Abstract
The ‘Basket-in-Catheter’ (BIC) technique facilitates basket-only laparoscopic transcystic exploration (LTCE), increasing its success rate. Using the cholangiography catheter as a sheath is easier and safer than inserting the wire basket-alone. This study evaluates its benefits in confirmed and suspected ductal stones. Retrospective analysis of prospectively collected data on patients with pre-operative or operative suspicion of bile duct stones or with positive and equivocal intraoperative cholangiographies (IOC) who had LTCE attempted using blind basket trawling, without choledochoscopy, were reviewed. The incidence and outcomes of blind basket LTCEs attempted before and after introducing the BIC technique, whether or not stones were retrieved, were analysed. Blind basket LTCE was attempted in 732 patients. Of 377 (51.5%) patients undergoing successful stone retrieval, only 62% had pre-operative clinical and radiological risk factors for ductal stones, 25% had operative risk factors and 13% had silent stones discovered on IOC. Another 355 patients (48.5%) had negative trawling, although one half had pre-operative risk factors for ductal stones and 47.6% had operative risk factors, e.g. cystic duct stones or dilatation. This cohort had equivocal cholangiography in 25.9%. Following basket trawling, repeat IOC confirmed resolution of abnormalities. As no stones were retrieved, these were not considered duct explorations. The BIC technique facilitates safe and speedy bile duct clearance when stones are confirmed, avoiding choledochotomies, without significant complications. BIC duct trawling is also beneficial in patients with suspected ductal stones, helping to resolve equivocal IOCs. It helps surgeons to acquire and consolidate ductal exploration skills.

Similar content being viewed by others

Data availability
Data is available from the corresponding author.
References
Feng Q, Huang Y, Wang K, Yuan R, Xiong X, Wu L (2016) Laparoscopic transcystic common bile duct exploration: advantages over laparoscopic choledochotomy. PLoS ONE 11:e0162885. https://doi.org/10.1371/journal.pone.0162885
Pang L, Zhang Y, Wang Y, Kong J (2018) Transcystic versus traditional laparoscopic common bile duct exploration: its advantages and a meta-analysis. Surg Endosc 32:4363–4367. https://doi.org/10.1007/s00464-018-6286-x
Chiarugi M, Galatito C, Decanini L, Puglisi A et al (2012) Laparoscopic transcystic exploration for single-stage management of common duct stones and acute cholecystitis. Surg Endosc 26:124–129. https://doi.org/10.1007/s00464-011-1837-4
Soltan HM, Ammar MS, El Balshy MA, Mahmoud ESA (2019) Laparoscopic cystic duct exploration. Menoufia Med J 32(3):1132–1135. https://doi.org/10.4103/mmj.mmj_668_16
Hanif F, Ahmed Z, Samie MA, Nassar AHM (2010) Laparoscopic transcystic bile duct exploration: the treatment of first choice for common bile duct stones. Surg Endosc 24(7):1552–1556. https://doi.org/10.1007/s00464-009-0809-4
Qandeel H, Zino S, Hanif Z, Nassar MK, Nassar AHM (2016) Basket-in-catheter access for transcystic laparoscopic bile duct exploration: technique and results. Surg Endosc 30(5):1958–1964. https://doi.org/10.1007/s00464-015-4421-5
Zhu JG, Guo W, Han W, Zhang ZT (2017) Laparoscopic transcystic common bile duct exploration in the elderly is as effective and safe as in younger patients. J Laparoendosc Adv Surg Tech A 27(1):48–52. https://doi.org/10.1089/lap.2016.0116
Czerwonko ME, Pekolj J, Uad P, Mazza O et al (2019) Laparoscopic transcystic common bile duct exploration in the emergency is as effective and safe as in elective setting. J Gastrointest Surg 23(9):1848–1855. https://doi.org/10.1007/s11605-018-4029-x
Nassar AHM, Ng HJ, Wysocki AP et al (2020) Achieving the critical view of safety in the difficult laparoscopic cholecystectomy: a prospective study of predictors of failure. Surg Endosc. https://doi.org/10.1007/s00464-020-08093-3
Mahmud S, Hamza Y, Nassar AHM (2001) The significance of cystic duct stones encountered during laparoscopic cholecystectomy. Surg Endosc 15:460–462
Nassar AHM, Nassar MK, Gil IC et al (2020) One-session laparoscopic management of Mirizzi syndrome: feasible and safe in specialist units. Surg Endosc. https://doi.org/10.1007/s00464-020-07765-4
Lei J, Wang J, Li Q, Wu P et al (2016) Laparoscopic transcystic common bile duct exploration: T-shaped incision of cystic duct with FREDDY laser lithotripsy. J Laparoendosc Adv Surg Tech A 26(8):646–651. https://doi.org/10.1089/lap.2016.0004
Jones T, Al Musawi J, Navaratne L, Martinez-Isla A (2019) Holmium laser lithotripsy improves the rate of successful transcystic laparoscopic common bile duct exploration. Langenbeck’s Arch Surg 404(8):985–992. https://doi.org/10.1007/s00423-019-01845-3
Aawsaj Y, Ibrahim I, Gilliam A (2019) Technique for laparoscopic common bile duct exploration using disposable bronchoscope. Ann R Coll Surg Engl 101(1):69–70. https://doi.org/10.1308/rcsann.2018.0125
Yang XB, Xu AS, Li JG, Xu YP et al (2020) Dilation of the cystic duct confluence in laparoscopic common bile duct exploration and stone extraction in patients with secondary choledocholithiasis. BMC Surg. https://doi.org/10.1186/s12893-020-00705-y
Di Mauro D, Ricciardi E, Siragusa L, Manzelli A (2019) Outcome of laparoscopic common bile duct exploration after failed endoscopic retrograde cholangiopancreatography: a comparative study. J Laparoendosc Adv Surg Tech A 29(11):1391–1396. https://doi.org/10.1089/lap.2019.0383
Platt T, Smith K, Nixon M, Sinha S, Srinivas G, Andrews S (2018) Success of intraoperative imaging and management of suspected choledocholithiasis without pre-operative bile duct imaging - a case series. Ann Med Surg 36:173–177. https://doi.org/10.1016/j.amsu.2018.10.036
Matsumura T, Komatsu S, Komaya K, Fukami Y et al (2020) Dual common bile duct examination with transcystic choledochoscopy and cholangiography in laparoscopic cholecystectomy for suspected choledocholithiasis: a prospective study. Surg Endosc. https://doi.org/10.1007/s00464-020-07779-y
Czerwonko ME, Pekolj J, Uad P, Mazza O et al (2018) Acute pancreatitis after laparoscopic transcystic common bile duct exploration: an analysis of predisposing factors in 447 patients. World J Surg 42(10):3134–3142. https://doi.org/10.1007/s00268-018-4611-0
Rajan KV, Kate V, Ananthakrishnan N, Elangovan S (2000) Role of operative flexible choledochoscopy in calculous biliary tract disease. Trop Gastroenterol 21(2):80–83
Pálf A, Bende S, Bartoki A, Szabo F et al (2002) Laparoscopic transcystic biliary calculus extraction with Dormia basket. Magy Seb 55(1):40–43
Topal B, Aerts R, Penninckx F (2007) Laparoscopic common bile duct stone clearance with flexible choledochoscopy. Surg Endosc 21(12):2317–2321. https://doi.org/10.1007/s00464-007-9577-1
Jameel M, Darmas B, Baker AL (2008) Trend towards primary closure following laparoscopic exploration of the common bile duct. Ann R Coll Surg Engl 90(1):29–35. https://doi.org/10.1308/003588408X242295
Puhalla H, Flint N, O’Rourke N (2015) Surgery for common bile duct stones–a lost surgical skill; still worthwhile in the minimally invasive century? Langenbeck’s Arch Surg 400(1):119–127. https://doi.org/10.1007/s00423-014-1254-y
Salama AF, Abd Ellatif ME, Abd Elaziz H, Magdy AS et al (2017) Preliminary experience with laparoscopic common bile duct exploration. BMC Surg 17(1):32. https://doi.org/10.1186/s12893-017-0225-y
ElGhamry EE, ElSheikh M, Abdelhady H, Hablus MA, Abdelhamid AF, Soliman H, Nassar A (2019) An auspicious experience with laparoscopic common bile duct exploration. Egypt J Surg 38(3):459–470
Rhodes M, Nathanson L, O’Rourke N, Fielding G (1995) Laparoscopic exploration of the common bile duct: lessons learned from 129 consecutive cases. Br J Surg 82(5):666–668. https://doi.org/10.1002/bjs.1800820533
Sherif TM, Sarhan AEA, Abdel-Elaziz A (2016) Total laparoscopic versus endolaparoscopic common bile duct stone extraction and cholecystectomy. Egypt J Surg 35(4):311–320. https://doi.org/10.4103/1110-1121.194727
Kelley WEJ, Sheridan VC (1995) Laparoscopic choledochoscopy with a small-caliber endoscope. A safe and effective technique for laparoscopic common bile duct exploration. Surg Endosc 9(3):293–296. https://doi.org/10.1007/BF00187771
Author information
Authors and Affiliations
Contributions
Study concept and design: AHMN, HQ. Acquisition of data: AHMN, HQ. Analysis and interpretation of data: HQ, KSK, SH, HA. Drafting of manuscript: HQ, AHMN, KSK, HJN. Critical revision of manuscript: AHMN, HJN, KSK. Final approval: AHMN, HQ, KSK, HJN, SH, HA.
Corresponding author
Ethics declarations
Conflict of interest
Drs. Ahmad H. M. Nassar, Haitham Qandeel, Khurram S Khan, Hwei J Ng, Ms Subreen Hasanat and Ms Haneen Ashour have no conflicts of interest or financial ties to disclose.
Research involving human participants and/or animals, and Informed consent
Informed consent was obtained from all patients throughout the period of data collection with explanation of the rationale for one-session management of bile duct stones. The management was in line with the approved hospital protocols and not contrary to the guidelines of national and international societies. Ethical approval was not required for anonymised retrospective analysis of data that was registered with local audit departments according to their requirements.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary media file 1: The potential difficulty in inserting “naked” disposable baskets into the cystic duct is resolved by using the BIC technique, allowing the basket to reach the common bile duct. Supplementary file1 (MOV 31228 KB)
Supplementary media file 2: The basket in catheter technique allows the trawling of the common bile duct and extraction of stones. A grasper is used to prevent stones from travelling into the common hepatic duct. As the basket emerges from the cystic duct opening the introducer tip is advanced to control the stones as they are removed. Supplementary file2 (MOV 51039 KB)
13304_2023_1610_MOESM4_ESM.tiff
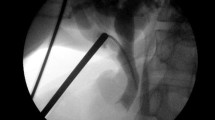
Supplementary Figure 1 B: Transcystic exploration, stone engaged in basket under X Ray control prior to removal. Supplementary file4 (TIFF 1646 KB)
13304_2023_1610_MOESM5_ESM.tiff
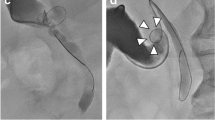
Supplementary Figure 2: Cholangiography showing two stones in the intramural cystic duct. Low medial entery of the cystic duct indicates exploration under choledochoscopic vision rather than blind basket exploration. Supplementary file5 (TIFF 2085 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nassar, A.H.M., Qandeel, H., Khan, K.S. et al. The “Basket-in-Catheter” technique: facilitating transcystic bile duct exploration and optimising the management of suspected ductal stones. Updates Surg 75, 1893–1902 (2023). https://doi.org/10.1007/s13304-023-01610-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01610-8