhythmia (infantile spasms/West syndrome). J Clin Neurophysiol. 2003;20:408–425.
Hrachovy RA, Frost JD, Jr., Kellaway P. Hypsarrhythmia: Variations on the theme. Epilepsia. 1984;25:317–325.
Drury I, Beydoun A, Garofalo EA, Henry TR. Asymmetric hypsarrhythmia: Clinical electroencephalo-graphic and radiological findings. Epilepsia. 1995;36:41–47.
Iype M, Kunju PA, Saradakutty G, Mohan D, Khan SA. The early electroclinical manifestations of infantile spasms: A video EEG study. Ann Indian Acad Neurol. 2016;19:52–57.
Hayashi Y, Yoshinaga H, Akiyama T, Endoh F, Ohtsuka Y, Kobayashi K. Predictive factors for relapse of epileptic spasms after adrenocorticotropic hormone therapy in West syndrome. Brain Dev. 2016;38:32–39.
Kotagal P. Multifocal independent spike syndrome: Relationship to hypsarrhythmia and the slow spike-wave (Lennox-Gastaut) syndrome. Clin Electroencephalogr. 1995;26:23–9.
Wirrell EC, Shellhaas RA, Joshi C, Keator C, Kumar S, Mitchell WG. How should children with West syndrome be efficiently and accurately investigated? Results from the national infantile spasms consortium. Epilepsia. 2015;56:617–25.
Pellock JM, Hrachovy R, Shinnar S, et al. Infantile Spasms: A U.S. Consensus Report. Epilepsia. 2010;51:2175–89.
Sakaguchi Y, Kidokoro H, Ogawa C, et al. Longitudinal findings of MRI and PET in West syndrome with subtle focal cortical dysplasia. Am J Neuroradiol. 2018;39:1932–1937.
Chugani HT, Ilyas M, Kumar A, et al. Surgical treatment for refractory epileptic spasms: The Detroit series. Epilepsia 2015;56:1941–1949.
Patel J, Mercimek-Mahmutoglu S. Epileptic encephalo-pathy in childhood: A stepwise approach for identification of underlying genetic causes. Indian J Pediatr. 2016;83:1164–74.
Wilmshurst JM, Gaillard WD, Vinayan KP, et al. Summary of Recommendations for the Management of Infantile Seizures: Task Force Report for the ILAE commission of Pediatrics. Epilepsia. 2015;56:1185–1197.
Yuskaitis CJ, Ruzhnikov MRZ, Howell KB, et al. Infantile spasms of unknown cause: Predictors of outcome and genotype-phenotype correlation. Pediatr Neurol. 2018;87:48–56.
Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the american college of medical genetics and genomics and the association for molecular pathology. Genet Med. 2015;17:405–24.
Lux AL, Edwards SW, Hancock E, et al. The United Kingdom infantile spasms study comparing vigabatrin with prednisolone or tetracosactide at 14 days: A multicentre, randomised controlled trial. Lancet. 2004;364:1773–78.
Lux AL, Edwards SW, Hancock E, et al. The United Kingdom infantile spasms study (UKISS) comparing hormone treatment with vigabatrin on developmental and epilepsy outcomes to age 14 months: A multicentre randomised trial. Lancet Neurol. 2005;4:712–7.
O’Callaghan FJ, Edwards SW, Alber FD, et al. Safety and effectiveness of hormonal treatment versus hormonal treatment with vigabatrin for infantile spasms (ICISS): A randomised, multi- centre, open-label trial. Lancet Neurol. 2017;16:33–42.
O’Callaghan FJK, Edwards SW, Alber FD, et al. Vigabatrin with hormonal treatment versus hormonal treatment alone (iciss) for infantile spasms: 18-month outcomes of an open-label, rando-mised controlled trial. Lancet Child Adolesc Health. 2018;2:715–25.
Kunnanayaka V, Jain P, Sharma S, Seth A, Aneja S. Addition of pyridoxine to prednisolone in the treatment of infantile spasms: A pilot, randomized controlled trial. Neurol India. 2018;66:385–90.
Hussain SA, Shinnar S, Kwong G, et al. Treatment of infantile spasms with very high dose prednisolone before high dose adrenocorticotropic hormone. Epilepsia. 2014;55:103–07.
Eliyan Y, Heesch J, Alayari A, Rajaraman RR, Sankar R, Hussain SA. Very-high-dose prednisolone before ACTH for treatment of infantile spasms: Evaluation of a standardized protocol. Pediatr Neurol. 2019;99:16–22.
Li S, Zhong X, Hong S, Li T, Jiang L. Prednisolone/prednisone as adrenocorticotropic hormone alternative for infantile spasms: A meta-analysis of randomized controlled trials. Dev Med Child Neurol. 2020;62:575–80.
Chang YH, Chen C, Chen SH, Shen YC, Kuo YT. Effectiveness of corticosteroids versus adrenocorticotropic hormone for infantile spasms: A systematic review and meta-analysis. Ann Clin Transl Neurol. 2019;6:2270–81.
Hrachovy RA, Frost JD, Jr., Glaze DG. High-dose, long-duration versus low-dose, short-duration corticotropin therapy for infantile spasms. J Pediatr. 1994;124:803–6.
Chellamuthu P, Sharma S, Jain P, Kaushik JS, Seth A, Aneja S. High dose (4 mg/kg/day) versus usual dose (2 mg/kg/day) oral prednisolone for treatment of infantile spasms: An open-label, randomized controlled trial. Epilepsy Res. 2014;108:1378–84.
Matsumoto A, Watanabe K, Negoro T, et al. Prognostic factors of infantile spasms from the etiological viewpoint. Brain Dev. 1981;3:361–4.
Ko A, Youn SE, Chung HJ, et al. Vigabatrin and high-dose prednisolone therapy for patients with west syndrome. Epilepsy Res. 2018;145:127–33.
Maguire MJ, Hemming K, Wild JM, Hutton JL, Marson AG. Prevalence of visual field loss following exposure to vigabatrin therapy: A systematic review. Epilepsia. 2010;51:2423–31.
Go CY, Mackay MT, Weiss SK, et al. Evidence-Based Guideline Update: Medical Treatment of Infantile Spasms. Report of the Guideline Development Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology, 2012;78:1974–80.
Kossoff EH, Hedderick EF, Turner Z, Freeman JM: A case-control evaluation of the ketogenic diet versus acth for new-onset infantile spasms. Epilepsia, 2008; 49:1504–09.
van der Louw E, van den Hurk D, Neal E, et al. Ketogenic diet guidelines for infants with refractory epilepsy. Eur J Paediatr Neurol, 2016;20:798–809.
Sharma S, Sankhyan N, Gulati S, Agarwala A. Use of the modified Atkins diet in infantile spasms refractory to first-line treatment. Seizure. 2012;21:45–8.
Abel TJ, Losito E, Ibrahim GM, Asano E, Rutka JT. Multimodal localization and surgery for epileptic spasms of focal origin: A review. Neurosurg Focus. 2018;45:E4.
Whitney R, Jan S, Zak M, McCoy B. The utility of surveillance electroencephalography to guide early antiepileptic drug therapy in infants with tuberous sclerosis complex. Pediatr Neurol. 2017;72:76–80.
Acknowledgment
Dr Sushma Goyal and Dr Chaitanya Datar for helpful inputs in the EEG and genetic testing sections, respectively.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Contributors
SS and RM: conceptualized the idea; SS, JSK, KS, JS, JNG, RM, KPV: constituted the writing committee and drafted the manuscript; JSK devised and conducted Delphi process. All the authors approved the final version of the manuscript.
Funding
The logistics of faculty travel for the West syndrome Delphi Consensus meeting was funded by Intas Pharmaceutical Ltd. and Ferring Pharmaceuticals. The venue support was provided by Army Hospital, Research and Referral, Dhaula Kuan, New Delhi. None of the funding sources had any role in content of the discussion during meeting, or in report or manuscript preparation. They did not have access to any version of the manuscript.
Competing interests
None stated.
Association of Child Neurology — Indian Epilepsy Society Expert Committee
Razia Adam (Hyderabad, Telengana); Satinder Aneja (Noida, Uttar Pradesh); Biswaroop Chakrabarty (Delhi); Arijit Chattopadhyay (Kolkata); Saurabh Chopra (Delhi), Rajni Farmania (Delhi); Pradnya Gadgil (Mumbai, Maharashtra); Divyani Garg (Delhi); Jatinder Singh Goraya (Ludhiana, Punjab); Sheffali Gulati (Delhi); Aparajita Gupta (Kolkata, West Bengal); Rachana Dubey Gupta (Indore, Madhya Pradesh); Vineet Bhushan Gupta (Delhi); Anaita Udwadia Hedge (Mumbai, Maharashtra); Mary Iype (Trivandrum, Kerala); Vivek Jain (Jaipur, Rajasthan); Prashant Jauhari (Delhi); Veena Kalra (Delhi); Mahesh Kamate (Belgavi, Karnataka); Lakshminarayanan Kannan (Chennai, Tamil Nadu); Anupriya Kaur (Chandigarh); Gurpreet Kochar (Ludhiana, Punjab); Ramesh Konanki (Hyderabad, Telangana); Ajay Kumar (Patna, Bihar); PAM Kunju (Trivandrum, Kerala); Lokesh Lingappa (Hyderabad, Telengana); Priyanka Madaan (Chandigarh); Ranjith Kumar Manokaran (Chennai, Tamil Nadu); MM Mehendiratta (Delhi); Ramshekhar Menon (Trivandrum, Kerala); Devendra Mishra (Delhi); Debasis Panigrahi (Bhubneshwar, Orissa); Harsh Patel (Ahmedabad, Gujarat); Sandeep Patil (Pune, Maharashtra); Bijoy Patra (Delhi); Leema Pauline (Chennai, Tamil Nadu); KVN Raju (Bangalore, Karnataka); Arushi Gehlot Saini (Chandigarh); Lokesh Saini (Chandigarh); Naveen Sankhyan (Chandigarh); Rachna Sehgal (Delhi); Anita Sharma (Delhi); Pratibha Singhi (Gurgaon, Haryana); Vishal Sondhi (Pune, Maharasthra); Renu Suthar (Chandigarh); Sanjeev V Thomas (Trivandrum, Kerala); Manjari Tripathi (Delhi); Vrajesh Udani (Mumbai, Maharasthra); Prashant Utage (Hyderabad, Telengana); Nitish Vora (Ahmedabad, Gujarat); Sangeeta Yoganathan (Vellore, Tamil Nadu).
Rights and permissions
About this article
Cite this article
Sharma, S., Kaushik, J.S., Srivastava, K. et al. Association of Child Neurology (AOCN) — Indian Epilepsy Society (IES) Consensus Guidelines for the Diagnosis and Management of West Syndrome. Indian Pediatr 58, 54–66 (2021). https://doi.org/10.1007/s13312-021-2097-6
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-021-2097-6