Abstract
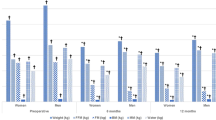
Bariatric surgery has been recognized as the most effective long-term treatment for morbid obesity. Despite the considerable positive results, adverse consequence can develop. Excessive Weight Loss (EXWL), a rare consequence of bariatric surgery, can lead to a broad adverse consequence. The aim of this study was determining of prevalence and the predicting model of EXWL in patient underwent bariatric surgery until 24 months after surgery. Data have been extracted from the National Obesity Surgery Database in obesity clinic of Iran University of Medical Sciences. The subjects of this retrospective cohort study were morbid obese individuals who underwent three various types of bariatric surgery [One Anastomosis Gastric Bypass (OAGB), Roux-en-Y Gastric Bypass (RYGB), or Sleeve Gastrectomy (SG)] in period of 24 months ago. EXWL has been defined as reaching to less than or equal to BMI 18.5 at any time until 24 months after surgery. SPSS was used in data analysis. Among 4214 subjects of this study, most excess weight loss after surgery has taken place in 18 months after surgery. 11.4% (n = 495) of patients experienced EXWL with highest percentage among OAGB patients (15.1%) at time of 24 months after surgery. The females (20.4% vs.9.9%) and younger persons (35.45 ± 10.25 vs. 39.06 ± 10.76) were more susceptible to EXWL. Patients with EXWL had significantly lower BMI (body mass index) (41.11 ± 4.51 vs. 46.73 ± 6.26) (Kg/m2), and were less probable to had emotional eating. Visceral fat level, fat percentage, and BMI were the best predictor of EXWL (P value for all < 0.05). So that per level increase in visceral fat, decreases the probability of EXWL as 47% and 61% in SG and OAGB. Moreover, each unit lower BMI leads to 25% higher susceptibility to experience EXWL. Surgery should be adjusted in younger females with a lower BMI and healthy metabolic status who are more prone to EXWL. In such a way that minimize weight loss speed/value. It may be possible by selection of other surgery procedures, rather than OAGB, tighter follow-ups, and consultations of patients after surgery is emphasized for more EXWL vulnerable patients.

Similar content being viewed by others
References
Brolin RE (2002) Bariatric surgery and long-term control of morbid obesity. JAMA 288(22):2793–2796
Shoar S, Nguyen T, Ona MA, Reddy M, Anand S, Alkuwari MJ, Saber AA (2016) Roux-en-Y gastric bypass reversal: a systematic review. Surg Obesity Related Dis 12(7):1366–1372
Karamanakos SN, Vagenas K, Kalfarentzos F, Alexandrides TK (2008) Weight loss, appetite suppression, and changes in fasting and postprandial ghrelin and peptide-YY levels after Roux-en-Y gastric bypass and sleeve gastrectomy: a prospective, double blind study. Ann Surg 247(3):401–407
Tacchino RM (2015) Bowel length: measurement, predictors, and impact on bariatric and metabolic surgery. Surg Obesity Related Dis 11(2):328–334
Hogling DE, Rydén M, Bäckdahl J, Thorell A, Arner P, Andersson DP (2018) Body fat mass and distribution as predictors of metabolic outcome and weight loss after Roux-en-Y gastric bypass. Surg Obe Related Dis 14(7):936–942
Lutfi R, Torquati A, Sekhar N, Richards W (2006) Predictors of success after laparoscopic gastric bypass: a multivariate analysis of socioeconomic factors. Surg Endosc Other Interv Tech 20(6):864–867
Major P, Wysocki M, Janik M, Stefura T, Walędziak M, Pędziwiatr M, Kowalewski P, Paśnik K, Budzyński A (2018) Impact of age on postoperative outcomes in bariatric surgery. Acta Chir Belg 118(5):307–314
Vázquez-Velázquez V, González AR, Ortega SO, Flores MR, Herrera MF, Pantoja JP, Sierra M, Prida CG-J, García JEG (2018) Differences in body composition in patients with obesity 1 year after roux-en-Y gastric bypass: Successful vs. unsuccessful weight loss, Obes Surg 28(3): 864–868.
Akusoba I, Birriel TJ, El Chaar M (2016) Management of excessive weight loss following laparoscopic Roux-en-Y gastric bypass: clinical algorithm and surgical techniques. Obes Surg 26(1):5–11
Martins TdCP, Duarte TC, Mosca ERT, de Fátima Pinheiro C, Marçola MA, De-Souza DA (2015) Severe protein malnutrition in a morbidly obese patient after bariatric surgery, Nutrition 31(3) 535–538.
Pucci A, Cheung WH, Jones J, Manning S, Kingett H, Adamo M, Elkalaawy M, Jenkinson A, Finer N, Doyle J (2015) A case of severe anorexia, excessive weight loss and high peptide-YY levels after sleeve gastrectomy, Endocrinology, diabetes & metabolism case reports 2015(1).
Hung K-C, Ho C-N, Chen J-Y, Liu W-C, Sun C-K, Soong T-C (2019) Association of preoperative hemoglobin with weight loss after bariatric surgery: a retrospective study. Surg Obes Related Dis 15(9):1595–1603
Schaaf C, Gugenheim J (2017) Impact of preoperative serum vitamin D level on postoperative complications and excess weight loss after gastric bypass. Obes Surg 27(8):1982–1985
Brethauer SA, Kim J, el Chaar M, Papasavas P, Eisenberg D, Rogers A, Ballem N, Kligman M, Kothari S (2015) Standardized outcomes reporting in metabolic and bariatric surgery. Surg Obes Related Dis 11(3):489–506
Martins TdCP, Duarte TC, Mosca ERT, Pinheiro CdF, Marçola MA, De-Souza DA (2015) Severe protein malnutrition in a morbidly obese patient after bariatric surgery, Nutrition 31(3): 535–538.
Zurita Mv LC, Tabari M, Hong D (2013) Laparoscopic conversion of laparoscopic Roux-en-Y gastric bypass to laparoscopic sleeve gastrectomy for intractable dumping syndrome and excessive weight loss, Surg Obes Related Dis 9(2): e34–7.
Mohapatra S, Gangadharan K, Pitchumoni CS (2020) Malnutrition in obesity before and after bariatric surgery. Dis Mon 66(2):100866
Kuin C, den Ouden F, Brandts H, Deden L, Hazebroek E, van Borren M, de Boer H (2019) Treatment of severe protein malnutrition after bariatric surgery. Obes Surg 29(10):3095–3102
Lee Y-C, Lee Y-H, Chuang P-N, Kuo C-S, Lu C-W, Yang K-C (2020) The utility of visceral fat level measured by bioelectrical impedance analysis in predicting metabolic syndrome. Obes Res Clin Pract 14(6):519–523
Dhana K, Koolhaas CM, Schoufour JD, Rivadeneira F, Hofman A, Kavousi M, Franco OH (2016) Association of anthropometric measures with fat and fat-free mass in the elderly: the Rotterdam study. Maturitas 88:96–100
Neto MG, Moon RC, de Quadros LG, Grecco E, Filho AC, de Souza TF, Mattar LA, de Sousa JAG, Dayyeh BKA, Morais H, Matz F, Jawad MA, Teixeira AF Safety and short-term effectiveness of endoscopic sleeve gastroplasty using overstitch: preliminary report from a multicenter study, Surgical endoscopy (2019).
Hoyas I, Leon-Sanz M (2019) Nutritional challenges in metabolic syndrome, J Clin Med 8(9).
Beaudry KM, Devries MC (2019) Nutritional strategies to combat type 2 diabetes in aging adults: the importance of protein, Front Nutr 6(138).
Hubert PA, Papasavas P, Stone A, Swede H, Huedo-Medina TB, Tishler D, Duffy VB (2019) Associations between weight loss, food likes, dietary behaviors, and chemosensory function in bariatric surgery: a case-control analysis in women. Nutrients 11(4):804
Preiss K, Clarke D, O'Brien P, de la Piedad Garcia X, Hindle A, Brennan L (2018) Psychosocial predictors of change in depressive symptoms following gastric banding surgery, Obes Surg 28(6): 1578–1586.
Susmallian S, Nikiforova I, Azoulai S, Barnea R (2019) Outcomes of bariatric surgery in patients with depression disorders. PLoS ONE 14(8):e0221576
Backman O, Stockeld D, Rasmussen F, Naslund E, Marsk R (2016) Alcohol and substance abuse, depression and suicide attempts after Roux-en-Y gastric bypass surgery. Br J Surg 103(10):1336–1342
Ng WL, Peeters A, Naslund I, Ottosson J, Johansson K, Marcus C, Shaw JE, Bruze G, Sundstrom J, Neovius M (2017) Change in use of sleep medications after gastric bypass surgery or intensive lifestyle treatment in adults with obesity, Obesity (Silver Spring, Md.) 25(8): 1451–1459.
Dixon JB (2016) Self-harm and suicide after bariatric surgery: time for action. Lancet Diabetes Endocrinol 4(3):199–200
Toolabi K, Sarkardeh M, Vasigh M, Golzarand M, Vezvaei P, Kooshki J Comparison of laparoscopic Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy on weight loss, weight regain, and remission of comorbidities: a 5 years of follow-up study, Obes Surg (2019).
. Kavanagh R, Smith J, Avgenackis E, Jones D, Nau P (2019). A Comparison of the effects of roux-en-Y gastric bypass and sleeve gastrectomy on body mass composition as measured by air displacement plethysmography, Obes Surg.
Antoniewicz A, Kalinowski P, Kotulecka KJ, Kocon P, Paluszkiewicz R, Remiszewski P, Zieniewicz K (2019) Nutritional deficiencies in patients after roux-en-Y gastric bypass and sleeve gastrectomy during 12-month follow-up. Obes Surg 29(10):3277–3284
Ahmed B, King WC, Gourash W, Hinerman A, Belle SH, Pomp A, Pories WJ, Courcoulas AP (2019) Proximal Roux-en-Y gastric bypass: addressing the myth of limb length. Surgery 166(4):445–455
Kermansaravi M, Pishgahroudsari M, Kabir A, Abdolhosseini MR, Pazouki A (2020) Weight loss after one-anastomosis/mini-gastric bypass—The impact of biliopancreatic limb: a retrospective cohort study. J Res Med Sci 25:5–5
Rutledge R (2017) Linear Association of Limb Length and Weight Loss in 3,309 Mini-gastric Bypass Patients. https://www.sages.org/meetings/annual-meeting/abstracts-archive/linear-association-of-limb-length-and-weight-loss-in-3309-mini-gastric-bypass-patients/. April 23.
Lee W-J, Wang W, Lee Y-C et al. (2008) Laparoscopic mini-gastric bypass: experience with tailored bypass limb according to body weight, Obes Surg 18: 294–299.
Chen J-C, Shen C-Y, Lee W-J, Tsai P-L, Lee Y-C (2019) Protein deficiency after gastric bypass: the role of common limb length in revision surgery. Surg Obes Related Dis 15(3):441–446
Khalaj A, Kalantar Motamedi MA, Mousapour P, Valizadeh M, Barzin M (2019) Protein-calorie malnutrition requiring revisional surgery after one-anastomosis-mini-gastric bypass (OAGB-MGB): case series from the tehran obesity treatment study (TOTS), Obesity Surgery 29(6): 1714–1720.
Parikh M, Gagner M, Heacock L, Strain G, Dakin G, Pomp A (2008) Laparoscopic sleeve gastrectomy: does bougie size affect mean %EWL? Short-term Outcomes Surg Obes Related Dis 4(4):528–533
Cottam S, Cottam D, Cottam A (2019) Sleeve gastrectomy weight loss and the preoperative and postoperative predictors: a systematic review. Obes Surg 29(4):1388–1396
Reinecke H, Trey T, Wellmann J, Heidrich J, Fobker M, Wichter T, Walter M, Breithardt G, Schaefer RM (2003) Haemoglobin-related mortality in patients undergoing percutaneous coronary interventions. Eur Heart J 24(23):2142–2150
Kucuk N, Orbak Z, Karakelloglu C, Akcay F (2019) The effect of therapy on plasma ghrelin and leptin levels, and appetite in children with iron deficiency anemia. J Pediatric Endocrinol Metab 32(3):275–280
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared no conflicts of interest regarding the publication of the present article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hatami, M., Pazouki, A. & Kabir, A. Excessive weight loss after bariatric surgery: a prediction model retrospective cohort study. Updates Surg 74, 1399–1411 (2022). https://doi.org/10.1007/s13304-022-01319-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-022-01319-0