Abstract
Objective
To review the Mid-upper arm circumference (MUAC) cut-off currently being used to identify Severe Acute Malnutrition (SAM) as currently defined using Weight-for-Height.
Methods
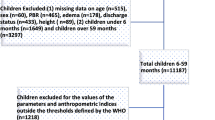
Cross-sectional study conducted in 24 villages of a Primary Health Centre in Wardha district of Maharashtra among 2650 children between the ages of 6 to 59 months.
Results
For identifying SAM, sensitivity of MUAC was 23.5% and specificity was 99.7% for cut-off <11.5 cm. Using Youden index, best Mid-upper arm circumference cut-off point to identify SAM was <13 cm with sensitivity of 74.5% and specificity of 92.7%. Using Receiver operating characteristics curve, best MUAC cut-off point was 12.8 cm with 74.5% sensitivity and 92.7% specificity. Area under curve was 0.88 (95%CI: 0.85-0.91).
Conclusion
The current MUAC cut-off of <11.5 cm for detecting SAM needs to be increased to ensure that children, who need referral for management of malnutrition, are not missed.
Similar content being viewed by others
References
International Institute for Population Sciences. India National Family Health Survey (NFHS–3), 2005–06. International Institute for Population Sciences; 2007.
Kapil U, Sachdev HP. Management of children with severe acute malnutrition: A national priority. Indian Pediatr. 2010;47:651–3.
Myatt M, Duffield A. Weight–for–height and MUAC for estimating the prevalence of acute undernutrition. Report for IASC, UNICEF. 2007:104–10.
Myatt M, Khara T, Collins S. A review of methods to detect cases of severely malnourished children in the community for their admission into community–based theraputic care programs. Food Nutr Bull. 2006;27:S7–23.
Berkley J, Mwangi I, Griffiths K, Ahmed I, Mithwani S, English M, et al. Assessment of severe malnutrition among hospitalized children in rural Kenya. JAMA. 2005;294:591–7.
Vella V, Tomkins A, Ndiku J, Marshal T, Cortinovis I. Anthropometry as a predictor for mortality among Ugandan children, allowing for socio–economic variables. Eur J Clin Nutr. 1994;48:189–97.
Chen LC, Chowdhury A, Huffman SL. Anthropometric assessment of energy–protein malnutrition and subsequent risk of mortality among preschool aged children. Am J Clin Nutr. 1980;33:1836–45.
Trowbridge FL, Sommer A. Nutritional anthropometry and mortality risk. Am J Clin Nutr. 1981;34:2591–2.
World Health Organization. WHO Child Growth Standards and the Identification of Severe Acute Malnutrition in Infants and Children: A Joint Statement by the World Health Organization and the United Nations Children’s Fund: World Health Organization (WHO); 2009.
Fernandez MA, Delchevalerie P, Van Herp M. Accuracy of MUAC in the detection of severe wasting with the new WHO growth standards. Pediatrics. 2010;126:195–201.
Dasgupta R, Sinha D, Jain SK, Prasad V. Screening for SAM in the community: Is MUAC a ‘simple tool’? Indian Pediatr. 2013;50:154–5.
Shekhar S, Shah D. Validation of mid–upper–arm circumference cut–offs to diagnose severe wasting in Indian children. Indian Pediatr. 2012;49:496–7.
Kumar R, Aggarwal AK, Iyengar SD. Nutritional status of children: Validity of mid–upper arm circumference for screening undernutrition. Indian Pediatr. 1996;33: 189–96.
Kapil U, Pandey RM, Bansal R, Pant B, Varshney AM, Yadav CP, et al. Mid–upper arm circumference in detection of weight–for–height Z–score below–3 in children aged 6–59 months. Public Health Nutr. 2018;21:1794–9.
Grijalva–Eternod CS, Wells JCK, Girma T, Kæstel P, Admassu B, Henrik Friis H, et al. Mid upper arm circumference and weight–for–length Z–scores have different associations with body composition: evidence from a cohort of Ethiopian infants. Am J Clin Nutr. 2015;102:593.
Shaw NJ, Crabtree NJ, Kibirige MS, Fordham JN. Ethnic and gender differences in body fat in British schoolchildren as measured by DXA. Arch Dis Child. 2007;92:872–5.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sougaijam, R., Gupta, S., Raut, A. et al. Validating the MUAC (Mid-upper arm circumference) Cut-off for Detection of Severe Acute Malnutrition in Children Aged 6–59 Months in Rural Maharashtra. Indian Pediatr 56, 209–212 (2019). https://doi.org/10.1007/s13312-019-1502-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-019-1502-x