Abstract
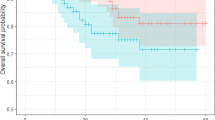
This study attempted to compare the prognostic performance of lymph node ratio (LNR) staging system with different cutoff values relative to American Joint Committee on Cancer (AJCC) pN staging system in stage III colorectal cancer (CRC). Overall, 45,069 patients from the SEER dataset and 69 patients from the Second Affiliated Hospital of Nanjing Medical University (the External set) who underwent surgical resection of the primary tumor and were diagnosed with stage III CRC by postoperative pathology were included. Patients were divided into three subgroups based on the LNR cutoff used in previous studies, Kaplan–Meier curves were plotted, and log-rank test was used to compare the differences among groups in terms of cancer-specific survival (CSS). Cox regression model was applied for survival analysis. To evaluate the discriminatory power of different lymph node staging systems, Harrell’s C statistic(C-index) and Akaike’s Information Criterion (AIC) were applied. A set of optimal cutoff values (0.11; 0.36; 0.66) of LNR staging system with the most considerable discriminatory power to the prognosis in patients with stage III CRC (SEER set: C-index = 0.714; AIC = 58,942.46, External set: C-index = 0.809; AIC = 164.36) were obtained, and both were superior to the AJCC pN staging system (SEER set: C-index = 0.708; AIC = 59,071.20, External set: C-index = 0.788; AIC = 167.06). For evaluating the prognostic efficacy of patients with stage III colorectal cancer, the cutoff value (0.11; 0.36; 0.66) of LNR staging system had the best discrimination and prognostic ability, which was superior to LNR staging system under other cutoff values and AJCC pN staging system.



Similar content being viewed by others
Data availability
The datasets used in this study are accessible to the corresponding author upon reasonable request.
Abbreviations
- CRC:
-
Colorectal cancer
- PLNs:
-
Positive lymph nodes
- ELNs:
-
Examined lymph nodes
- LNR:
-
Lymph node ratio
- AIC:
-
Akaike’s Information Criterion
- SEER:
-
The Surveillance, Epidemiology, and End Results
- C-index:
-
Harrell’s concordance index
- CSS:
-
Cancer-specific survival
- AJCC:
-
American Joint Committee on Cancer
- LODDS:
-
Log odds of positive lymph nodes
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71(3):209–249
Curtis NJ, Foster JD, Miskovic D, Brown CSB, Hewett PJ, Abbott S, Hanna GB, Stevenson ARL, Francis NK (2020) Association of surgical skill assessment with clinical outcomes in cancer surgery. JAMA Surg 155(7):590–598
Yang H, Xing J, Zhang C, Yao Z, Wu X, Jiang B, Cui M, Su X (2022) Lymph node yield less than 12 is not a poor predictor of survival in locally advanced rectal cancer after laparoscopic TME following neoadjuvant chemoradiotherapy. Front Oncol 12:1080475
Nagtegaal ID, van de Velde CJH, van der Worp E, Kapiteijn E, Quirke P, van Krieken J, Pathology Review Comm C (2002) Macroscopic evaluation of rectal cancer resection specimen: clinical significance of the pathologist in quality control. J Clin Oncol 20(7):1729–1734
Zhou ZY, Zhu H, Liu WX, Tan FB, Pei Q, Zhao LL, Li CL, Wang D, Zhou Y, Peng H et al (2021) Has the increase in the regional nodes evaluated improved survival rates for patients with locoregional colon cancer? J Cancer 12(9):2513–2525
Yang L, Xiong ZC, Xie QK, He WZ, Liu SS, Kong PF, Jiang C, Guo GF, Xia LP (2018) Prognostic value of total number of lymph nodes retrieved differs between left-sided colon cancer and right-sided colon cancer in stage III patients with colon cancer. BMC Cancer 18(1):558
Washington MK, Berlin J, Branton P, Burgart LJ, Carter DK, Fitzgibbons PL, Halling K, Frankel W, Jessup J, Kakar S et al (2009) Protocol for the examination of specimens from patients with primary carcinoma of the colon and rectum. Arch Pathol Lab Med 133(10):1539–1551
Ceelen W, Van Nieuwenhove Y, Pattyn P (2010) Prognostic value of the lymph node ratio in stage III colorectal cancer: a systematic review. Ann Surg Oncol 17(11):2847–2855
Parnaby CN, Scott NW, Ramsay G, MacKay C, Samuel L, Murray GI, Loudon MA (2015) Prognostic value of lymph node ratio and extramural vascular invasion on survival for patients undergoing curative colon cancer resection. Br J Cancer 113(2):212–219
Arrichiello G, Pirozzi M, Facchini BA, Facchini S, Paragliola F, Nacca V, Nicastro A, Canciello MA, Orlando A, Caterino M et al (2022) Beyond N staging in colorectal cancer: current approaches and future perspectives. Front Oncol 12:937114
Zhang CH, Li YY, Zhang QW, Biondi A, Fico V, Persiani R, Ni XC, Luo M (2018) The prognostic impact of the metastatic lymph nodes ratio in colorectal cancer. Front Oncol 8:628
Zanghi A, Cavallaro A, Lo Menzo E, Botta SC, Lo Bianco S, Di Vita M, Cardi F, Cappellani A (2021) Is there a relationship between length of resection and lymph-node ratio in colorectal cancer? Gastroenterol Rep 9(3):234–240
Rosenberg R, Friederichs J, Schuster T, Gertler R, Maak M, Becker K, Grebner A, Ulm K, Hofler H, Nekarda H et al (2008) Prognosis of patients with colorectal cancer is associated with lymph node ratio a single-center analysis of 3026 patients over a 25-year time period. Ann Surg 248(6):968–978
Song YX, Gao P, Wang ZN, Tong LL, Xu YY, Sun Z, Xing CZ, Xu HM (2011) which is the most suitable classification for colorectal cancer, log odds, the number or the ratio of positive lymph nodes? PLoS ONE 6(12):e28937
Lee HY, Choi HJ, Park KJ, Shin JS, Kwon HC, Roh MS, Kim C (2007) Prognostic significance of metastatic lymph node ratio in node-positive colon carcinoma. Ann Surg Oncol 14(5):1712–1717
Benson A, Venook AP, Al-Hawary MM, Cederquist L, Chen YJ, Ciombor KK, Cohen S, Cooper HS, Deming D, Engstrom PF et al (2018) Rectal cancer, version 2.2018 clinical practice guidelines in oncology. J Natl Compr Cancer Netw 16(7):874–901
Ichimasa K, Nakahara K, Kudo SE, Misawa M, Bretthauer M, Shimada S, Takehara Y, Mukai S, Kouyama Y, Miyachi H et al (2022) Novel “resect and analysis” approach for T2 colorectal cancer with use of artificial intelligence. Gastrointest Endosc 96(4):665
Miyazaki K, Wada Y, Okuno K, Murano T, Morine Y, Ikemoto T, Saito Y, Ikematsu H, Kinugasa Y, Shimada M et al (2023) An exosome-based liquid biopsy signature for pre-operative identification of lymph node metastasis in patients with pathological high-risk T1 colorectal cancer. Mol Cancer 22(1):2
Evans MD, Barton K, Rees A, Stamatakis JD, Karandikar SS (2008) The impact of surgeon and pathologist on lymph node retrieval in colorectal cancer and its impact on survival for patients with Dukes’ stage B disease. Colorectal Dis 10(2):157–164
Huang B, Chen C, Ni M, Mo S, Cai G, Cai S (2016) Log odds of positive lymph nodes is a superior prognostic indicator in stage III rectal cancer patients: a retrospective analysis of 17,632 patients in the SEER database. Int J Surg 32:24–30
Leonard D, Remue C, Abbes Orabi N, van Maanen A, Danse E, Dragean A, Debetancourt D, Humblet Y, Jouret-Mourin A, Maddalena F et al (2016) Lymph node ratio and surgical quality are strong prognostic factors of rectal cancer: results from a single referral centre. Colorectal Dis 18(6):O175-184
Lykke J, Jess P, Roikjaer O, Danish Colorectal Cancer Group (2016) The prognostic value of lymph node ratio in a national cohort of rectal cancer patients. EJSO 42(4):504–512
Wang JP, Hassett JM, Dayton MT, Kulaylat MN (2008) Lymph node ratio: role in the staging of node-positive colon cancer. Ann Surg Oncol 15(6):1600–1608
Frederique P, Stephane B, Catherine J, Alain B, Christophe P, Philippe R, Nordlinger B (2008) The ratio of metastatic to examined lymph nodes is a powerful independent prognostic factor in rectal cancer. Ann Surg 248(6):1067–1073
Calero A, Escrig-Sos J, Mingol F, Arroyo A, Martinez-Ramos D, de Juan M, Salvador-Sanchis JL, Garcia-Granero E, Calpena R, Lacueva FJ (2015) Usefulness of the log odds of positive lymph nodes to predict and discriminate prognosis in gastric carcinomas. J Gastrointest Surg 19(5):813–820
Lee CC, Ho HC, Su YC, Lee MS, Hung SK, Chen YL (2015) The prognostic ability of log odds of positive lymph nodes in oral cavity squamous cell carcinoma. Medicine 94(27):e1069
Chen LJ, Chung KP, Chang YJ, Chang YJ (2015) Ratio and log odds of positive lymph nodes in breast cancer patients with mastectomy. Surg Oncol-Oxford 24(3):239–247
Baqar AR, Wilkins S, Wang W, Oliva K, McMurrick P (2020) Log odds of positive lymph nodes is prognostically equivalent to lymph node ratio in non-metastatic colon cancer. BMC Cancer 20(1):762
Han LY, Mo SB, Xiang WQ, Li QG, Wang RJ, Xu Y, Dai WX, Cai GX (2020) Comparison of four lymph node staging systems for predicting prognosis for stage IV rectum cancer. Ann Transl Med 8(4):13
Acknowledgements
Not applicable.
Funding
The research was funded by the following grants: General Program of National Natural Science Foundation of China (No.82373293); Research project of Jiangsu Commission of Health (No. ZD2022063); The fifth phase of the "333 Project" scientific research project of Jiangsu Province (No. BRA2020091); Primary Research and Development Plan of Jiangsu Province (No. BE2019759); the National Key Research and Development Program of China (No. 2018YFE0127300).
Author information
Authors and Affiliations
Contributions
YE: data curation (lead); writing—original draft (lead); writing—review and editing (lead); visualization (lead); formal analysis (lead). CL: investigation (equal); methodology (equal); writing—original draft (equal). PJ: formal analysis (equal); methodology (equal). YH: methodology (equal); visualization (equal). XL: data curation (equal); formal analysis (equal). ZW: validation (equal); writing—review and editing (equal). CC: resources (equal); funding acquisition (equal); supervision (equal); investigation (equal); methodology (lead); writing—review and editing (lead). CY: data curation (equal); methodology (equal); validation (equal); writing—review and editing (equal). YE, CL and ZW should be considered as co-first authors. CY is the first corresponding author of this article.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
This study was reviewed and approved by the Medical Ethics Committee of the Second Affiliated Hospital of Nanjing Medical University.
Patient consent
As a retrospective study, this study did not require written informed consent from the patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
E, Y., Lu, C., Wang, Z. et al. Evaluation of the prognostic performance of different cutoff values of lymph node ratio staging system for stage III colorectal cancer. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01770-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01770-1