Abstract
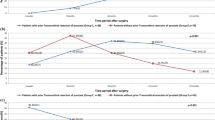
The aim of this study is to compare the functional, oncological, and complication outcomes of perineoscopic radical prostatectomy (PeRP) and robot-assisted radical prostatectomy (RARP) operations. Patients who underwent radical prostatectomy (RP) between October 2018 and June 2020 for localized prostate cancer (N0, < T3) were retrospectively screened. After the exclusion criteria, 56 patients who underwent PeRP and 67 patients who underwent RARP remained in the study. Demographic, perioperative, and postoperative data were collected. In functional outcomes, continence and potency status were compared at 1, 3, 6, and 12 months. The mean age of the patients was 61.3 ± 5.9 years in the PeRP group and 62.2 ± 5.7 years in the RARP group. No statistically significant differences were present between preoperative and postoperative values. Among the perioperative findings, the mean operation time was 90.4 ± 11.2 min for the PeRP group and 114.6 ± 14.7 min for the RARP group. The operation time was shorter in the PeRP group. The average hospital stay was 2 ± 0.6 days in the PeRP group and 2.3 ± 0.5 days in the RARP group. It was significantly shorter in the PeRP group. There is no statistically significant difference between the two groups in the oncological and functional results. PeRP is a surgical procedure safe in low-risk patients with medium-risk prostate cancer (PCa) who do not require lymph-node dissection. Moreover, PeRP minimizes the difficulties of perineal surgery.




Similar content being viewed by others
Data availability
All materials are available upon request.
References
Rawla P (2019) Epidemiology of prostatecancer. World J Oncol 10(2):63–89. https://doi.org/10.14740/wjon1191PubMedGoogleScholar
CancerResearch UK. Prostate cancer statistics. 2021. Accessed 29 Jul 2021. https://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/prostate-cancer#heading-Zero
Coughlin GD, Yaxley JW, Chambers SK et al (2018) Robot-assisted laparoscopic prostatectomy versus open radical retropubic prostatectomy: 24-month outcomes from a randomized controlled study. Lancet Oncol 19(8):1051–1060. https://doi.org/10.1016/S1470-2045(18)30357-7. (PubMed Google Scholar)
Wilt TJ, Vo TN, Langsetmo L, Dahm P, Wheeler T, Aronson WJ et al (2020) Radical prostatectomy or observation for clinically localized prostate cancer: extended follow-up of the prostate cancer intervention versus observation trial (PIVOT). Eur Urol 77(6):713–724
Bianco FJ Jr, Scardino PT, Eastham JA (2005) Radical prostatectomy: long-term cancer control and recovery of sexual and urinary function (“trifecta”). Urology 66(5 Suppl):83–94
Patel VR, Sivaraman A, Coelho RF, Chauhan S, Palmer KJ, Orvieto MA et al (2011) Pentafecta: a new concept for reporting outcomes of robot-assisted laparoscopic radical prostatectomy. Eur Urol 59(5):702–707
Basiri A, de la Rosette JJ, Tabatabaei S, Woo HH, Laguna MP, Shemshaki H (2018) Comparison of retropubic, laparoscopic and robotic radical prostatectomy: who is the winner? World J Urol 36(4):609–621
Zhang B, Zhou J, Wu S, Guo M, Zhang Y, Liu R (2020) The impact of surgical margin status on prostate cancer-specific mortality after radical prostatectomy: a systematic review and meta-analysis. Clin Transl Oncol 22(11):2087–2096
Song W, Park JH, Jeon HG, Jeong BC, Seo SI, Jeon SS et al (2017) Comparison of oncologic outcomes and complications according to surgical approach to radical prostatectomy: special focus on the perineal approach. Clin Genitourin Cancer 15(4):e645–e652
Tuğcu V, Ekşi M, Sahin S, Çolakoğlu Y, Simsek A, Evren İ et al (2020) Robot-assisted radical perineal prostatectomy: a review of 95 cases. BJU Int 125(4):573–578
Harris MJ (2003) Radical perineal prostatectomy: cost efficient, outcome effective, minimally invasive prostate cancer management. Eur Urol 44(3):303–308
Tuğcu V, Akça O, Şimşek A, Yiğitbaşı İ, Şahin S, Taşçı Aİ (2017) Robot-assisted radical perineal prostatectomy: first experience of 15 cases. Turk J Urol 43(4):476–483. https://doi.org/10.5152/tud.2017.35488. (Epub 2017 Dec 1. PMID: 29201511; PMCID: PMC5687211)
Taşçı Aİ, Şimşek A, Şam E, Şeker KG, Atar FA, Şahin S (2019) Perineoscopic radical prostatectomy: a novel surgical technique for the treatment of prostate cancer. Turk J Urol 46(1):31–36. https://doi.org/10.5152/tud.2019.19052. (PMID:31658015; PMCID:PMC6944416)
Patel VR, Tully AS, Holmes R et al (2005) Robotic radical prostatectomy in the community setting the learning curve and beyond: initial 200 cases. J Urol 174:269
Eliya F, Kernen K, Gonzalez J, Peters K, Ibrahim I, Petzel K (2011) Radical perineal prostatectomy: a learning curve? Int Urol Nephrol 43(1):139–142. https://doi.org/10.1007/s11255-010-9781-0. (Epub 2010 Sep 30 PMID: 20882343)
Jo JK, Jeong SJ, Oh JJ, Lee SW, Lee S, Hong SK et al (2018) Effect of starting penile rehabilitation with sildenafil immediately after robot-assisted laparoscopic radical prostatectomy on erectile function recovery: a prospective randomized trial. J Urol 199(6):1600–1606
Horuz R, Göktaş C, Çetinel CA, Akca O, Canguven O, Sahin C et al (2013) Simple preoperative parameters to assess technical difficulty during a radical perineal prostatectomy. Int Urol Nephrol 45(1):129–133
Kaouk JH, Akca O, Zargar H, Caputo P, Ramirez D, Andrade H et al (2016) Descriptive technique and initial results for robotic radical perineal prostatectomy. Urology 94:129–138
Heaton JP (1994) Video-assisted perineal and open surgery. J Urol 152(3):923
Resnick MI (2003) Radical perineal prostatectomy. BJU Int 92(6):522–523
Novara G, Ficarra V, Rosen RC, Artibani W, Costello A, Eastham JA et al (2012) Systematic review and meta-analysis of perioperative outcomes and complications after robot-assisted radical prostatectomy. Eur Urol 62(3):431–452
Alibhai SM, Leach M, Tomlinson G, Krahn MD, Fleshner N, Holowaty E et al (2005) 30-day mortality and major complications after radical prostatectomy: influence of age and comorbidity. J Natl Cancer Inst 97(20):1525–1532
Gillitzer R, Thomas C, Wiesner C, Jones J, Schmidt F, Hampel C et al (2010) Single center comparison of anastomotic strictures after radical perineal and radical retropubic prostatectomy. Urology 76(2):417–422
Branche B, Crocerossa F, Carbonara U, Klausner AP, Roseman JT, Hampton LJ et al (2021) Management of bladder neck contracture in the age of robotic prostatectomy: an evidence-based guide. Eur Urol Focus S2405–4569(21):00008
Wroński S (2012) Radical perineal prostatectomy—the contemporary resurgence of a genuinely minimally invasive procedure: procedure outline. Comparison of the advantages, disadvantages, and outcomes of different surgical techniques of treating organ-confined prostate cancer (PCa). A literature review with special focus on perineal prostatectomy. Cent European J Urol 65(4):188–194
Yablon CM, Banner MP, Ramchandani P, Rovner ES (2004) Complications of prostate cancer treatment: spectrum of imaging findings. Radiographics 24(Suppl 1):181–194
Amorim GL, Cruz GM, Veloso DF, Kartabil JD, Vieira JC, Alves PR (2010) Comparative analysis of radical prostatectomy techniques using perineal or suprapubic approach in the treatment of localized prostate cancer. Einstein (Sao Paulo) 8(2):200–204
Prasad SM, Gu X, Lavelle R, Lipsitz SR, Hu JC (2011) Comparative effectiveness of perineal versus retropubic and minimally invasive radical prostatectomy. J Urol 185(1):111–115. https://doi.org/10.1016/j.juro.2010.08.090. (Epub 2010 Nov 12 PMID: 21074198)
Zhang L, Wu B, Zha Z, Zhao H, Jiang Y, Yuan J (2018) Positive surgical margin is associated with biochemical recurrence risk following radical prostatectomy: a meta-analysis from high-quality retrospective cohort studies. World J Surg Oncol 16(1):124
Huang X, Wang L, Zheng X, Wang X (2017) Comparison of perioperative, functional, and oncologic outcomes between standard laparoscopic and robotic-assisted radical prostatectomy: a systemic review and meta-analysis. Surg Endosc 31(3):1045–1060
Tasci AI, Simsek A, Sam E, Seker KG, Atar FA, Sahin S et al (2020) Gasless robotic perineal radical prostatectomy: experience of the first 12 cases. Arch Esp Urol 73(3):236–241 (English, Spanish. PMID: 32240115)
Badani KK, Kaul S, Menon M (2007) Evolution of robotic radical prostatectomy: assesment after 2766 procedures. Cancer 110:1951–1958
Liesenfeld L, Kron M, Gschwend JE, Herkommer K (2017) Prognostic factors for biochemical recurrence more than 10 years after radical prostatectomy. J Urol 197:143–148
Comploj E, Pycha A (2012) Experience with radical perineal prostatectomy in the treatment of localized prostate cancer. Ther Adv Urol 4(3):125–131
Menon M, Shrivastava A, Kaul S, Badani KK, Fumo M, Bhandari M et al (2007) Vattikuti institute prostatectomy: comtemporary technique and analysis of results. Eur Urol 51:648–657
Novara G, Ficarra V, D’elia C, Secco S, Cio A, Cavalleri S, Artibani W (2010) Evaluating urinary continence and preoperative predictors of urinary continence after robot assisted laparoscopic radical prostatectomy. J Urol 184(3):1028–1033
Tuğcu V, Akça O, Şimşek A, Yiğitbaşı İ, Şahin S, Yenice MG et al (2019) Robotic-assisted perineal versus transperitoneal radical prostatectomy: a matched-pair analysis. Turk J Urol 45(4):265–272
Tasci AI, Simsek A, Torer BD, Sokmen D, Sahin S, Tugcu V (2014) Fascia-sparing intrafascial nerve-sparing robot-assisted radical prostatectomy and anatomic vesicourethral anastomosis: point of technique. Arch Esp Urol 67(9):731–739
Acknowledgements
No.
Funding
The authors declared that this study has received no financial support.
Author information
Authors and Affiliations
Contributions
Conception: AIT and YA. Design: YA and AIT. Supervision: AIT, ME, and YA. Fundings: None. Materials: YA and AIT. Data collection: YA and ME. Analysis: ME and AIT. Literature review: YA and AIT. Writer: YA. Critical review: AIT, ME, and YA.
Corresponding author
Ethics declarations
Conflict of interest
No conflict of interest was declared by the authors.
Ethical approval
Ethics committee approval was received for this study from the ethics committee of Health Science University Bakırköy Dr. Sadi Konuk Training and Research Hospital.
Research involving human participants and/or animals
This article does not contain any studies with animals performed by any of the authors. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Written informed consent was obtained from patients who participated in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arikan, Y., Eksi, M. & Tasci, A.I. Comparison of oncological and functional outcomes of perineoscopic radical prostatectomy and robot-assisted radical prostatectomy. Updates Surg 75, 1027–1035 (2023). https://doi.org/10.1007/s13304-023-01453-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-023-01453-3