Abstract
Background
Maternal urinary iodine concentration (MUIC) and percentage of neonates with Thyroid stimulating hormone (TSH) >5 mIU/L are amongst the parameters suggested for assessing adequate iodine status.
Objective
To assess the correlation between MUIC and neonatal TSH levels.
Study design
Cross-sectional.
Settings
Tertiary care center in Delhi, India, between November 2015 to November 2016.
Participants
Postnatal mother-neonate dyads.
Methods
TSH levels assessed among neonatal samples were stratified as below and above 5 mIU/L. MUIC was measured in 544 mothers, 400 mother-neonate dyads with neonatal TSH levels >5 mIU/L (cases) and 144 mother-neonate newborn mother dyads with neonatal TSH <5 mIU/L (controls).
Results
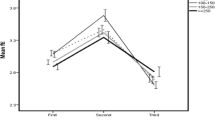
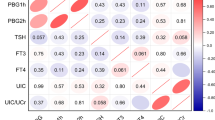
The percentage of mothers with iodine insufficiency (9.8% vs 5.6%) as well as iodine excess (54.3% vs 41.7%) were significant higher in cases than controls. Mean TSH was also higher (P=0.0002) in both the iodine deficient and iodine excess group. There was no correlation between neonatal TSH values and MUIC.
Conclusions
Lack of correlation between neonatal TSH and MUIC is due to iodine excess together with iodine deficiency.
Similar content being viewed by others
References
Pandav CS, Yadav K, Srivastava R, Pandav R, Karmarkar MG. Iodine deficiency disorders (IDD) control in India. Indian J Med Res. 2013;138:418–33.
Vandevijvere S, Coucke W, Vanderpas J, Trumpff C, Fauvart M, Meulemans A, et al. Neonatal thyroid-stimulating hormone concentrations in Belgium: A useful indicator for detecting mild iodine deficiency? PLoS One. 2012;7:e47770.
Vanderpump MPJ, Lazarus JH, Smyth PP, Laurberg P, Holder RL, Boelaert K, et al. Iodine status of UK schoolgirls: A cross-sectional survey. Lancet. 2011;377:2007–12.
Rah JH, Anas AM, Chakrabarty A, Sankar R, Pandav CS, Aguayo VM. Towards universal salt iodisation in India: Achievements, challenges and future actions. Matern Child Nutr. 2015;11:483–96.
Grewal E, Khadgawat R, Gupta N, Desai A, Tandon N. Assessment of iodine nutrition in pregnant north Indian subjects in three trimesters. Indian J Endocrinol Metab. 2013;17:289–93.
Marwaha RK, Tandon N, Desai A, Kanwar R, Mani K. Iodine nutrition in upper socioeconomic school children of Delhi. Indian Pediatr. 2010;47:335–8.
World Health Organization. A Guide for Programme Managers. Assessment of Iodine Deficiency Disorders and Monitoring their Elimination. Geneva: World Health Organization; 2007.
Hamza R, Youssef A, Mouharam W, Danasoury AEl. Maternal and neonatal iodine nutrition in Cairo. Internet J Pediatr Neonatol. 2007;8:2.
Wolff J, Chaikoff IL. Plasma inorganic iodide as a homeostatic regulator of thyroid function. J Biol Chem. 1948;174:555–64.
Usha Menon V, Sundaram KR, Unnikrishnan AG, Jayakumar RV, Kumar NV. High prevalence of undetected thyroid disorders in an iodine sufficient adult south Indian population. J Indian Med Assoc. 2009;107:72.
Marwaha RK, Tandon N, Karak AK, Gupta N, Verma K, Kochupillai N. Hashimoto’s thyroiditis: Countrywide screening of goitrous healthy young girls in postiodization phase in India. J Clin Endocrinol Metab. 2000;85: 3798–802.
Katagiri R, Yuan X, Kobayashi S, Sasaki S. Effect of excess iodine intake onthyroid diseases in different populations: A systematic review and meta-analyses including observational studies. PLoS One. 2017;12: p. e0173722.
Bürgi H. Iodine excess. Best Pract Res Endocrinol Metab. 2010;24:107–15.
Funding
Funding: Science and Engineering Research Board, New Delhi for NBS study in Delhi state vide Grant # IR/SO/LC-0001/2012.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sait, H., Kapoor, S., Jindal, A. et al. Association Between Neonatal Thyroid Stimulating Hormone Status and Maternal Urinary Iodine Status. Indian Pediatr 56, 472–475 (2019). https://doi.org/10.1007/s13312-019-1571-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-019-1571-x