Abstract
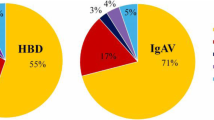
To explore the value of blood routine examination indexes in the differential diagnosis of immunoglobulin A vasculitis (IgAV) with abdominal involvement and appendicitis in children. Forty-seven patients with IgAV and abdominal involvement, 95 cases with appendicitis, and 48 healthy children were enrolled in this study. Demographic and laboratory data were retrospectively recorded from medical files. The levels of serum percentage of lymphocytes (LYM%), percentage of eosinophils (E%), red cell volume distribution width (RDW) and platelet (PLT) count were higher, while blood cells (WBC) count, percentage of neutrophils (N%), percentage of monocytes (M%), mean platelet volume (MPV), platelet distribution width and C-reactive protein were lower in the group of IgAV with abdominal involvement compared to appendicitis group (P < 0.05). Multivariate logistic regression analysis showed LYM% (odds ratio (OR) = 1.34, P = 0.001) and RDW (OR = 2.96, P = 0.045) were independent risk factors for IgAV with abdominal involvement. N% (OR = 1.270, P = 0.006) and MPV (OR = 51.15, P = 0.042) were independently associated with appendicitis. Using receiver operating characteristic analysis, the optimal cut-off values (sensitivity and specificity) respectively were 42.17% (95.7%, 100.0%) for LYM%, 12.65% (83.0%, 83.2%) for RDW, 61.5% (91.6%, 97.9%) for NE% and 10.1fL (78.9%, 75.4%) for MPV, with the AUC values of 0.989, 0.881, 0.985, 0.810, respectively. Blood routine examination indices, especially the N%, LYM%, RDW, and MPV, can be used for simple differential diagnosis of IgAV with abdominal involvement and appendicitis.

Similar content being viewed by others
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
López-Mejías R, Castañeda S, Genre F et al (2018) Genetics of immunoglobulin-A vasculitis (Henoch-Schönlein purpura): an updated review. Autoimmun Rev 17:301–315. https://doi.org/10.1016/J.AUTREV.2017.11.024
Piram M, Maldini C, Biscardi S et al (2017) Incidence of IgA vasculitis in children estimated by four-source capture-recapture analysis: a population-based study. Rheumatology (Oxford) 56:1358–1366. https://doi.org/10.1093/rheumatology/kex158
Ozen S, Pistorio A, Iusan SM et al (2010) EULAR/PRINTO/PRES criteria for Henoch-Schönlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008. Part II: Final classification criteria. Ann Rheum Dis 69:798–806. https://doi.org/10.1136/ard.2009.116657
Trapani S, Rubino C, Indolfi G (2020) Gastrointestinal involvement in childhood vasculitides. Acta Paediatr 109:2226–2236. https://doi.org/10.1111/APA.15381
Rubino C, Monacelli C, Marrani E et al (2021) Gastrointestinal involvement in IgA vasculitis: a single-center 11-year study on a cohort of 118 children. Clin Rheumatol 40:5041–5046. https://doi.org/10.1007/S10067-021-05863-9
Anderson JE, Bickler SW, Chang DC, Talamini MA (2012) Examining a common disease with unknown etiology: trends in epidemiology and surgical management of appendicitis in California, 1995–2009. World J Surg 36:2787–2794. https://doi.org/10.1007/S00268-012-1749-Z
Glerum KM, Selbst SM, Parikh PD, Zonfrillo MR (2021) Pediatric Malpractice Claims in the Emergency Department and Urgent Care Settings From 2001 to 2015. Pediatr Emerg Care 37:E376–E379. https://doi.org/10.1097/PEC.0000000000001602
Baxter KJ, Nguyen HTMH, Wulkan ML, Raval MV (2018) Association of health care utilization with rates of perforated appendicitis in children 18 years or younger. JAMA Surg 153:544–550. https://doi.org/10.1001/JAMASURG.2017.5316
Benabbas R, Hanna M, Shah J, Sinert R (2017) Diagnostic accuracy of history, physical examination, laboratory tests, and point-of-care ultrasound for pediatric acute appendicitis in the emergency department: a systematic review and meta-analysis. Acad Emerg Med Off J Soc Acad Emerg Med 24:523–551. https://doi.org/10.1111/ACEM.13181
Bhangu A, Søreide K, di Saverio S, Assarsson HJ, Drake TF (2015) Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet (London, England) 386:1278–1287. https://doi.org/10.1016/S0140-6736(15)00275-5
Choong CK, Beasley SW (1998) Intra-abdominal manifestations of Henoch-Schönlein purpura. J Paediatr Child Health 34:405–409. https://doi.org/10.1046/J.1440-1754.1998.00263.X
Karabulut R, Sonmez K, Turkyilmaz Z et al (2011) Negative appendectomy experience in children. Ir J Med Sci 180:55–58. https://doi.org/10.1007/S11845-010-0526-Y
Jaszczura M, Góra A, Grzywna-Rozenek E et al (2019) Analysis of neutrophil-to-lymphocyte ratio, platelet to lymphocyte ratio and mean platelet volume to platelet count ratio in children with acute stage of immunoglobulin A vasculitis and assessment of their suitability for predicting the course of the disease. Rheumatol Int 39:869–878. https://doi.org/10.1007/S00296-019-04274-Z
Peksöz R, Bayar B (2021) The role of complete blood count parameters in diagnosing acute appendicitis and measuring the severity of inflammation. Ulus Travma Acil Cerrahi Derg 27:654–661. https://doi.org/10.14744/TJTES.2020.69195
Hajibandeh S, Hajibandeh S, Hobbs N, Mansour M (2020) Neutrophil-to-lymphocyte ratio predicts acute appendicitis and distinguishes between complicated and uncomplicated appendicitis: A systematic review and meta-analysis. Am J Surg 219:154–163. https://doi.org/10.1016/J.AMJSURG.2019.04.018
Dayawansa NH, Segan JDS, Yao HHI et al (2018) Incidence of normal white cell count and C-reactive protein in adults with acute appendicitis. ANZ J Surg 88:E539–E543. https://doi.org/10.1111/ANS.13760
Karadağ ŞG, Çakmak F, Çil B et al (2021) The relevance of practical laboratory markers in predicting gastrointestinal and renal involvement in children with Henoch-Schönlein Purpura. Postgrad Med 133:272–277. https://doi.org/10.1080/00325481.2020.1807161
Furer A, Finkelstein A, Halkin A et al (2015) High red blood cell distribution width and preclinical carotid atherosclerosis. Biomarkers 20:376–381. https://doi.org/10.3109/1354750X.2015.1096304
Wei J, Yang RX, Ye Q et al (2018) Higher risk of myocardial injury in chest pain patients with elevated red blood cell distribution width. Clin Chim Acta 481:121–125. https://doi.org/10.1016/J.CCA.2018.03.001
Huang YL, Hu ZD, Liu SJ, et al (2014) Prognostic value of red blood cell distribution width for patients with heart failure: a systematic review and meta-analysis of cohort studies. PLoS ONE 9:e104861. https://doi.org/10.1371/JOURNAL.PONE.0104861
Li J, Li D-E, Hu M et al (2022) Red blood cell distribution width and tumor necrosis factor-α for the early prediction of coronary artery lesion in Kawasaki disease: a retrospective study. Eur J Pediatr 181:903–909. https://doi.org/10.1007/S00431-021-04252-3
Zhu X, Zhang M, Lan F et al (2018) The relationship between red cell distribution width and the risk of Henoch-Schönlein purpura nephritis. Br J Biomed Sci 75:30–35. https://doi.org/10.1080/09674845.2017.1368184
Xu H, Li W, Mao JH, Pan YX (2017) Association between red blood cell distribution width and Henoch-Schonlein purpura nephritis. Medicine 96:e7091. https://doi.org/10.1097/MD.0000000000007091
Korniluk A, Koper-Lenkiewicz OM, Kamińska J et al (2019) Mean Platelet Volume (MPV): new perspectives for an old marker in the course and prognosis of inflammatory conditions. Mediators Inflamm 2019:9213074. https://doi.org/10.1155/2019/9213074
Kaser A, Brandacher G, Steurer W et al (2001) Interleukin-6 stimulates thrombopoiesis through thrombopoietin: role in inflammatory thrombocytosis. Blood 98:2720–2725. https://doi.org/10.1182/BLOOD.V98.9.2720
Narci H, Turk E, Karagulle E et al (2013) The role of mean platelet volume in the diagnosis of acute appendicitis: a retrospective case-controlled study. Iran Red Crescent Med J 15:e11934. https://doi.org/10.5812/IRCMJ.11934
Shen G, Li S, Shao Z et al (2021) Platelet indices in patients with acute appendicitis: a systematic review with meta-analysis. Updat Surg 73:1327–1341. https://doi.org/10.1007/S13304-020-00928-X
Albayrak Y, Albayrak A, Albayrak F et al (2011) Mean platelet volume: a new predictor in confirming acute appendicitis diagnosis. Clin Appl Thromb 17:362–366. https://doi.org/10.1177/1076029610364520
Uyanik B, Kavalci C, Arslan ED et al (2012) Role of mean platelet volume in diagnosis of childhood acute appendicitis. Emerg Med Int 2012:823095. https://doi.org/10.1155/2012/823095
Chen Z, Lu Y, Wu J, Zhang H (2021) Clinical significance of blood platelets and mean platelet volume in patients with ulcerative colitis. J Int Med Res 49:1–9. https://doi.org/10.1177/03000605211009715
Li B, Ren Q, Ling J et al (2021) Clinical relevance of neutrophil-to-lymphocyte ratio and mean platelet volume in pediatric Henoch-Schonlein Purpura: a meta-analysis. Bioengineered 12:286–295. https://doi.org/10.1080/21655979.2020.1865607
Acknowledgements
The author would like to thank Prof. Mizu Jiang and Prof. Yunguang Bao for their supports and encouragement for this article writing. The author also would like to thank doctor Xiaobing Li for his support for data collection. Xinyi Jia conceived the study and participated in its design, coordination, and data interpretation as well as review of the manuscript. Ting Yang, Jing Miao and Linqian Zhang carried out data acquisition and got involved in data interpretation as well as manuscript preparation. All authors read and approved the manuscript. We also would like to thank Editage (www.editage.cn) for English language editing.
Funding
No specific funding was received from public, commercials or organizations. The study was carried out for no profit.
Author information
Authors and Affiliations
Contributions
Xinyi Jia conceived the study and participated in its design, coordination, and data interpretation as well as review of the manuscript. Ting Yang, Jing Miao and Linqian Zhang carried out data acquisition and got involved in data interpretation as well as manuscript preparation. All authors read and approved the manuscript. Xiaobing Li and Yunguang Bao are responsible for checking the patient information and analyzing the rationality of the data. Mizu Jiang is responsible for article review and detail optimization.
Corresponding author
Ethics declarations
Conflict of interests
The authors have declared no conflicts of interest.
Ethics approval and consent to participate
This study was approved by the medical ethics committee of the Jinhua Municipal Central Hospital; written informed consent was obtained from parents.
Research involving human participants and/or animals and Informed consent
This study was approved by the Institutional Ethics Review Board for human studies at the Jinhua Municipal Central Hospital (Permission number: 2019-014-001), and written informed consent was obtained from the parents prior to the present study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jia, X., Yang, T., Miao, J. et al. Blood routine examination: a simple way for differential diagnosis of immunoglobulin A vasculitis with abdominal involvement and appendicitis in children. Updates Surg 74, 1683–1689 (2022). https://doi.org/10.1007/s13304-022-01299-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-022-01299-1