Abstract
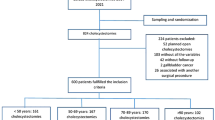
Major bile duct injuries (BDIs) may require complex surgical repairs that are usually performed with a conventional open approach. This study aims to analyze current evidence concerning the safety and the outcomes of the minimally invasive (MI) approach for biliary anastomosis in post-cholecystectomy BDIs. A systematic search of MEDLINE, Embase, and Web-Of-Science indexed studies involving MI (laparoscopic or robotic) biliary anastomosis in patients with iatrogenic BDIs was performed. The quality of the studies was assessed using the MINORS criteria. A total of 13 studies involving 198 patients were included. One hundred and twenty-five patients (63.1%) underwent a laparoscopic biliary anastomosis, while 73 (36.1%) received an analogue robotic procedure. All the included BDIs were types D and E (E1–E5). The mean OT varied between 190 and 330 (mean = 227) minutes. Ten studies reported the mean intraoperative blood loss that ranged between 50 and 252 (mean = 135.9) mL. No conversions occurred in the robotic series, while four patients required conversion to open surgery among the laparoscopic ones. The mean length of postoperative hospital stay was 6.3 days. The reported overall morbidity was similar among the robotic and laparoscopic series. During the follow‐up period, no surgery-related mortality occurred. A growing number of referral centers are showing the safety and feasibility of the MI approach for biliary anastomosis in patients with major BDIs. Further prospective comparative studies are needed to draw more definitive conclusions.



Similar content being viewed by others
References
Alexander HC, Bartlett AS, Wells CI et al (2018) Reporting of complications after laparoscopic cholecystectomy: a systematic review. HPB 20(9):786–794. https://doi.org/10.1016/j.hpb.2018.03.004
Hogan NM, Dorcaratto D, Hogan AM et al (2016) Iatrogenic common bile duct injuries: Increasing complexity in the laparoscopic era: A prospective cohort study. Int J Surg 33:151–156. https://doi.org/10.1016/j.ijsu.2016.08.004
Fletcher R, Cortina CS, Kornfield H et al (2020) Bile duct injuries: a contemporary survey of surgeon attitudes and experiences. Surg Endosc 34(7):3079–3084. https://doi.org/10.1007/s00464-019-07056-7
Strasberg SM, Hertl M, Soper NJ (1995) An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J Am Coll Surg 180(1):101–125
Schreuder AM, Busch OR, Besselink MG et al (2020) Long-term impact of iatrogenic bile duct injury. Dig Surg 37(1):10–21. https://doi.org/10.1159/000496432
Booij KAC, de Reuver PR, van Dieren S et al (2018) Long-term impact of bile duct injury on morbidity, mortality, quality of life, and work related limitations. Ann Surg 268(1):143–150. https://doi.org/10.1097/SLA.0000000000002258
Koppatz H, Sallinen V, Mäkisalo H, Nordin A (2021) Outcomes and quality of life after major bile duct injury in long-term follow-up. Surg Endosc 35(6):2879–2888. https://doi.org/10.1007/s00464-020-07726-x
Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J (2003) Methodological index for non-randomized studies ( MINORS ): development and validation of a new instrument: Methodological index for non-randomized studies. ANZ J Surg 73(9):712–716. https://doi.org/10.1046/j.1445-2197.2003.02748.x
Crema E, Silva AA, Lenza RM, de Oliveira CB, Bridi VAU, Martins A (2002) Excluded-loop hepatojejunal anastomosis with use of laparoscopy in late management of iatrogenic ligature of the bile duct. Surg Laparosc Endosc Percutan Tech 12(2):110–114. https://doi.org/10.1097/00129689-200204000-00007
Palermo M, Trelles N, Gagner M (2011) Laparoscopic revisional hepaticojejunostomy for biliary stricture after open repair following common bile duct injury: a case report. Surg Innov 18(1):105–109. https://doi.org/10.1177/1553350610395033
Prasad A (2015) Robotic assisted Roux-en-Y hepaticojejunostomy in a post-cholecystectomy type E2 bile duct injury. WJG 21(6):1703. https://doi.org/10.3748/wjg.v21.i6.1703
Ayloo S, Schwartzman J (2019) Robot-assisted repair of E1 biliary ductal injury with Roux-en-Y hepaticojejunostomy. J Laparoendosc Adv Surg Tech A 29(6):817–819. https://doi.org/10.1089/lap.2018.0664
Machado MA, Surjan RC, Ardengh AO, Makdissi F (2019) Robotic left hepatectomy and Roux-en-Y hepaticojejunostomy after bile duct injury. Ann Surg Oncol 26(9):2981–2984. https://doi.org/10.1245/s10434-019-07474-w
Goméz D, Cabrera LF, Pedraza-Ciro M, Mendoza A, Pulido J (2020) Laparoscopic Roux-en-Y hepaticojejunostomy reconstruction after iatrogenic bile duct injury: case series report. Cir Cir 88(5):608–616. https://doi.org/10.24875/CIRU.20001541
Marino MV, Mirabella A, Guarrasi D, Lupo M, Komorowski AL (2019) Robotic-assisted repair of iatrogenic common bile duct injury after laparoscopic cholecystectomy: Surgical technique and outcomes. Int J Med Robot 15(3):e1992. https://doi.org/10.1002/rcs.1992
Sucandy I, Jabbar F, Syblis C et al (2022) Robotic versus open extrahepatic biliary reconstruction for iatrogenic bile duct injury. Am Surg 88(3):345–347. https://doi.org/10.1177/00031348211047472
Kwak BJ, Choi HJ, You YK, Kim DG, Hong TH (2019) Laparoscopic end-to-end biliary reconstruction with T-tube for transected bile duct injury during laparoscopic cholecystectomy. Ann Surg Treat Res 96(6):319. https://doi.org/10.4174/astr.2019.96.6.319
Javed A, Shashikiran BD, Aravinda PS, Agarwal AK (2021) Laparoscopic versus open surgery for the management of post-cholecystectomy benign biliary strictures. Surg Endosc 35(3):1254–1263. https://doi.org/10.1007/s00464-020-07496-6
D’Hondt M, Wicherts DA (2022) Robotic biliary surgery for benign and malignant bile duct obstruction: a case series. J Robotic Surg. https://doi.org/10.1007/s11701-022-01392-y
Giulianotti PC, Quadri P, Durgam S, Bianco FM (2018) Reconstruction/repair of iatrogenic biliary injuries: is the robot offering a new option? short clinical report. Annals Surg 267(1):e7–e9. https://doi.org/10.1097/SLA.0000000000002343
Chowbey PK, Soni V, Sharma A, Khullar R, Baijal M (2005) Laparoscopic hepaticojejunostomy for biliary strictures: the experience of 10 patients. Surg Endosc 19(2):273–279. https://doi.org/10.1007/s00464-003-8288-5
Chen D, Zhu A, Zhang Z (2013) Total laparoscopic Roux-en-Y cholangiojejunostomy for the treatment of biliary disease. JSLS 17(2):178–187. https://doi.org/10.4293/108680813X13654754535232
Dokmak S, Amharar N, Aussilhou B et al (2017) Laparoscopic repair of post-cholecystectomy bile duct injury: an advance in surgical management. J Gastrointest Surg 21(8):1368–1372. https://doi.org/10.1007/s11605-017-3400-7
Cuendis-Velázquez A, Trejo-Ávila M, Bada-Yllán O et al (2019) A new era of bile duct repair: robotic-assisted versus laparoscopic hepaticojejunostomy. J Gastrointest Surg 23(3):451–459. https://doi.org/10.1007/s11605-018-4018-0
Sahoo MR, Ali MS, Sarthak S, Nayak J (2022) Laparoscopic hepaticojejunostomy for benign biliary stricture: A case series of 16 patients at a tertiary care centre in India. J Minim Access Surg 18(1):20–24. https://doi.org/10.4103/jmas.JMAS_223_20
Wang X, Yu WL, Fu XH, Zhu B, Zhao T, Zhang YJ (2020) Early versus delayed surgical repair and referral for patients with bile duct injury: a systematic review and meta-analysis. Ann Surg 271(3):449–459. https://doi.org/10.1097/SLA.0000000000003448
Perera MTPR, Silva MA, Hegab B et al (2011) Specialist early and immediate repair of post-laparoscopic cholecystectomy bile duct injuries is associated with an improved long-term outcome. Ann Surg 253(3):553–560. https://doi.org/10.1097/SLA.0b013e318208fad3
Guerra F, Coletta D, Gavioli M, Coco D, Patriti A (2020) Minimally invasive surgery for the management of major bile duct injury due to cholecystectomy. J Hepatobiliary Pancreat Sci 27(4):157–163. https://doi.org/10.1002/jhbp.710
Ismael HN, Cox S, Cooper A, Narula N, Aloia T (2017) The morbidity and mortality of hepaticojejunostomies for complex bile duct injuries: a multi-institutional analysis of risk factors and outcomes using NSQIP. HPB 19(4):352–358. https://doi.org/10.1016/j.hpb.2016.12.004
Boerma D, Rauws EAJ, Keulemans YCA et al (2001) Impaired quality of life 5 years after bile duct injury during laparoscopic cholecystectomy: a prospective analysis. Ann Surg 234(6):750–757. https://doi.org/10.1097/00000658-200112000-00006
Walsh RM, Henderson JM, Vogt DP, Brown N (2007) Long-term outcome of biliary reconstruction for bile duct injuries from laparoscopic cholecystectomies. Surgery 142(4):450–457. https://doi.org/10.1016/j.surg.2007.07.008
Pitt HA, Sherman S, Johnson MS et al (2013) Improved outcomes of bile duct injuries in the 21st century. Ann Surg 258(3):490–499. https://doi.org/10.1097/SLA.0b013e3182a1b25b
Dimou FM, Adhikari D, Mehta HB, Olino K, Riall TS, Brown KM (2016) Incidence of hepaticojejunostomy stricture after hepaticojejunostomy. Surgery 160(3):691–698. https://doi.org/10.1016/j.surg.2016.05.021
Dageforde LA, Landman MP, Feurer ID, Poulose B, Pinson CW, Moore DE (2012) A cost-effectiveness analysis of early vs late reconstruction of iatrogenic bile duct injuries. J Am Coll Surg 214(6):919–927. https://doi.org/10.1016/j.jamcollsurg.2012.01.054
Thomson BNJ, Parks RW, Madhavan KK, Wigmore SJ, Garden OJ (2006) Early specialist repair of biliary injury. Br J Surg 93(2):216–220. https://doi.org/10.1002/bjs.5194
Huang Q, Yao HH, Shao F et al (2014) Analysis of risk factors for postoperative complication of repair of bile duct injury after laparoscopic cholecystectomy. Dig Dis Sci 59(12):3085–3091. https://doi.org/10.1007/s10620-014-3255-7
Lindemann J, Jonas E, Kotze U, Krige JEJ (2020) Evolution of bile duct repair in a low and middle-income country (LMIC): a comparison of diagnosis, referral, management and outcomes in repair of bile duct injury after laparoscopic cholecystectomy from 1991 to 2004 and 2005–2017. HPB 22(3):391–397. https://doi.org/10.1016/j.hpb.2019.07.009
Krige JE (2010) Bile leaks and sepsis: drain now, fix later: comment on “bile duct injuries associated with laparoscopic cholecystectomy.” Arch Surg 145(8):763. https://doi.org/10.1001/archsurg.2010.154
Rystedt JML, Kleeff J, Salvia R et al (2019) Post cholecystectomy bile duct injury: early, intermediate or late repair with hepaticojejunostomy – an E-AHPBA multi-center study. HPB 21(12):1641–1647. https://doi.org/10.1016/j.hpb.2019.04.003
Pulitanò C, Parks RW, Ireland H, Wigmore SJ, Garden OJ (2011) Impact of concomitant arterial injury on the outcome of laparoscopic bile duct injury. Am J Surg 201(2):238–244. https://doi.org/10.1016/j.amjsurg.2009.07.038
Alves A, Farges O, Nicolet J, Watrin T, Sauvanet A, Belghiti J (2003) Incidence and consequence of an hepatic artery injury in patients with postcholecystectomy bile duct strictures. Ann Surg 238(1):93–96. https://doi.org/10.1097/01.sla.0000074983.39297.c5
Strasberg SM, Helton WS (2011) An analytical review of vasculobiliary injury in laparoscopic and open cholecystectomy. HPB 13(1):1–14. https://doi.org/10.1111/j.1477-2574.2010.00225.x
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
Each individual listed as an author on this article contributed substantially and in accordance with the guidelines of the International Committee of Medical Journal Editors.
Corresponding author
Ethics declarations
Conflict of interests
AC, NHD, GC and FP have no conflict of interest or financial ties to disclose. FMB has an educational agreement with Asensus, Intuitive, and Medtronic.
Ethical standards
Research involving human participants and/or animals.
This research did not involve human participants and/or animals, since it is a secondary research.
Informed consent
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cubisino, A., Dreifuss, N.H., Cassese, G. et al. Minimally invasive biliary anastomosis after iatrogenic bile duct injury: a systematic review. Updates Surg 75, 31–39 (2023). https://doi.org/10.1007/s13304-022-01392-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-022-01392-5