Abstract
Spinal cord injury (SCI) disrupts the autonomic nervous system (ANS), impairing its ability to coordinate organ function throughout the body. Emerging data indicate that the systemic pathology that manifests from ANS dysfunction exacerbates intraspinal pathology and neurological impairment. Precisely how this happens is unknown, although new data, in both humans and in rodent models, implicate changes in the composition of bacteria in the gut (i.e., the gut microbiota) as disease-modifying factors that are capable of affecting systemic physiology and pathophysiology. Recent data from rodents indicate that SCI causes gut dysbiosis, which exacerbates intraspinal inflammation and lesion pathology leading to impaired recovery of motor function. Postinjury delivery of probiotics containing various types of “good” bacteria can partially overcome the pathophysiologal effects of gut dysbiosis; immune function, locomotor recovery, and spinal cord integrity are partially restored by a sustained regimen of oral probiotics. More research is needed to determine whether gut dysbiosis varies across a range of clinically relevant variables, including sex, injury level, and injury severity, and whether changes in the gut microbiota can predict the onset or severity of common postinjury comorbidities, including infection, anemia, metabolic syndrome, and, perhaps, secondary neurological deterioration. Those microbial populations that dominate the gut could become “druggable” targets that could be manipulated via dietary interventions. For example, personalized nutraceuticals (e.g., pre- or probiotics) could be developed to treat the above comorbidities and improve health and quality of life after SCI.
Similar content being viewed by others
Paralysis and sensory loss are devastating consequences of spinal cord injury (SCI). Less obvious to the public, but not less incapacitating for the individual affected by SCI, are loss of bladder and bowel function, an increase in susceptibility to infections, depression and anxiety, fatigue, deficits in thermoregulation, and an increase in cardiovascular dysfunction and disease. All of these latter complications result from damage to the autonomic nervous system.
Within the spinal cord, autonomic function is primarily coordinated through cholinergic sympathetic preganglionic neurons (SPNs) that reside in the intermediate lateral gray matter of the thoracic and upper lumbar spinal cord. Although recent data indicate that autonomic efferents in sacral spinal cord also are sympathetic (rather than parasympathetic) [1]. When the spinal cord is injured, especially at high spinal levels, most or all brainstem circuitry that provides tonic “executive” control over SPNs is lost. Injury to these presympathetic axons “unplugs” SPNs from the brain and brainstem, eliminating feedback regulation of autonomic reflexes that are initiated below the level of injury by, for example, visceral or somatic sensory nerves that relay information into the spinal cord from the bowel, bladder, or muscle. Once activated, SPNs signal to second-order postganglionic adrenergic neurons that innervate the cardiovascular system (changing heart rate, blood pressure), other viscera (e.g., kidney, pancreas, liver, stomach, intestine, etc.), and lymphoid tissues (e.g., bone marrow, spleen). After SCI, the loss of descending control over SPNs causes autonomic reflex circuitry to become dysfunctional creating pathology including autonomic dysreflexia and SCI–immune depression syndrome [2,3,4,5,6,7]. SCI also causes an autonomic imbalance in the gastrointestinal tract, which leads to deficits in colonic motility, mucosal secretions, and vascular tone [8, 9].
The spinal cord, gut, and immune system form an interconnected triad of “super systems” that together help to maintain human health. Damage or dysfunction to any part of the triad breaks homeostasis and causes disease. After SCI, the initial break in the spinal cord–gut–immune axis occurs in the spinal cord, owing to loss of the aforementioned autonomic reflex control over the gastrointestinal tract and lymphoid tissues, including bone marrow and spleen [10, 11]. Less is known about how SCI affects the function of the immune cells that reside in gut-associated lymphoid tissues (GALT) or whether SCI-induced changes in GALT affect postinjury morbidity or mortality. A comprehensive understanding of how SCI causes cellular and molecular changes in GALT will require that we also determine how the gut microbiota are affected by SCI.
The gut microbiota are a heterogeneous community of microbes that live in the gastrointestinal tract, mostly in the large intestine. The species present and the relative abundance of these species varies throughout the length of the gastrointestinal tract (see [12,13,14] for a review of varied types and functions of gut microbiota in mammalian intestine). These microbes outnumber mammalian cells by ~10:1 and the gut microbiome (genes expressed by gut microbiota) contains ~100-fold more genes than the human genome [15, 16], although recent estimates place the ratio at ~1:1 [17]. Regardless, in mammals a vast microbial network exists that is critical for normal digestion, nutrient absorption, and the development, metabolism, and function of cells throughout the body [18,19,20]. Recent data indicate that gut microbes also regulate both normal development and disease pathogenesis in the central nervous system (CNS) [21,22,23,24].
Altering the composition of the gut microbiota creates a state of “dysbiosis” where the balance between helpful bacteria and pathogenic bacteria (“pathobionts”) is skewed, usually favoring pathobionts. Common causes of gut dysbiosis include antibiotic use, prolonged stress, and gastrointestinal dysfunction [18, 25, 26]. Autoimmune diseases (e.g., multiple sclerosis, type 1 diabetes, rheumatoid arthritis), allergy, and metabolic disorders have been linked to gut dysbiosis [27,28,29,30,31,32,33]. Similarly, dysbiosis has been implicated in the onset or progression of neurological diseases, including autism, pain, depression, anxiety, and stroke [23, 24, 34,35,36,37,38,39,40].
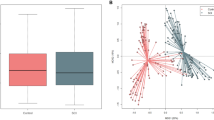
Recent data from our laboratory show that traumatic SCI also causes gut dysbiosis and that dysbiosis impairs functional recovery and exacerbates intraspinal inflammation and lesion pathology (Fig. 1) [41]. Specifically, mice (C57BL/6, females) received mid-thoracic SCIs using a clinically relevant model of controlled contusion injury. At baseline and at different times postinjury, fecal samples were collected and 16s rRNA sequencing was used to quantify time-dependent changes in gut microbiota. The 16S rRNA gene contains hypervariable regions (V1–9) that, when sequenced, provide specific identification of bacterial communities. Data analyses revealed that Bacteroidales and Clostridiales, the 2 major bacterial orders in the gut [42, 43], were inversely regulated by SCI—by 3 weeks postinjury, Bacteroidales (phylum Bacteroidetes) decreased ~30%, whereas Clostridiales (phylum Firmicutes) increased ~250% relative to preinjury values. Significant changes in these major bacterial taxa were accompanied by lesser but consistent changes in minor taxa, including Anaeroplasmatales, Turicibacterales, and Lactobacillales. These changes in gut bacteria populations persisted, and in some cases increased by 4 weeks postinjury. Given that the bacterial orders Bacteroidales and Clostridiales together constitute >80% of all species residing in the gut, significant and lasting changes in their relative population densities after SCI will likely influence numerous physiological processes, both within and outside the gastrointestinal tract. Indeed, although gut microbiota live in the gastrointestinal tract, these bacteria likely affect spinal cord structure and function by various modes of communication. For example, the constant dialogue that occurs between gut microbiota and GALT immune cells produces cytokines and other metabolites that circulate and affect CNS function [44]. After SCI, we found that gut dysbiosis is associated with marked changes in the relative proportion of immune cells found in mesenteric lymph nodes and Peyer’s patches. An increase in the synthesis of inflammatory and immunoregulatory cytokines also occurred in GALT in parallel with changes in immune cell populations [41]. Gut microbes also produce neuroactive metabolites (short-chain fatty acids, choline) and neurotransmitters (γ-aminobutyric acid, serotonin, dopamine, acetylcholine), which can affect CNS function by activating vagal afferent nerve fibers in the intestines [19, 22, 34, 45, 46].
Spinal cord injury (SCI) disrupts brain and brainstem control over the sympathetic preganglionic neurons (SPNs) that are located in the thoracic spinal cord. This break in executive control over SPNs breaks homeostasis and control over postganglionic neurons (e.g., projecting from celiac ganglia) that innervate the gastrointestinal (GI) tract. Loss of coordinated neural control over the GI tract will impair motility, mucous secretion, immune surveillance, and epithelial barrier permeability in the small and large intestines. Together, these changes in the GI tract can cause bacterial translocation and gut dysbiosis (a). After SCI, probiotic treatment may normalize the gut microbiota leading to improvements in gut barrier integrity (b)
Gut microbes may also exit the gastrointestinal tract and colonize other tissues. Indeed, in our mouse model of SCI, we found evidence of increased intestinal barrier permeability with bacterial translocation to mesenteric lymph nodes, liver, spleen, kidney, and blood [41]. Chronic systemic immune suppression, intestinal obstruction, and impaired intestinal motility—all complications of SCI—can independently cause bacterial translocation [47]. When this occurs, gut microbes or microbial components (e.g., endotoxin, peptidoglycan) can directly activate immune receptors (e.g., Toll-like receptors) on glia, neurons, hematopoietic stem/precursor cells, and mature immune cells [48, 49]. These are important considerations given that gut dysbiosis also develops in people after a SCI [50].
In a small cohort of SCI and able-bodied human subjects (30 SCI patients vs 10 age-matched able-bodied controls), gut microbe population dynamics were evaluated from fecal samples using 16s rRNA sequencing. All individuals had sustained a SCI at least 12 months prior to sample collection. Data from this study showed that butyrate-producing bacteria, such as Roseburia and Pseudobutyrivibrio, decreased in individuals with SCI [50]. Although the mechanisms responsible for the onset or maintenance of gut dysbiosis were not evaluated in this clinical cohort, it is logical to assume that dysbiosis develops secondary to the loss of autonomic control over the gastrointestinal tract. Repeat or sustained antibiotic use and psychological stress, which are common after SCI, can also exacerbate the effects of dysautonomia on the gut microbiome. This creates a feed-forward system; SCI-induced dysautonomia causes dysbiosis and impairs immune function, which, in turn, increases susceptibility to infections [2, 3, 6, 51,52,53,54,55]. High rates of infection in SCI populations increase the need for repeat dosing with antibiotics [56,57,58]. Precisely how repeat antibiotic use affects people with a SCI has not been studied, but antibiotics can disrupt bacterial gene and protein expression in the gut [59] and the composition of the gut microbiota can be changed for months or years after taking a single prescription of antibiotics [60, 61]. Thus, the conditions are ripe in both SCI animals and people for prolonged gut dysbiosis, which could adversely affect organ systems throughout the body.
Gut Dysbiosis as a Therapeutic Target After SCI
Restoring effective dialogue between the spinal cord, gut, and immune system would undoubtedly improve recovery and/or quality of life for individuals living with SCI. However, repair of the injured spinal cord is a formidable therapeutic target. Both the gut and immune system are more tractable targets and since each is affected by changes in the gut microbiota, efforts to modify postinjury gut dysbiosis could have therapeutic value. In this context, oral probiotics must be considered for use in human SCI.
Probiotics influence mucosal homeostasis by regulating intestinal microbe population dynamics, stabilizing gut epithelial barrier function, and by modulating local (GALT) and systemic immune responses [62, 63]. In patients with SCI, probiotics have been used to treat urinary tract infections and gastrointestinal distress [64, 65]. Whether probiotics can confer neuroprotection or ameliorate a range of comorbidities and neurological complications caused by a traumatic SCI has not been tested. Recently, using a mouse model of SCI, we showed that sustained postinjury delivery of VSL#3, a medical-grade probiotic, improved immune function and promoted recovery of locomotor function [41].
VSL#3 is a commercial probiotic formula comprised of 8 distinct lactic acid bacteria, primarily Lactobacillus and Bifidobacterium. These and other probiotic bacteria exert diverse effects throughout the body. In addition to their immunomodulatory effects, Lactobacillus and Bifidobacterium produce neuroactive metabolites (butyrate and other short-chain fatty acids) and neurotransmitters (serotonin, dopamine, γ-aminobutyric acid) [26, 46, 66]. These neurometabolites, produced locally in the gut, can spill over into the circulation where they can influence systemic inflammation and immune function [19, 66, 67]. These metabolites also can bypass the blood–brain barrier to affect CNS structure and function including mood, appetite, sleep, memory and learning, temperature regulation, and social behaviors [19, 66, 67]. Data from our laboratory show that SCI mice fed VSL#3 daily for 5 weeks show improvements in spontaneous locomotor recovery with reduced neuropathology [41]. Importantly, in the mesenteric lymph nodes of VSL#3-treated mice, CD4+CD25+FoxP3+ regulatory T cells (Tregs) increased significantly. Tregs, a population of T lymphocytes that express the transcription factor FoxP3, play a crucial role in immune homeostasis; Tregs actively suppress potentially damaging self-reactive (autoreactive) T cells [68]. Loss of Treg function is implicated in the onset or progression of multiple sclerosis, rheumatoid arthritis, graft versus host disease, and irritable bowel disease. Probiotics, especially those containing Lactobacillus and Bifidobacterium, significantly boost Treg activity in vivo and can ameliorate disease in multiple sclerosis models [69, 70].
Because gut microbes exert profound biological effects throughout the body, the translocation of bacteria and the development of gut dysbiosis after SCI could contribute to the various comorbidities typically attributed to paralysis or the psychological stress associated with adapting to life after SCI. Indeed, in able-bodied individuals gut dysbiosis has been linked to major depressive disorders and gastrointestinal and metabolic diseases (e.g., obesity, diabetes, Crohn’s disease, irritable bowel syndrome, etc.) (Fig. 2) [34, 46, 62, 71]. Dysbiosis and “leaky gut” also have been implicated in the onset and progression of chronic fatigue syndrome. Chronic fatigue syndrome is a multisystem disease characterized by persistent fatigue, postexertion malaise, cognitive impairment, mood changes, and gastrointestinal disturbances. Despite persistent fatigue, people with chronic fatigue syndrome often report difficulty sleeping. Many of these same symptoms also plague people with SCI [72,73,74]. In fact, fatigue affects most SCI individuals [75]. Fatigue in people with SCI is an amalgam of changes in physiological and behavioral factors including innate neuromuscular ability, motivation, resilience, and depressive-like mood swings, and is influenced by one’s overall sense of quality of life [76, 77]. As such, measures of fatigue are closely linked to social and mental health after SCI [75].
Gut dysbiosis is a disease-modifying comorbidity that likely causes or exacerbates many other comorbidities associated with spinal cord injury (SCI). Gut microbiota can directly influence immune function, neurocognitive function, and mood, metabolism, and energy/fatigue. Each of these can, in turn, influence the gut microbiota. Thus, gut dysbiosis creates a feed-forward cycle that can contribute to lasting pathophysiology, which will impair function and quality of life after SCI
SCI also enhances the risk or frequency of developing heart disease or metabolic disorders, including obesity, diabetes, and liver dysfunction [78,79,80,81,82,83,84,85]. The development of these diverse multisystem pathologies is often attributed to inactivity in people with SCI; however, changes in muscle mass and adiposity take time to develop and the onset of insulin resistance and hyperinsulinemia are not immediate consequences of SCI [86]. Similarly, cardiovascular disease and/or the consequences of chronic low-grade systemic inflammation do not manifest soon after SCI. The postinjury onset of gut dysbiosis could contribute to or cause cardiometabolic disease. After SCI in mice, the relative abundance of Bacteroidetes (order Bacteroidales) decreases as a function of time postinjury with a corresponding time-dependent increase in Firmicutes (order Clostridiales) [41]. These are the 2 major bacterial phyla that comprise both mouse and human microbiota [42, 43]. A reciprocal change in the Bacteroidetes-to-Firmicutes ratio also occurs in obese humans and rodents [87]. Gut microbiota are now believed to represent novel genetic determinants that, together with changes in diet and lifestyle, contribute to the pathophysiology of obesity [32, 88,89,90]. Precisely how obesity dysbiosis causes or exacerbates adiposity is not known; however, a high Firmicutes-to-Bacteroidetes ratio was found to increase energy harvest from the diet. Indeed, an obese microbiota is more efficient than nonobese microbiota at metabolizing and absorbing dietary substrates from food [87, 91, 92].
Each of these multiorgan “failures” develop over time and each can be linked to preceding changes in gastrointestinal dysfunction, dysbiosis, and leaky gut. Individuals with SCI also suffer from dysfunctional immune responses that exacerbate the above conditions and impair host defense, rendering individuals with SCI more susceptible to infection [2, 54, 93]. Since gut dysbiosis will affect nutrient absorption, mental health, whole-body metabolism, and systemic immune function, oral probiotics could be a “magic bullet” therapy that would simultaneously benefit various neurological and behavioral manifestations of SCI.
Future Directions and Challenges
The continuing analyses of genomic and metagenomic changes in gut microbiota will allow scientists to map the dynamic patterns of dysbiosis caused by SCI. Data from these analyses can then be used to estimate how the biological functions attributed to specific gut microbiota (e.g., metabolism of amino acids by Lactobacilli) are affected by SCI and whether these and other changes can predict the probability or severity of various SCI comorbidities including infection, anemia, obesity/metabolic syndrome, and, perhaps, secondary neurological deterioration or improvement. To date, this type of analysis in preclinical studies has been limited to fecal samples obtained from a single mouse strain affected by a moderate level of mid-thoracic SCI [41]. A similarly narrow scope of genomic analysis has been completed in fecal samples obtained from human subjects with SCI human [50].
One might predict that the magnitude of gut dysbiosis after SCI will vary as a function of injury level, injury severity, and time postinjury in both males and females after SCI. Indeed, the gut microbiota affect serotonin synthesis, metabolism, and neurotransmission in a sex-specific manner [45, 46, 94]. Also, the magnitude of innervation to the intestine by the sympathetic nervous system will vary as a function of injury severity and the spinal level affected by injury. Comparative studies of dysbiosis should also incorporate an analysis of the much less accessible small intestine microbiota [95]. The small intestine contains fewer microbiota than the large intestine, but most (~90%) energy absorption from the diet occurs in the small intestine [95, 96]. Future studies should determine whether SCI-induced changes in intestinal microbiota contribute to the high incidence of metabolic disease and increased adiposity that develop in individuals with SCI [80,81,82,83,84,85, 97,98,99]. The clinical value of considering changes in the microbiota after SCI seems obvious given that changes in the relative abundance of discrete gut microbiota (e.g., Bacteroidetes:Firmicutes) can contribute to the pathophysiology of obesity [32, 87,88,89,90,91,92]. These and other changes in the population dynamics of gut microbes represent “druggable” targets and can be manipulated in future studies using custom diets, personalized nutraceuticals (e.g., pre- or probiotics), or possibly by altering the composition of bacteriophages in the intestine that feed on pathobionts (“phage therapy”) [100, 101].
To understand how SCI-induced changes in gut microbial communities affect human physiology and pathophysiology, comparative preclinical studies are essential. In humans, it is exceedingly difficult to control the many variables that influence gut microbiota, including diet, environment, and genetics. These variables are easy to control in mice. Because mice and humans have the same core bacteria in their intestines [43, 102], mice have proven to be a productive and tractable model system for dissecting host–microbiota functional relationships. In a large multicenter study, 184 fecal samples were collected from several strains of mice housed in various laboratories around the world. A comparison of the microbiota (bacterial species) and microbiome (genes expressed by these bacteria) in these mouse samples with a human gut gene catalog revealed that the mouse and human gut microbiomes encode proteins that control nearly identical biological functions including nutrient harvest and metabolism [102]. Thus, there is remarkable conservation of function between mouse and human microbiota, making it reasonable to predict that the functional implications of large shifts in gut bacterial communities in rodent SCI models are relevant to human SCI. Still, species-specific variables do exist that can critically impact microbiota studies, many of which are driven by dietary differences between rodents and humans [103, 104]. Accordingly, researchers must remain vigilant about these (and other) differences as they design and interpret data regarding the microbiota. By doing so, the “hype” that often surrounds new microbiota research findings can be placed into context to appropriately manage the scientific and public expectations of these new data [105].
References
Espinosa-Medina I, Saha O, Boismoreau F, et al. The sacral autonomic outflow is sympathetic. Science 2016, 354:893-897.
Brommer B, Engel O, Kopp MA, et al. Spinal cord injury-induced immune deficiency syndrome enhances infection susceptibility dependent on lesion level. Brain 2016, 139:692-707.
Meisel C, Schwab JM, Prass K, Meisel A, Dirnagl U. Central nervous system injury-induced immune deficiency syndrome. Nat Rev Neurosci 2005, 6:775-786.
Rabchevsky AG. Segmental organization of spinal reflexes mediating autonomic dysreflexia after spinal cord injury. Prog Brain Res 2006, 152:265-274.
Ueno M, Ueno-Nakamura Y, Niehaus J, Popovich PG, Yoshida Y. Silencing spinal interneurons inhibits immune suppressive autonomic reflexes caused by spinal cord injury. Nat Neurosci 2016, 19:784-787.
Zhang Y, Guan Z, Reader B, et al. Autonomic dysreflexia causes chronic immune suppression after spinal cord injury. J Neurosci 2013, 33:12970-12981.
Hou S, Duale H, Cameron AA, Abshire SM, Lyttle TS, Rabchevsky AG. Plasticity of lumbosacral propriospinal neurons is associated with the development of autonomic dysreflexia after thoracic spinal cord transection. J Comp Neurol 2008, 509:382-399.
Cervi AL, Lukewich MK, Lomax AE. Neural regulation of gastrointestinal inflammation: role of the sympathetic nervous system. Auton Neurosci 2014, 182:83-88.
Elenkov IJ, Wilder RL, Chrousos GP, Vizi ES: The sympathetic nerve—an integrative interface between two supersystems: the brain and the immune system. Pharmacol Rev 2000, 52:595-638.
Mignini F, Streccioni V, Amenta F. Autonomic innervation of immune organs and neuroimmune modulation. Auton Autacoid Pharmacol 2003, 23:1-25.
Bellinger DL, Lorton D. Autonomic regulation of cellular immune function. Auton Neurosci 2014, 182:15-41.
Suzuki TA, Nachman MW. Spatial heterogeneity of gut microbial composition along the gastrointestinal tract in natural populations of house mice. PLoS ONE 2016, 11:e0163720.
Gu S, Chen D, Zhang JN, et al. Bacterial community mapping of the mouse gastrointestinal tract. PLoS ONE 2013, 8:e74957.
Donaldson GP, Lee SM, Mazmanian SK. Gut biogeography of the bacterial microbiota. Nat Rev Microbiol 2016, 14:20-32.
Hollister EB, Gao C, Versalovic J. Compositional and functional features of the gastrointestinal microbiome and their effects on human health. Gastroenterology 2014, 146:1449-1458.
Gill SR, Pop M, Deboy RT, et al. Metagenomic analysis of the human distal gut microbiome. Science 2006, 312:1355-1359.
Sender R, Fuchs S, Milo R. Revised estimates for the number of human and bacteria cells in the body. PLoS Biol 2016, 14:e1002533.
Hooper LV, Littman DR, Macpherson AJ. Interactions between the microbiota and the immune system. Science 2012, 336:1268-1273.
Yano JM, Yu K, Donaldson GP, et al. Indigenous bacteria from the gut microbiota regulate host serotonin biosynthesis. Cell 2015, 161:264-276.
Ochoa-Repáraz J, Mielcarz DW, Begum-Haque S, Kasper LH. Gut, bugs, and brain: role of commensal bacteria in the control of central nervous system disease. Ann Neurol 2011, 69:240-247.
Wang Y, Kasper LH. The role of microbiome in central nervous system disorders. Brain Behav Immun 2014, 38:1-12.
Collins SM, Surette M, Bercik P. The interplay between the intestinal microbiota and the brain. Nat Rev Microbiol 2012, 10:735-742.
Benakis C, Brea D, Caballero S, et al. Commensal microbiota affects ischemic stroke outcome by regulating intestinal γδ T cells. Nat Med 2016, 22:516-523.
Winek K, Engel O, Koduah P, et al. Depletion of cultivatable gut microbiota by broad-spectrum antibiotic pretreatment worsens outcome after murine stroke. Stroke 2016, 47:1354-1363.
Hill DA, Artis D. Intestinal bacteria and the regulation of immune cell homeostasis. Annu Rev Immunol 2010, 28:623-667.
El Aidy S, Dinan TG, Cryan JF. Gut microbiota: the conductor in the orchestra of immune-neuroendocrine communication. Clin Ther 2015, 37:954-967.
Berer K, Mues M, Koutrolos M, et al. Commensal microbiota and myelin autoantigen cooperate to trigger autoimmune demyelination. Nature 2011, 479:538-541.
Lee YK, Menezes JS, Umesaki Y, Mazmanian SK. Proinflammatory T-cell responses to gut microbiota promote experimental autoimmune encephalomyelitis. Proc Natl Acad Sci U S A 2011, 108(Suppl. 1):4615-4622.
Soyucen E, Gulcan A, Aktuglu-Zeybek AC, Onal H, Kiykim E, Aydin A: Differences in the gut microbiota of healthy children and those with type 1 diabetes. Pediatr Int 2014, 56:336-343.
Murri M, Leiva I, Gomez-Zumaquero JM, et al. Gut microbiota in children with type 1 diabetes differs from that in healthy children: a case-control study. BMC Med 2013, 11:46.
Kriegel MA, Sefik E, Hill JA, Wu HJ, Benoist C, Mathis D. Naturally transmitted segmented filamentous bacteria segregate with diabetes protection in nonobese diabetic mice. Proc Natl Acad Sci U S A 2011, 108:11548-11553.
Tilg H, Kaser A. Gut microbiome, obesity, and metabolic dysfunction. J Clin Invest 2011, 121:2126-2132.
Cao S, Feehley TJ, Nagler CR. The role of commensal bacteria in the regulation of sensitization to food allergens. FEBS Lett 2014;588:4258-4266.
Hsiao EY, McBride SW, Hsien S, et al. Microbiota modulate behavioral and physiological abnormalities associated with neurodevelopmental disorders. Cell 2013, 155:1451-1463.
de Theije CG, Wopereis H, Ramadan M, et al. Altered gut microbiota and activity in a murine model of autism spectrum disorders. Brain Behav Immun 2014, 37:197-206.
de Theije CG, Koelink PJ, Korte-Bouws GA, et al. Intestinal inflammation in a murine model of autism spectrum disorders. Brain Behav Immun 2014, 37:240-247.
Foster JA, McVey Neufeld KA. Gut-brain axis: how the microbiome influences anxiety and depression. Trends Neurosci 2013, 36:305-312.
Cryan JF, Dinan TG. Mind-altering microorganisms: the impact of the gut microbiota on brain and behaviour. Nat Rev Neurosci 2012, 13:701-712.
Rousseaux C, Thuru X, Gelot A, et al. Lactobacillus acidophilus modulates intestinal pain and induces opioid and cannabinoid receptors. Nat Med 2007, 13:35-37.
Ait-Belgnaoui A, Han W, Lamine F, et al. Lactobacillus farciminis treatment suppresses stress induced visceral hypersensitivity: a possible action through interaction with epithelial cell cytoskeleton contraction. Gut 2006, 55:1090-1094.
Kigerl KA, Hall JC, Wang L, Mo X, Yu Z, Popovich PG. Gut dysbiosis impairs recovery after spinal cord injury. J Exp Med 2016, 213:2603-2620.
Eckburg PB, Bik EM, Bernstein CN, et al. Diversity of the human intestinal microbial flora. Science 2005, 308:1635-1638.
Krych L, Hansen CH, Hansen AK, van den Berg FW, Nielsen DS. Quantitatively different, yet qualitatively alike: a meta-analysis of the mouse core gut microbiome with a view towards the human gut microbiome. PLoS ONE 2013, 8:e62578.
Castro GA, Arntzen CJ. Immunophysiology of the gut: a research frontier for integrative studies of the common mucosal immune system. Am J Phys 1993, 265:G599-610.
Clarke G, Grenham S, Scully P, et al. The microbiome-gut-brain axis during early life regulates the hippocampal serotonergic system in a sex-dependent manner. Mol Psychiatry 2013, 18:666-673.
O'Mahony SM, Clarke G, Borre YE, Dinan TG, Cryan JF. Serotonin, tryptophan metabolism and the brain-gut-microbiome axis. Behav Brain Res 2015, 277:32-48.
Balzan S, de Almeida Quadros C, de Cleva R, Zilberstein B, Cecconello I. Bacterial translocation: overview of mechanisms and clinical impact. J Gastroenterol Hepatol 2007, 22:464-471.
Khosravi A, Yáñez A, Price JG, et al. Gut microbiota promote hematopoiesis to control bacterial infection. Cell Host Microbe 2014, 15:374-381.
Mazo IB, Massberg S, von Andrian UH. Hematopoietic stem and progenitor cell trafficking. Trends Immunol 2011, 32:493-503.
Gungor B, Adiguzel E, Gursel I, Yilmaz B, Gursel M. Intestinal microbiota in patients with spinal cord injury. PLoS ONE 2016, 11:e0145878.
Lucin KM, Sanders VM, Jones TB, Malarkey WB, Popovich PG. Impaired antibody synthesis after spinal cord injury is level dependent and is due to sympathetic nervous system dysregulation. Exp Neurol 2007, 207:75-84.
Lucin KM, Sanders VM, Popovich PG. Stress hormones collaborate to induce lymphocyte apoptosis after high level spinal cord injury. J Neurochem 2009, 110:1409-1421.
Riegger T, Conrad S, Liu K, Schluesener HJ, Adibzahdeh M, Schwab JM. Spinal cord injury-induced immune depression syndrome (SCI-IDS). Eur J Neurosci 2007, 25:1743-1747.
Riegger T, Conrad S, Schluesener HJ, et al. Immune depression syndrome following human spinal cord injury (SCI): a pilot study. Neuroscience 2009, 158:1194-1199.
Oropallo MA, Held KS, Goenka R, et al. Chronic spinal cord injury impairs primary antibody responses but spares existing humoral immunity in mice. J Immunol 2012, 188:5257-5266.
Failli V, Kopp MA, Gericke C, et al. Functional neurological recovery after spinal cord injury is impaired in patients with infections. Brain 2012, 135:3238-3250.
Evans CT, Rogers TJ, Weaver FM, Burns SP. Providers’ beliefs and behaviors regarding antibiotic prescribing and antibiotic resistance in persons with spinal cord injury or disorder. J Spinal Cord Med 2011, 34:16-21.
Evans CT, Rogers TJ, Chin A, et al. Antibiotic prescribing trends in the emergency department for veterans with spinal cord injury and disorder 2002-2007. J Spinal Cord Med 2013, 36:492-498.
Pérez-Cobas AE, Gosalbes MJ, Friedrichs A, et al. Gut microbiota disturbance during antibiotic therapy: a multi-omic approach. Gut 2013, 62:1591-1601.
Francino MP. Antibiotics and the human gut microbiome: dysbioses and accumulation of resistances. Front Microbiol 2015, 6:1543.
Jernberg C, Löfmark S, Edlund C, Jansson JK. Long-term impacts of antibiotic exposure on the human intestinal microbiota. Microbiology 2010, 156:3216-3223.
Verna EC, Lucak S. Use of probiotics in gastrointestinal disorders: what to recommend? Therap Adv Gastroenterol 2010, 3:307-319.
van Baarlen P, Wells JM, Kleerebezem M. Regulation of intestinal homeostasis and immunity with probiotic lactobacilli. Trends Immunol 2013, 34:208-215.
Wong S, Jamous A, O'Driscoll J, et al. A Lactobacillus casei Shirota probiotic drink reduces antibiotic-associated diarrhoea in patients with spinal cord injuries: a randomised controlled trial. Br J Nutr 2014, 111:672-678.
Anukam KC, Hayes K, Summers K, Reid G. Probiotic Lactobacillus rhamnosus GR-1 and Lactobacillus reuteri RC-14 may help downregulate TNF-Alpha, IL-6, IL-8, IL-10 and IL-12 (p70) in the neurogenic bladder of spinal cord injured patient with urinary tract infections: a two-case study. Adv Urol 2009;680363.
Furusawa Y, Obata Y, Fukuda S, et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature 2013, 504:446-450.
Wikoff WR, Anfora AT, Liu J, et al. Metabolomics analysis reveals large effects of gut microflora on mammalian blood metabolites. Proc Natl Acad Sci U S A 2009, 106:3698-3703.
Bilate AM, Lafaille JJ. Induced CD4+Foxp3+ regulatory T cells in immune tolerance. Annu Rev Immunol 2012, 30:733-758.
Kwon HK, Kim GC, Kim Y, et al. Amelioration of experimental autoimmune encephalomyelitis by probiotic mixture is mediated by a shift in T helper cell immune response. Clin Immunol 2013, 146:217-227.
Lavasani S, Dzhambazov B, Nouri M, et al. A novel probiotic mixture exerts a therapeutic effect on experimental autoimmune encephalomyelitis mediated by IL-10 producing regulatory T cells. PLoS ONE 2010, 5:e9009.
Carding S, Verbeke K, Vipond DT, Corfe BM, Owen LJ. Dysbiosis of the gut microbiota in disease. Microb Ecol Health Dis 2015, 26:26191.
Wulff K, Gatti S, Wettstein JG, Foster RG. Sleep and circadian rhythm disruption in psychiatric and neurodegenerative disease. Nat Rev Neurosci 2010, 11:589-599.
Altindag O, Karagullu H, Gur A. Sleep disturbances in patients with spinal cord injury. Orthopedic Muscul Syst 2014, 3:164.
Jensen MP, Hirsh AT, Molton IR, Bamer AM. Sleep problems in individuals with spinal cord injury: frequency and age effects. Rehabil Psychol 2009, 54:323-331.
Jensen MP, Kuehn CM, Amtmann D, Cardenas DD. Symptom burden in persons with spinal cord injury. Arch Phys Med Rehabil 2007, 88:638-645.
Wijesuriya N, Tran Y, Middleton J, Craig A. Impact of fatigue on the health-related quality of life in persons with spinal cord injury. Arch Phys Med Rehabil 2012, 93:319-324.
Craig A, Tran Y, Wijesuriya N, Middleton J. Fatigue and tiredness in people with spinal cord injury. J Psychosom Res 2012, 73:205-210.
Bauman WA, Spungen AM. Metabolic changes in persons after spinal cord injury. Phys Med Rehabil Clin N Am 2000, 11:109-140.
Inskip J, Plunet W, Ramer L, et al. Cardiometabolic risk factors in experimental spinal cord injury. J Neurotrauma 2010, 27:275-285.
Cragg JJ, Noonan VK, Krassioukov A, Borisoff J. Cardiovascular disease and spinal cord injury: results from a national population health survey. Neurology 2013, 81:723-728.
Cragg JJ, Noonan VK, Dvorak M, Krassioukov A, Mancini GB, Borisoff JF. Spinal cord injury and type 2 diabetes: results from a population health survey. Neurology 2013, 81:1864-1868.
Wahman K, Nash MS, Westgren N, Lewis JE, Seiger A, Levi R. Cardiovascular disease risk factors in persons with paraplegia: the Stockholm spinal cord injury study. J Rehabil Med 2010, 42:272-278.
Nash MS, Tractenberg RE, Mendez AJ, et al. Cardiometabolic syndrome in people with spinal cord injury/disease: guideline-derived and nonguideline risk components in a pooled sample. Arch Phys Med Rehabil 2016, 97:1696-1705.
Gorgey AS, Mather KJ, Gater DR. Central adiposity associations to carbohydrate and lipid metabolism in individuals with complete motor spinal cord injury. Metabolism 2011, 60:843-851.
Gater DR: Obesity after spinal cord injury. Phys Med Rehabil Clin N Am 2007, 18:333-351.
Gorgey AS, Dolbow DR, Dolbow JD, Khalil RK, Castillo C, Gater DR. Effects of spinal cord injury on body composition and metabolic profile—part I. J Spinal Cord Med 2014, 37:693-702.
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI. An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 2006, 444:1027-1031.
Baothman OA, Zamzami MA, Taher I, Abubaker J, Abu-Farha M. The role of gut microbiota in the development of obesity and diabetes. Lipids Health Dis 2016, 15:108.
Ley RE: Obesity and the human microbiome. Curr Opin Gastroenterol 2010, 26:5-11.
Turnbaugh PJ, Gordon JI: The core gut microbiome, energy balance and obesity. J Physiol 2009, 587:4153-4158.
Bäckhed F, Ding H, Wang T, et al. The gut microbiota as an environmental factor that regulates fat storage. Proc Natl Acad Sci U S A 2004, 101:15718-15723.
Bäckhed F, Manchester JK, Semenkovich CF, Gordon JI. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc Natl Acad Sci U S A 2007, 104:979-984.
DeVivo MJ, Black KJ, Stover SL. Causes of death during the first 12 years after spinal cord injury. Arch Phys Med Rehabil 1993, 74:248-254.
Bolnick DI, Snowberg LK, Hirsch PE, et al. Individual diet has sex-dependent effects on vertebrate gut microbiota. Nat Commun 2014, 5:4500.
El Aidy S, van den Bogert B, Kleerebezem M. The small intestine microbiota, nutritional modulation and relevance for health. Curr Opin Biotechnol 2015, 32:14-20.
Sekirov I, Russell SL, Antunes LC, Finlay BB: Gut microbiota in health and disease. Physiol Rev 2010, 90:859-904.
Manns PJ, McCubbin JA, Williams DP. Fitness, inflammation, and the metabolic syndrome in men with paraplegia. Arch Phys Med Rehabil 2005, 86:1176-1181.
Nelson MD, Widman LM, Abresch RT, et al. Metabolic syndrome in adolescents with spinal cord dysfunction. J Spinal Cord Med 2007, 30(Suppl. 1):S127-139.
Maruyama Y, Mizuguchi M, Yaginuma T, et al. Serum leptin, abdominal obesity and the metabolic syndrome in individuals with chronic spinal cord injury. Spinal Cord 2008, 46:494-499.
Scarpellini E, Ianiro G, Attili F, Bassanelli C, De Santis A, Gasbarrini A. The human gut microbiota and virome: potential therapeutic implications. Dig Liver Dis 2015, 47:1007-1012.
Young R, Gill JJ. Microbiology. Phage therapy redux—What is to be done? Science 2015, 350:1163-1164.
Xiao L, Feng Q, Liang S, et al: A catalog of the mouse gut metagenome. Nat Biotechnol 2015, 33:1103-1108.
Winek K, Meisel A, Dirnagl U. Gut microbiota impact on stroke outcome: Fad or fact? J Cereb Blood Flow Metab 2016, 36:891-898.
Nguyen TL, Vieira-Silva S, Liston A, Raes J. How informative is the mouse for human gut microbiota research? Dis Model Mech 2015, 8:1-16.
Hanage WP: Microbiology: Microbiome science needs a healthy dose of scepticism. Nature 2014, 512:247-248.
Acknowledgments
Supported, in part, by National Institutes of Health National Institute of Neurological Disorders and Stroke NS099532 and NS083942 and the Ray W. Poppleton Endowment.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
ESM 1
(PDF 1225 kb)
Rights and permissions
About this article
Cite this article
Kigerl, K.A., Mostacada, K. & Popovich, P.G. Gut Microbiota Are Disease-Modifying Factors After Traumatic Spinal Cord Injury. Neurotherapeutics 15, 60–67 (2018). https://doi.org/10.1007/s13311-017-0583-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13311-017-0583-2