Abstract
This review highlights pitfalls and challenges in interpreting neonatal hormone reports. Pre-analytical errors contribute to nearly 50% of all errors. Modern chemiluminescence assay are more accurate, have lower risk of Hook’s effect, but continue to have problems of assay interference. Liquid chromatography mass spectroscopy is gold standard for most hormone assays. Neonatal hypoglycemia diagnostic cut-offs are lower than adults. Random growth hormone testing is of value in diagnosing growth hormone deficiency in neonates. 17-hydroxy-progesterone testing in first three days of life for congenital adrenal hyperplasia (CAH) remains a challenge due to crossreactivity with maternal circulating steroids, prematurity and lack of adrenal maturation. Both T4 and TSH testing is encouraged after 48 hours of delivery for diagnosing neonatal hypothyroidism; repeat testing should be done immediately for confirmation of diagnosis. There is an urgent need to develop age- sex- and ethnicity-based normative data for different hormone parameters in neonates. Laboratory should develop their own neonatal references and avoid using ranges from manufacturers. In neonatal endocrinopathies, the clinical scenario should primarily dictate the treatment formulation with hormonal assay to supplement treatment.
Similar content being viewed by others
References
Coffin CM, Hamilton MS, Pysher TJ, Bach P, Ashwood E, Schweiger J, et al. Pediatric laboratory medicine current challenges and future opportunities. Am J Clin Pathol. 2002;117:683–90.
Verras P, Greaves R. Interpreting paediatric biochemistry results. Aust Prescr. 2005;28:126–9.
Dutta D, Chowdhury S. Endocrine Labomas. Indian J Endocr Metab. 2012;16:S275–8
Harms E, Olgemöller B. Neonatal screening for metabolic and endocrine disorders. Dtsch Arztebl Int. 2011;108: 11–22.
Thornton PS, Stanley CA, De Leon DD, Harris D, Haymond MW, Hussain K, et al.; Pediatric Endocrine Society. Recommendations from the Pediatric Endocrine Society for evaluation and management of persistent hypoglycemia in neonates, infants, and children. J Pediatr. 2015;167:238–45.
McKinlay CJ, Alsweiler JM, Ansell JM, Anstice NS, Chase JG, Gamble GD, et al.; CHYLD Study Group. Neonatal glycemia and neurodevelopmental outcomes at 2 years. N Engl J Med. 2015;373:1507–18.
Stanley CA, Rozance PJ, Thornton PS, De leon DD, Harris D, Haymond MW, et al. Re-evaluating “transitional neonatal hypoglycemia”: mechanism and implications for management. J Pediatr. 2015;166:1520–25.
Nangia S. Point of care estimation of blood glucose in neonates. Indian Pediatr. 2012;49:612–3.
Hawkes CP, Grimberg A. Measuring growth hormone and insulin-like growth factor-I in infants: What is normal? Pediatr Endocrinol Rev. 2013;11:126–46.
Kurtoðlu S, Kondolot M, Mazicioðlu MM, Hatipoðlu N, Akin MA, Akyildiz B. Growth hormone, insulin like growth factor-1, and insulin-like growth factor-binding protein-3 levels in the neonatal period: a preliminary study. J Pediatr Endocrinol Metab. 2010;23:885–9.
Wit JM, van Unen H. Growth of infants with neonatal growth hormone deficiency. Arch Dis Child. 1992;67:920–4.
Senniappan S, Hussain K. An evaluation of growth hormone and IGF-1 responses in neonates with hyperinsulinaemic hypoglycaemia. Int J Endocrinol. 2013;2013:638257.
Ong K, Kratzsch J, Kiess W, Costello M, Scott C, Dunger D. Size at birth and cord blood levels of insulin, insulin-like growth factor I (IGF-I), IGF-II, IGF-binding protein-1 (IGFBP-1), IGFBP-3, and the soluble IGF-II/mannose-6- phosphate receptor in term human infants. The ALSPAC Study Team. Avon Longitudinal Study of Pregnancy and Childhood. J Clin Endocrinol Metab. 2000;85:4266–9.
Speiser PW, Azziz R, Baskin LS, Ghizzoni L, Hensle TW, Merke DP, et al. Congenital adrenal hyperplasia due to steroid 21-Hydroxylase deficiency: An Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2010; 95:4133–60
van der Kamp HJ, Oudshoorn CG, Elvers BH, van Baarle M, Otten BJ, Wit JM, et al. Cutoff levels of 17-alphahydroxyprogesterone in neonatal screening for congenital adrenal hyperplasia should be based on gestational age rather than on birth weight. J Clin Endocrinol Metab. 2005;90:3904–7.
al Saedi S, Dean H, Dent W, Cronin C. Reference ranges for serum cortisol and 17-hydroxyprogesterone levels in preterm infants. J Pediatr. 1995;126:985–7.
La Franchi SH. Approach to the diagnosis and treatment of neonatal hypothyroidism. J Clin Endocrinol Metab. 2011;96:2959–2967.
Wang SL, Su PH, Jong SB, Guo YL, Chou WL, Päpke O. In utero exposure to dioxins and polychlorinated biphenyls and its relations to thyroid function and growth hormone in newborns. Environ Health Perspect. 2005;113:1645–50.
Williams FL, Simpson J, Delahunty C, Ogston SA, Bongers-Schokking JJ, Murphy N; Collaboration from the Scottish Preterm Thyroid Group. Developmental trends in cord and postpartum serum thyroid hormones in preterm infants. J Clin Endocrinol Metab. 2004;89:5314–20.
Straussman S, Levitsky LL. Congenital hypothyroidism–Monitoring thyroid function in infants. Eur Endocrinol. 2012;8:53–6.
Williams FL, Ogston SA, van Toor H, Visser TJ, Hume R. Serum thyroid hormones in preterm infants: associations with postnatal illnesses and drug usage. J Clin Endocrinol Metab. 2005;90:5954–63.
Mahyar A. Effects of exchange transfusion on neonatal thyroid function. Indian J Pediatr. 2007;74:511–2.
Sharma LK, Sharma N, Gadpayle AK, Dutta D. Prevalence and predictors of hyperprolactinemia in subclinical hypothyroidism. Eur J Intern Med. 2016;35:106–10.
Kumar M, Mukhopadhyay S, Dutta D. Challenges and controversies in diagnosis and management of gonadotropin dependent precocious puberty: An Indian perspective. Indian J Endocrinol Metab. 2015;19:228–35.
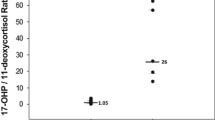
Garagorri JM, Rodríguez G, Lario-Elboj AJ, Olivares JL, Lario-Muñoz A, Orden I. Reference levels for 17- hydroxyprogesterone, 11-desoxycortisol, cortisol, testosterone, dehydroepiandrosterone sulfate and androstenedione in infants from birth to six months of age. Eur J Pediatr. 2008;167:647–53.
Sharma LK, Dutta D, Gadpayle AK, Sharma N. The increasing problem of subclinical and overt hypervitaminosis-D in India: An institutional experience and review. Nutrition. 2017;34:76–81.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Chittawar, S., Dutta, D., Khandelwal, D. et al. Neonatal endocrine labomas - pitfalls and challenges in reporting neonatal hormonal reports. Indian Pediatr 54, 757–762 (2017). https://doi.org/10.1007/s13312-017-1170-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13312-017-1170-7