Summary
The objective of this cluster randomized trial was to determine if Rojiroti microfinance, for poor Indian women in the state of Bihar, improves child nutrition. Women with children under 5 years formed self-help groups, and saved their money to provide loans to group members. After an interval of 6 months, they received larger external loans and tolas were randomized to receive Rojiroti immediately or after 18 months. The primary outcome measure was mean weight for height Z score (WHZ) of children under 5 years in the intervention versus control tolas who attended for weight and height measurement 18 months after randomization. Total 28 tolas to each arm were randomized and data were collected from 2469 children (1560 mothers) at baseline and 2064 children (1326 mothers) at follow-up. WHZ was calculated for 1718 children at baseline and 1377 (674 intervention and 703 control) at follow-up. At 18 months, mean WHZ was significantly higher for intervention (–1.02) vs controls (–1.37; regression coefficient adjusted for clustering b=0.38, 95% CI 0.16 to 0.61, P=0.001). Significantly fewer children were wasted in the intervention group (122, 18%) vs control (200, 29%; OR=0.46, 95% CI 0.28 to 0.74, P=0.002. The authors concluded that in marginalized communities of rural Bihar, child nutrition was better in thosewho received Rojiroti microfinance, compared with controls.
Similar content being viewed by others
References
Ojha S, Szatkowski L, Sinha R, Yaron G, Fogarty A, Allen SJ, et al. Rojiroti microfinance and child nutrition: a cluster randomized trial. Arch Dis Child. 2020; 105:229–35.
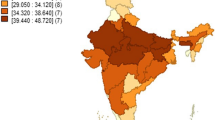
Government of India, Ministry of Health and Family Welfare. National Family Health Survey-4 2015-16. Available from: http://rchiips.org/NFHS/pdf/NFHS4/India.pdf. Accessed April 13, 2020.
References
Development Initiatives. 2018 Global Nutrition Report: Shining a light to spur action on nutrition [Internet]. Development Initiatives Poverty Research Ltd, Bristol, UK; 2018. Available from: https://globalnutritionreport.org/reports/global-nutrition-report-2018/. Accessed April 10, 2020.
Institute for Health Metrics and Evaluation. GBD Compare data visualization [Internet]. Institute for Health Metrics and Evaluation, University of Washington, 2018. Available from: http://www.healthdata.org/data-visualization/gbdcompare. Accessed April 10, 2020.
Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Maternal and child undernutrition: Consequences for adult health and human capital. Lancet. 2008;371: 340–57.
United Nations Department of Economic and Social Affairs. Sustainable Development Goal 2. [Internet]. United Nations; 2019. Available from: https://sustainable-development.un.org/sdg2. Accessed April 10, 2020.
WHO Commission on Social Determinants of Health, World Health Organization, editors. Closing the gap in a generation: health equity through action on the social determinants of health: Commission on Social Determinants of Health final report. Geneva, Switzerland: World Health Organization, Commission on Social Determinants of Health; 2008.p.246.
Subramanyam MA, Kawachi I, Berkman LF, Subramanian SV. Is economic growth associated with reduction in child undernutrition in India? PLoS Med. 2011;8: e1000424.
Ministry of Women and Child Development, Government of India. Poshan Abhiyan. PM’s overarching scheme for holistic nourishment [Internet]. Available from: https://icds-wcd.nic.in/nnm/home.htm#. Accessed April 10, 2020.
Pandey VL, Mahendra Dev S, Jayachandran U. Impact of agricultural interventions on the nutritional status in South Asia: A review. Food Policy. 2016; 62:28–40.
Ojha S, Szatkowski L, Sinha R, Yaron G, Fogarty A, Allen SJ, et al. Rojiroti microfinance and child nutrition: A cluster randomised trial. Arch Dis Child. 2020;105:229–35.
Chaturvedi S, Ramji S, Arora NK, Rewal S, Dasgupta R, V Deshmukh, et al. Time-constrained mother and expanding market: Emerging model of under-nutrition in India. BMC Public Health. 2016;16:632.
Balarajan Y, Selvaraj S, Subramanian S. Health care and equity in India. Lancet. 2011; 377:505–15.
References
UNICEF, WHO & World Bank Group 2018. Joint Child Malnutrition Estimates 2019 Edition. Available at http://data.unicef.org/resource/jme/. Assessed on April 14, 2020.
Ruel MT, Alderman H; Maternal and Child Nutrition Study group. Nutrition-sensitive interventions and programmes: How can they help to accelerate progress in improving maternal and child nutrition? Lancet. 2013; 382:536–51.
Ojha S, Szatkowski L, Sinha R, Yaron G, Fogarty A, Allen SJ, et al. Rojiroti microfinance and child nutrition: A cluster randomised trial Arch Dis Child. 2020; 105:229–35.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Mathew, J.L., Das, M.K. & Kumar, P. Cluster Randomized Trial Evaluating Impact of a Community-based Microfinance Scheme on Childhood Nutritional Status. Indian Pediatr 57, 459–464 (2020). https://doi.org/10.1007/s13312-020-1822-x
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-020-1822-x