Abstract
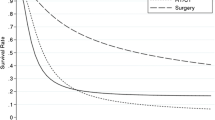
According to international guidelines, surgical treatment is not recommended for gallbladder adenocarcinoma with liver metastases (GCL), and research on the clinical implications of surgery in GCL is very scarce. In this study, we aimed to investigate whether surgery is an effective means to improve survival in GCL. Data were collected from the Surveillance, Epidemiology, and End Results database. A total of 612 people diagnosed with GCL were identified. According to their treatment, patients were categorised into 4 groups: synchronous resection of the primary tumour and liver metastases (SPL), synchronous primary site and other resection (SPO), single resection of the primary site (SPS), and no resection (NR). Our study findings showed that 34 (5.6%) patients received SPL, 18 (2.9%) had SPO, 185 (30.2%) underwent SPS, and 375 (61.3%) received NR. Our analysis showed that surgical treatment was an independent protective prognostic factor for gallbladder cancer cause-specific survival. Groups who underwent SPL, SPO, and SPS showed gradually decreasing survival benefit compared with the NR group (median survival: 9, 5, 4, and 2 months, respectively). Notably, mortality in the SPL, SPO, and SPS groups were significantly different compared with NR group, and the hazard ratio were gradually increased, which were 0.402 (95% confidence interval [CI] 0.264–0.611), 0.463 (95% CI 0.274–0.784), and 0.597 (95% CI 0.457–0.779), respectively (all P < 0.05). Survival in patients with GCL was significantly improved via surgery of the primary site with simultaneous metastasectomy. Among them, SPL and SPO showed greater survival advantages in carefully selected patients with GCL. Registered at researchregistery.com: Trial registration number is researchregistry6915.

Similar content being viewed by others
Availability of data and materials
The data that support the findings of this study are openly available in National Cancer Institute's Surveillance Epidemiology and End Result SEER at https://seer.cancer.gov/.
References
Miller G, Jarnagin WR (2008) Gallbladder carcinoma. Eur J Surg Oncol 34:306–312. https://doi.org/10.1016/j.ejso.2007.07.206
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424. https://doi.org/10.3322/caac.21492
Kokudo N, Makuuchi M, Natori T et al (2003) Strategies for surgical treatment of gallbladder carcinoma based on information available before resection. Arch Surg 138:741–750. https://doi.org/10.1001/archsurg.138.7.741
Ohtani T, Shirai Y, Tsukada K et al (1996) Spread of gallbladder carcinoma: CT evaluation with pathologic correlation. Abdom Imaging 21:195–201. https://doi.org/10.1007/s002619900045
Sakamoto Y, Kosuge T, Shimada K et al (2006) Clinical significance of extrahepatic bile duct resection for advanced gallbladder cancer. J Surg Oncol 94:298–306. https://doi.org/10.1002/jso.20585
Taner CB, Nagorney DM, Donohue JH (2004) Surgical treatment of gallbladder cancer. J Gastrointest Surg 8:83–89. https://doi.org/10.1016/j.gassur.2003.09.022
Levy AD, Murakata LA, Rohrmann CA (2001) Gallbladder carcinoma: radiologic-pathologic correlation. Radiographics 21:295–314. https://doi.org/10.1148/radiographics.21.2.g01mr16295
Dixon E, Vollmer CM, Sahajpal A et al (2005) An aggressive surgical approach leads to improved survival in patients with gallbladder cancer: a 12-year study at a North American Center. Ann Surg 241:385–394. https://doi.org/10.1097/01.sla.0000154118.07704.ef
Neron M, Sajous C, Thezenas S et al (2020) Impact of metastasis surgery and alkylating-agent-based chemotherapy on outcomes of metastatic malignant phyllodes tumors: a multicenter retrospective study. Ann Surg Oncol 27:1693–1699. https://doi.org/10.1245/s10434-019-08097-x
Testori AAE, Blankenstein SA, van Akkooi ACJ (2019) Surgery for metastatic melanoma: an evolving concept. Curr Oncol Rep 21:98. https://doi.org/10.1007/s11912-019-0847-6
Alpantaki K, Ioannidis A, Raptis K et al (2020) Surgery for spinal metastatic tumors: prognostication systems in clinical practice (Review). Mol Clin Oncol 12:399–402. https://doi.org/10.3892/mco.2020.2008
Concors SJ, Sinnamon AJ, Ecker BL et al (2020) The impact of surgery for metastatic pancreatic neuroendocrine tumor: a contemporary evaluation matching for chromogranin a level. HPB (Oxford) 22:83–90. https://doi.org/10.1016/j.hpb.2019.05.011
Stein A, Bokemeyer C (2014) How to select the optimal treatment for first line metastatic colorectal cancer. World J Gastroenterol 20:899–907. https://doi.org/10.3748/wjg.v20.i4.899
Fong Y, Jarnagin W, Blumgart LH (2000) Gallbladder cancer: comparison of patients presenting initially for definitive operation with those presenting after prior noncurative intervention. Ann Surg 232:557–569. https://doi.org/10.1097/00000658-200010000-00011
National Comprehensive Cancer Network (2019) NCCN Clinical Practice Guidelines in Oncology. Hepatobiliary Cancers Version 2.
Wistuba II, Gazdar AF (2004) Gallbladder cancer: lessons from a rare tumour. Nat Rev Cancer 4:695–706. https://doi.org/10.1038/nrc1429
Park JO, Oh DY, Hsu C et al (2015) Gemcitabine plus cisplatin for advanced biliary tract cancer: a systematic review. Cancer Res Treat 47:343–361. https://doi.org/10.4143/crt.2014.308
Wang J, Narang AK, Sugar EA et al (2015) Evaluation of adjuvant radiation therapy for resected gallbladder carcinoma: a multi-institutional experience. Ann Surg Oncol. https://doi.org/10.1245/s10434-015-4685-y
Doval DC, Sekhon JS, Gupta SK et al (2004) A phase II study of gemcitabine and cisplatin in chemotherapy-naive, unresectable gall bladder cancer. Br J Cancer 90:1516–1520. https://doi.org/10.1038/sj.bjc.6601736
Qin TJ, Zhao XH, Yun J et al (2008) Efficacy and safety of gemcitabine-oxaliplatin combined with huachansu in patients with advanced gallbladder carcinoma. World J Gastroenterol 14:5210–5216. https://doi.org/10.3748/wjg.14.5210
Chijiiwa K, Kai M, Nagano M et al (2007) Outcome of radical surgery for stage IV gallbladder carcinoma. J Hepatobiliary Pancreat Surg 14:345–350. https://doi.org/10.1007/s00534-006-1186-1
Nakamura S, Sakaguchi S, Suzuki S et al (1989) Aggressive surgery for carcinoma of the gallbladder. Surgery 106:467–473
Wg X, Peng CH, Zhou GW et al (2005) Surgical treatment for Nevin stage IV and V gallbladder carcinoma: report of 70 cases. Hepatobiliary Pancreat Dis Int 4:589–592
Geng ZM, Cai ZQ, Zhang Z et al (2019) Estimating survival benefit of adjuvant therapy based on a Bayesian network prediction model in curatively resected advanced gallbladder adenocarcinoma. World J Gastroenterol 25:5655–5666. https://doi.org/10.3748/wjg.v25.i37.5655
Acknowledgements
The authors acknowledge the efforts of the SEER program in the creation of the SEER database
Funding
This work was supported by the National Natural Science Foundation of China Grant (No. 82173353) and the Top talent scientific research project of “six one projects” (LGY2018028).
Author information
Authors and Affiliations
Contributions
GTM: conceptualisation, data curation, supervision, and writing—original draft. TH: conceptualisation, formal analysis, writing—original draft, and supervision. ZBH: conceptualisation, formal analysis, and writing—review and editing. BDS: methodology and title page project administration. JSJ: data curation, resources, software, formal analysis, validation, and visualisation. ZC: investigation, methodology, and project administration. JGQ: conceptualisation, supervision, formal analysis, funding acquisition, and writing—review and editing.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declare no conflicts of interest.
Ethics approval statement
The SEER Program collects data from population-based cancer registries with anonymous information. The SEER is a publicly available database and data extracted from SEER was deemed “non-human study” by the North Shore LIJ IRB committee.
Informed consent
As this study is based on a publicly available database without identifying patient information, informed consent was not needed.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gao, T., Tang, H., Zhou, B. et al. Can patients with gallbladder adenocarcinoma and liver metastases obtain survival benefit from surgery? A population-based study. Updates Surg 74, 1353–1366 (2022). https://doi.org/10.1007/s13304-022-01302-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-022-01302-9