Abstract
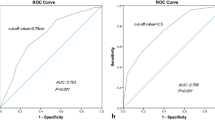
The surgical resection range of papillary thyroid microcarcinoma of the isthmus (PTMCI) is controversial, and the guidelines do not fully guide the central lymph node dissection (CLND).We retrospectively studied the comparison of PTMCI (Group A, n = 65 cases) and non-PTMCI (Group B, n = 80 cases). Based on whether central lymph node metastasis (CLNM) was further detected, they were further divided into the PTMCI with CLNM (group C, n = 42 cases), the PTMCI without CLNM (group D, n = 23 cases), the non-PTMCI with CLNM (group E, n = 45 cases), the non-PTMCI without CLNM (group F, n = 35 cases). All patients underwent total thyroidectomy and CLND. The CLNM pathological examination was divided into right recurrent laryngeal nerve superficial lymph nodes (Right VI a), right recurrent laryngeal nerve deep lymph nodes (Right VI b), left VI area lymph nodes (Left VI), prelaryngeal lymph node, and pretracheal lymph node. The extent of lymph node metastasis and risk factors of PTMCI were analyzed by univariate and multivariate analysis. The ROC curve was used to calculate the maximum diameter of the tumor and the Youden index was calculated to analyze the impact of diameter on the risk factors for CLNM in PTMCI. To construct a prediction model of transfer risk of high risk factors by Nomogram, there were significant differences in prelaryngeal lymph nodes (p = 0.034) and pretracheal lymph nodes ( n = 0.035) between group A and group B, and the risk factors of lymph node metastasis were tumor invasion (p = 0.003), multifocality (p = 0.001), and the maximum tumor diameter≧6.5 mm. PTMCI is more prone to metastasis of pretracheal lymph nodes and prelaryngeal lymph nodes, and the presence of tumor invasion, multifocality, and tumor diameter≧6.5 mm are high risk factors for metastasis in PTMCI. According to the prediction model, with all risk factors the risk of cervical lymph node metastasis is up to 90%.







Similar content being viewed by others
Data availability
All data are available for further use.
Abbreviations
- PTMCI:
-
Papillary thyroid microcarcinoma of the isthmus
- PTMC:
-
Papillary thyroid microcarcinoma
- CLNM:
-
Cervical lymph node metastasis
- CLND:
-
Central lymph node dissection
- Right VI a:
-
Right recurrent laryngeal nerve superficial lymph nodes
- Right VI b:
-
Right recurrent laryngeal nerve deep lymph nodes
- Left VI:
-
Left VI area lymph nodes
- TSH:
-
Thyroid stimulating hormone
- TG:
-
Thyroglobulin
- TGAb:
-
Anti-thyroglobulin antibody
- ROC:
-
Receiver operating characteristic curve
- FNAB:
-
Fine needle aspiration biopsy
References
Chang YW, Lee HY, Kim HS et al (2018) Extent of central lymph node dissection for papillary thyroid carcinoma in the isthmus. Ann Surg Treat Res 94(5):229–234
Pontieri G, RselliPeschi UF et al (2018) Is the isthmus location an additional risk factor for indeterminate thyroid nodules? case report and review of the literature. Front Endocrinol (Lausanne) 9:750
Tam AA, Özdemir D, Çuhacı N et al (2016) Association of multifocality, tumor number, and total tumor diameter with clinicopathological features in papillary thyroid cancer. Endocrine 53(3):774–783
Lee YC, Na SY, Chung H et al (2016) Clinicopathologic characteristics and pattern of central lymph node metastasis in papillary thyroid cancer located in the isthmus. Laryngoscope 126(10):2419–2421
Cooper DS, Doherty GM, Haugen BR et al (2009) Revised American Thyroid Association management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 19(11):1167–1214
Haddad R, Bischoff L, Ball D et al (2022) Thyroid carcinoma, NCCN Clinical Practice Guidelines in oncology. J Natl Comprehens Cancer Netw. https://doi.org/10.6004/jnccn.2022.0040
Hahn SY, Han BK, Ko EY et al (2014) Ultrasound findings of papillary thyroid carcinoma originating in the isthmus: comparison with lobe-originating papillary thyroid carcinoma. AJR Am J Roentgenol 203(3):637–642
Duman G, Sariakcali B (2021) Thyroid nodules located in the lower pole have a higher risk of malignancy than located in the isthmus: a single-center experience. Int J Endocrinol 3(19):1–10
Jeon MJ, Chun SM, Lee JY et al (2019) Mutational profile of papillary thyroid microcarcinoma with extensive lymph node metastasis. Endocrine 64(1):130–138
Song CM, Lee DW, Ji YB et al (2016) Frequency and pattern of central lymph node metastasis in papillary carcinoma of the thyroid isthmus. Head Neck 38(Suppl 1):E412–E416
Shaha AR (2018) Central lymph node metastasis in papillary thyroid carcinoma. World J Surg 42(2):1–2
Karatzas T, Vasileiadis I, Kapetanakis S et al (2013) Risk factors contributing to the difference in prognosis for papillary versus micropapillary thyroid carcinoma. Am J Surg 206(4):586–593
Qian B, Hu L, Zhang S et al (2022) Comparison of clinicopathological features and prognosis of papillary thyroid carcinoma and microcarcinoma: a population-based propensity score matching analysis. Front Endocrinol (Lausanne) 13:944758
Kim SK, Park I, Woo JW et al (2016) Predictive factors for lymph node metastasis in papillary thyroid microcarcinoma. Ann Surg Oncol 23(9):2866–2873
Jin BJ, Kim MK, Ji YB et al (2015) Characteristics and significance of minimal and maximal extrathyroidal extension in papillary thyroid carcinoma. Oral Oncol 51(8):759–763
ZhuF ZhuL, Shen Y et al (2022) Differences in the clinical characteristics of papillary thyroid microcarcinoma located in the isthmus ≤5 mm and >5mm in diameter. Front Oncol 1(12):923266
Vasileiadis I, Boutzios G, Karalaki M et al (2018) Papillary thyroid carcinoma of the isthmus: total thyroidectomy or isthmusectomy? Am J Surg 216(1):135–139
Kwak JY, Kim EK, Youk JH et al (2008) Extrathyroid ex-tension of well-differentiated papillary thyroid microcar-cinoma on US. Thyroid 18(6):609–614
Yang Z, Heng Y, Lin J et al (2020) Nomogram for predicting central lymph node metastasis in papillary thyroid cancer: a retrospective cohort study of two clinical centers. Cancer Res Treat 52(4):1010–1018
Li X, Duan Y, Liu D et al (2021) Diagnostic model incorporating clinicopathological characteristics of delphian lymph node metastasis risk profiles in papillary thyroid cancer. Front Endocrinol (Lausanne) 5(25):591015
Wang J, Sun H, Gao L et al (2016) Evaluation of thyroid isthmusectomy as a potential treatment for papillary thyroid carcinoma limited to the isthmus: a clinical study of 73 patients. Head Neck 38(Suppl1):1510–1514
Xiang D, Xie L, Xu Y et al (2015) Papillary thyroid microcarcinomas located at the middle part of the middle third of the thyroid gland correlates with the presence of neck metastasis. Surgery 157(3):526–533
Gui Z, Wang Z, Xiang J, Sun W et al (2020) Comparison of outcomes following thyroid isthmusectomy, unilateral thyroid lobectomy, and total thyroidectomy in patients with papillary thyroid microcarcinoma of the thyroid isthmus: a retrospective Study at a Single Center. Med Sci Monit 22(26):e927407
Seo HW, Song CM et al (2021) Surgical outcomes and efficacy of isthmusectomy in single isthmic papillary thyroid carcinoma: a preliminary retrospective study. J Invest Surg 34(10):1129–1134
Kwon O, Lee S, Bae JS (2021) Thyroid isthmusectomy with prophylactic central compartment neck dissection is a feasible approach for papillary thyroid cancer on the isthmus. Ann Surg Oncol 28(11):6603–6612
Park HK, Harries V, McGill MR et al (2020) Isthmusectomy in selected patients with well-differentiated thyroid carcinoma. Head Neck 42(1):43–49
Nixon IJ, Palmer FL, Whitcher MM et al (2011) Thyroid isthmusectomy for well-differentiated thyroid cancer. Ann Surg Oncol 18(3):767–770
Lei JY, Zhu JQ, Li ZH et al (2016) Surgical procedures for papillary thyroid carcinoma located in the thyroid isthmus: an intention-to-treat analysis. Onco Targets Ther 1(9):5209–5216
Acknowledgements
The work was supported by Sichuan Provincial Cancer Hospital, all colleagues in department head and neck surgery, and Linjie Ma is the corresponding author, provide financial support.
Funding
No funding was received to produce this paper.
Author information
Authors and Affiliations
Contributions
Linjie Ma, M.D. master: The first author, mainly responsible for data analysis and manuscript writing.
Corresponding author
Ethics declarations
Conflicts of interest
The authors have no competing interests or funding relevant to this article to disclose.
Ethical approval
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013).
Research involving human participants and/or animals
This research involved only human participants and no animals, and was performed in accordance with the 1964 Helsinki Declaration. This study was approved by the institutional Ethics Committee of Sichuan Provincial Cancer Hospital.
Informed consent
Informed consent was obtained from all patients.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ma, L. Characteristics and risk factors of cervical lymph node metastasis in cN0 papillary thyroid microcarcinoma of the isthmus. Updates Surg (2024). https://doi.org/10.1007/s13304-024-01760-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13304-024-01760-3