Abstract
Despite existing evidence-based practice guidelines for the management of biliary acute pancreatitis (AP), the clinical compliance with recommendations is overall poor. Studies in this field have identified significant discrepancies between evidence-based recommendations and daily clinical practice. The most commonly reported gaps between clinical practice and AP guidelines include the indications for CT scan, need and timing of artificial nutritional support, indications for antibiotics, and surgical/endoscopic management of biliary AP. The MANCTRA-1 (coMpliAnce with evideNce-based cliniCal guidelines in the managemenT of acute biliaRy pancreAtitis) study is aiming to identify the areas for quality improvement that will require new implementation strategies. The study primary objective is to evaluate which items of the current AP guidelines are commonly disregarded and if they correlate with negative clinical outcomes according to the different clinical presentations of the disease. We attempt to summarize the main areas of sub-optimal care due to the lack of compliance with current guidelines to provide the basis for introducing a number of bundles in AP patients’ management to be implemented during the next years. The MANCTRA-1 study is an international multicenter, retrospective cohort study with the purpose to assess the outcomes of patients admitted to hospital with a diagnosis of biliary AP and the compliance of surgeons worldwide to the most up-to-dated international guidelines on biliary AP. ClinicalTrials.Gov ID Number: NCT04747990, Date: February 23, 2021. Protocol Version V2.2.
Similar content being viewed by others
Introduction
Acute pancreatitis (AP) is an inflammatory disease of the pancreas, most commonly caused by gallstones or excessive alcohol use. The incidence of AP ranges globally from 5 to 30 cases per 100.000 inhabitants/year, and there is evidence that the incidence has increased in recent years. The overall case-fatality rate for AP is roughly 5%, and it is expectedly higher for more severe stages of the disease [1, 2]. In most cases (80%), the outcome of AP is rapidly favorable [3]. However, acute necrotizing pancreatitis (ANP) may develop in up to 20% of cases and is associated with significant rates of early organ failure (38%), needing some surgical/endoscopic intervention (38%), and death (15%) [4].
Infection of pancreatic necrosis is the predominant driver of sustained morbidity and late mortality in patients with severe AP. The subset of patients with ANP may face a complicated and prolonged clinical course with an associated mortality of up to 30% if an infection develops in the necrotic collection [5]. Optimal management of patients with pancreatic necrosis requires a multidisciplinary approach, and ad-hoc guidelines for this specific subgroup of patients have been recently released [6]. Although antibiotic prophylaxis may prevent or reduce the risk of necrosis colonization, the results of randomized-controlled trials (RCTs) evaluating this approach and meta-analyses do not support routine use of antibiotic prophylaxis in these patients [7]. However, several global overviews assessing reports from across the world of the use of antibiotics in prophylaxis in AP have shown a wide diffusion of such behavior [8].
In 2020, the spread of the virus COVID-19 represented a pandemic, which also profoundly impacted the surgical community [9,10,11]. The constant increase in the number of patients requiring treatment became a massive challenge for the healthcare systems of many involved countries. In an emergency situation, resources must be focused and used rationally to handle the pandemic as well as to continue handling the pre-existing diseases. In this context, most surgical departments were obliged to re-schedule their activity, giving priority to urgent/emergent surgical cases and non-deferrable oncological cases. The outbreak of the COVID-19 pandemic could have influenced in many ways the daily clinical practice for patients with biliary AP, leading to a failure in adherence to the recommendations provided by the guidelines, especially those regarding the early and definitive treatment with cholecystectomy or endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy. First of all, the recommendation to postpone all non-urgent endoscopic procedures during the peak of the pandemic; second, the recommendation to conservatively treat inflammatory conditions such as acute cholecystitis and acute appendicitis wherever possible.
Several scientific societies have issued practice guidelines and consensus documents over the past decades to guide physicians and surgeons in managing AP [12,13,14,15,16,17,18,19]. The main topics of such guidelines included diagnosis, use of prophylactic antibiotics, management in the intensive-care unit, surgical and operative management, and open abdomen management.
The rationale for the study
It is commonly thought that clinical guidelines would help to decrease inappropriate variation of practice, as well as that they provide a rational basis for referral, and they would help to reduce uncertainty in the management of certain conditions. Clinical guidelines also provide a basis for continuing medical education and can improve control of healthcare costs. However, the value of national and/or international guidelines is mostly dependent on a strategy for their implementation.
Even though the contemporary literature includes several studies on the management of biliary AP, reports about the real-world implementation of evidence-based recommendations coming from AP guidelines are scant. As the way in which biliary AP is managed in the early stages could impact the progression of the disease and subsequent events, it would be important to investigate how recommendations from guidelines are perceived in the real world by clinicians worldwide. Numerous Clinical Audit about biliary AP has been performed in Italy, Germany, France, and England [20,21,22,23], revealing discrepancies in AP management and lack of compliance to guidelines [20, 22,23,24,25,26]. The most commonly reported gaps between clinical practice and guidelines include the indications for CT scan, need and timing of artificial nutritional support, indications for antibiotics, and surgical/endoscopic management of biliary AP. Less than 15% of the respondents stated that they strictly followed all recommendations included in the guidelines in Germany [22], and 25.8% of patients did not receive definitive treatment for biliary AP within 1 year in the UK [27]. A recent study from Singapore aiming to review the clinical management of patients with AP in an HPB referral center in the light of assessing the compliance to the 2013 International Association of Pancreatology (IAP)/American Pancreatic Association (APA) and the 2015 Japanese guidelines found that only 50% of patients received Ringer lactate for initial fluid resuscitation, 38.7% received antibiotics as prophylaxis, 21.4% of patients with severe AP had early enteral nutrition, and only 21.4% patients with biliary AP had index admission cholecystectomy despite the recommendations [28]. In another recent study by a Canadian group, only 25% of patients with gallstones AP underwent a cholecystectomy on the same admission. Furthermore, only one-quarter of patients in whom an index admission cholecystectomy was not possible underwent ERCP with sphincterotomy, and only one-third of patients with gallstones AP and an imaging-confirmed obstructed common bile duct had an ERCP and sphincterotomy [29]. Slow implementation of the guidelines on early cholecystectomy has also been reported in a Danish survey seeking compliance with the recommendations of the national reference program for the treatment of patients with gallstone disease [30], and a similar lack of compliance with guidelines was found in Italy, mainly regarding indications for endoscopic and surgical management [31]. Conversely, a recent study from Sweden found that 80% of patients with biliary AP underwent definitive treatment during their first attack (68% cholecystectomy, 17% ERCP and sphincterotomy, 15% both interventions) [32].
The MANCTRA-1 (coMpliAnce with evideNce-based cliniCal guidelines in the managemenT of acute biliaRy pancreAtitis) study can identify a number of areas for quality improvement that will require new implementation strategies. We aim to summarize the main areas of sub-optimal care due to the lack of compliance with current guidelines and the possible correlation between non-compliance with guidelines and adverse outcomes to finally provide the basis for introducing a number of bundles in the management of patients with AP, to be implemented during the next years.
Methods
The MANCTRA-1 study protocol is designed according to the SPIRIT 2013 explanation and elaboration: guidance for protocols of clinical trials [33]. The MANCTRA Steering Committee, composed of delegates from the World Society of Emergency Surgery (WSES), the Association of Italian Surgeons in Europe (ACIE), the Italian Society of Endoscopic Surgery and new technologies (SICE), and the Spanish Association of Surgeons—HPB Section (AEC), developed the questionnaire using web-based and remote discussion, after identifying the components and topics to include.
Aim of the study
Since the clinical compliance with recommendations about AP is poor and the impact of implementing guidelines recommendations in biliary AP has not been well studied globally, we launched the MANCTRA-1 study with the aim to demonstrate areas where there is currently a sub-optimal implementation of current guidelines on biliary AP.
Moreover, we argue that during the COVID-19 pandemic, the tendency to disregard the guidelines recommendations has been more marked than usual, and we will try to find out if the care of AP patients during the COVID-19 pandemic resulted in a higher rate of adverse outcomes compared to non-pandemic times due to the lack of compliance to guidelines.
Primary aim
-
To evaluate which items of the current AP guidelines, if disregarded, correlate with negative clinical outcomes according to the different clinical presentations of the disease.
Secondary aim
-
To assess the compliance of surgeons worldwide to the most up-to-date international guidelines on biliary AP.
-
To evaluate the medical and surgical practice in the management of biliary AP during the non-pandemic (2019) and pandemic COVID-19 periods (2020).
-
To investigate outcomes of patients with biliary AP treatment during the two study periods.
Primary outcome measures
-
In-hospital mortality: assessed by the number of patients deceased in hospital due to complications directly related to AP with biliary etiology during the non-pandemic period (2019) and the COVID-19 pandemic period (2020).
-
In-hospital morbidity: assessed by the number of AP patients with biliary etiology who experienced any type of AP-related complication during the hospital admission in 2019 (non-pandemic period) and 2020 (pandemic period).
Secondary outcome measures
-
Early definitive treatment rate in 2019 vs. 2020: defined as treatment in accordance with the current guidelines (cholecystectomy or ERCP with endoscopic sphincterotomy during the same hospital admission or within 2 weeks of discharge).
-
30-Day hospital readmission rate in 2019 vs. 2020: defined as hospital readmission within 30 days from discharge for recurrent biliary AP while awaiting interval cholecystectomy, or due to post-cholecystectomy complications.
-
Predictive factors of morbidity and mortality in patients with biliary AP.
The compliance of surgeons to the most up-to-date international guidelines on biliary AP will be assessed through the analysis of the following attitudes:
-
Use of scoring systems for the diagnosis and severity grading of biliary AP.
-
Use of lipase dosage (for the diagnosis) and C-reactive protein—CRP (for the severity grading) during the diagnostic workup.
-
Use of Ultrasound scan, CT scan, MRCP, and endoscopic Ultrasound scan (EUS) in the correct way and timing.
-
Use of early ERCP and sphincterotomy in case of cholangitis and/or choledocholithiasis.
-
Use of percutaneous and/or endoscopic drainage in case of infected pseudocyst or walled-off necrosis (WON).
-
Timing of surgical necrosectomy.
-
Timing of re-laparotomy in case of open abdomen strategies.
-
Use of prophylactic antibiotics/antifungals in the first week.
-
Use of somatostatin analogs.
-
Use of early oral/enteral feeding.
-
Use of early definitive treatment strategies, including cholecystectomy and/or ERCP and sphincterotomy.
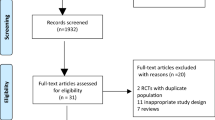
Study design
The MANCTRA-1 study is an international multicenter, retrospective cohort study to assess the outcomes of patients admitted to hospital with a diagnosis of biliary AP and the compliance of surgeons worldwide to the most up-to-dated international guidelines on biliary AP. The study compares data collected in 2019 (pre-pandemic period) with those of 2020 (COVID-19 pandemic period).
Study population
All consecutive adult patients admitted to the participating surgical departments with a clinical and radiological diagnosis of biliary AP (with and without concomitant cholecystitis) between 01/01/2019 and 31/12/2020 will be included in the study. Patient data will be retrospectively analyzed, and demographic characteristics, comorbidity status, clinical and radiological findings, treatment strategies, in-hospital morbidity, and mortality will be evaluated.
Inclusion criteria
Patients of both sexes, ≥ 16 years old, admitted to any of the participating general surgery departments, hepatopancreatobiliary (HPB) surgery departments, and/or internal medicine or gastroenterology departments for biliary AP in 2019 and 2020.
Exclusion criteria
Patients with AP having an etiology other than gallstones; pregnant patients.
Study periods
The pre-pandemic period runs from 01/01/2019 to 31/12/2019. The COVID-19 pandemic period is from 01/01/2020 to 31/12/2020. Data will be entered in the database from 01/04/2021 to 31/08/2021. Strategies to identify consecutive patients will include review of elective and emergency theater logbooks, review of handover sheets and ward lists, and review of institutional databases.
Sample size
Studies on biliary AP found a mortality rate of approximately 10%. Patients with biliary AP tend to have a higher mortality than patients with alcoholic pancreatitis. However, this rate has been falling over the last 2 decades as improvements in supportive care have been introduced. In patients with severe disease (organ failure), accounting for about 20% of presentations, mortality is approximately 30%. This rate has not decreased in the past 10 years.
We estimate that a minimum of 200 patients per group (2019 vs. 2020) would yield a power of 0.80 (1-β) to establish whether changes in clinical care for patients with biliary AP during the COVID-19 pandemic has impacted on overall mortality using a one-sided significance α level of 0.05 (5%) with power sample size calculator (sealedenvelope.com).
Statistical analysis
The dichotomous variables will be expressed as numbers and percentages, while continuous variables will be expressed as mean and standard deviation (SD), or median and interquartile range (IQR, minimum and maximum values). Student’s t test or ANOVA will be used for comparisons of continuous variables between groups. Chi-squared test or Fisher’s exact test, as appropriate, will be used for analysis of categorical data.
A propensity score model will be implemented considering the following variables as covariates: patient age, sex, Body Mass Index (BMI), Charlson’s comorbidity index, q-SOFA score, WSES sepsis score, BISAP (Bedside Index of Severity in Acute Pancreatitis) score, ASA score, Glasgow-Imrie score, Ranson’s score, and presence of concomitant findings on admission (choledocholithiasis with common bile duct obstruction, cholangitis). Patients treated in 2019 and 2020 will be matched using the “nearest neighbor matching,” based on the individual propensity score and with a 1:1 matching model with replacement.
Planned investigations of subgroups will be carried out for different severity grades of the disease according to the revised Atlanta Classification [34], setting of acquisition of the pancreatitis (community acquired or hospital acquired), and hospital characteristics (Academic/Non-Academic setting, performance factors related to hospital patient volume, access to hepatopancreatobiliary subspecialty services, and admitting speciality);
Multiple regression model, including moderation and mediation analysis, will be used to investigate clinical variables (independent) predictive of morbidity and mortality:
-
Non-compliance to AP practice guidelines regarding medical and antibiotic therapy, nutritional support, management of complications, endoscopic treatment, and timing of cholecystectomy;
-
COVID-19 status on admission;
-
Physical, laboratory, and radiologic variables.
Residual analysis will also be conducted to investigate the amount of information that cannot be explained by the model. Machine learning (ML) such as random forest and ANNs will also be used to investigate the information held within the predictor variables.
A value of P < 0.05 will be considered statistically significant.
Ethical aspects and publication policy
This is an international observational study; it will not attempt to change or modify the clinical practice of the participating physicians. The study will meet and conform to the standards outlined in the Declaration of Helsinki and Good Epidemiological Practices.
Ethics Committee approval was obtained in Italy (Acceptance Code: Independent Ethics Committee of the University of Cagliari, Prot. PG/2021/7108) from the coordinating center.
National leads in other countries will oversee appropriate registration and study approval, which may include completing full ethical review depending on the local policy for observational and non-interventional studies. Local leads from the UK participating centers will be prompted to consider using the HRA REC National Research Ethics Service decision tool (http://www.hra-decisiontools.org.uk) to know whether a formal ethical approval is required to take part in the study.
The Local lead and two Collaborators from each center will be listed as Co-authors in the final publications. Data will be published as a pool from all participating surgical units [35], and published irrespective of findings. Results will be published on ClinicalTrials.Gov and each manuscript that is generated based on the registry will be disseminated to all participating centers before final publication.
Data collection
National committees will lead the study in participating countries, with overall coordination provided by the study steering committee. The MANCTRA-1 study involves 286 clinical centers from 51 countries worldwide to date (Fig. 1). In each center, the coordinator will collect epidemiological, clinical, and surgical data on a case report form (CRF) that will be completed by accessing a protected data system. The link for accessing the completion of the CRF will be sent via email to only one contact person (local lead) of each participating center (Suppl. Material Table 1). The database was developed by the MANCTRA-1 Steering Committee using web-based and remote discussion, after identifying the key components and topics to include. Seventeen clinical sections were identified, that included closed and open-ended questions. Online questions and response items in the Google Forms database are available by accessing the link https://forms.gle/PLZhf73kGtNhhJEy7.
Data will be recorded contemporaneously on a dedicated server that allows collaborators to enter and store data in a secure system (Google Form survey software, Google, Mountain View, California, USA) hosted and managed by the University of Cagliari, Italy. No patient identifiable data (name, date of birth, address, telephone number, etc.) will be recorded. A database will be generated in Excel for Mac, and final statistical analyses will be performed using R version 4.0.2 and SPSS V.22.
Due to its retrospective design, this observational study will not attempt to change or modify the laboratory or clinical practices of the participating physicians. Consequently, informed consent will not be required.
Data completeness
Strategies to identify consecutive patients with biliary AP admitted at each participating center from 01/01/2019 to 31/12/2019 will include: manual review of emergency hospital admissions; electronic review of the hospital admissions software with specific query for AP codes; manual or electronic review of handover sheets and ward lists; manual or electronic review of theater logbooks.
Following data collection, only data sets with > 95% data completeness will be accepted for pooled international analyses. Centers who do not upload patients meeting the eligibility criteria or with > 5% missing data points cannot be included in the study and local leads from those centers will be asked to complete the missing boxes with the requested data. Failure to meet these requirements will cause the exclusion from the publication list.
Discussion
Findings from previous studies about the compliance with AP guidelines support the view that publication only of nationally or internationally developed and approved guidelines is insufficient to modify the practice of non-specialists and raises the question of how best to spread guideline recommendations. Previous reports, including the one from France in 2012, have shown that major changes in biliary AP patients’ management were noticed since the French guidelines publication. In particular, after the publication of the mentioned guidelines, lipase levels were measured for establishing AP diagnosis by 99% (vs. 83% pre-guidelines), and a CT scan was performed at 48 h by 69% (vs. 29% pre-guidelines) to evaluate AP severity. Antibiotic prophylaxis and enteral nutrition were proposed by 20% (vs. 57% pre-guidelines) and 58% (vs. 25% pre-guidelines) for necrotizing AP [36].
In a recent multicenter international survey on the patterns of early management of AP, Talukdar et al. demonstrated that there is still non-compliance to practice guidelines in severity prediction, fluid therapy monitoring, use of antibiotics, and feeding modalities. Among the participating specialists who followed the guidelines, nearly 42% and 60% were actually non-compliant to feeding and antibiotic recommendations, respectively [24]. Moreover, there are significant differences in behaviors regarding various aspects of fluid therapy, feeding, and antibiotic use between clinicians from academic and non-academic centers. A significantly higher proportion of clinicians from academic centers would use Ringer’s solution as the first fluid choice compared to non-academic practice groups (79.2% vs. 55.6%), whereas a significantly higher proportion of clinicians in the non-academic setting would start antibiotics during the first week of illness based on the presence of necrosis on CT scan. Relevant differences in AP management also exist between the admitting specialists. The authors found that a significantly higher proportion of physicians compared to surgeons (53.1% vs. 27.8%) opted to use SIRS criteria to assess severity, whereas a significantly higher proportion of surgeons compared to physicians would opt to use nasogastric tube (40.7% vs. 26.3%) [24]. Reasons for which we decided to plan investigations of subgroups basing on hospital characteristics, performance factors related to hospital patient volume, the admitting specialty, and the availability of hepatopancreatobiliary subspecialty services.
Discrepancies in management and lack of compliance to guidelines had been reported earlier in different surveys from Europe and New Zealand [22,23,24]. Aly et al. showed in their survey that significant differences in survey assessment, indication, and timing of requesting CT scan and nutritional support existed between the practice of HPB specialists and non-specialists [26]. A subsequent survey in 2012 that involved 51 surgical departments (nine academic hospitals and 42 non-academic hospitals) in Sweden also revealed a lack of early severity stratification and a difference in standard of care between different hospitals [25]. These studies emphasized on two relevant issues: the need for evidence-based standardization of management of biliary AP, and the importance of a timely referral to a specialist unit for patients with severe AP and those with extensive necrotizing forms or with other complications who may require intensive therapy unit care, or interventional radiological, endoscopic, or surgical procedures. The management of severe cases of AP requires not only the availability of numerous specialty services (gastroenterology, surgery, critical care, and interventional radiology), but also the experience to coordinate a multidisciplinary team. An analysis of the United States Nationwide Inpatient sample showed that treatment of patients with AP in high-volume centers resulted in a decreased risk of prolonged hospital stay and mortality [37, 38]. According to the UK Party on Acute Pancreatitis, every hospital that receives acute admission should have a nominated multidisciplinary clinical team to manage all patients with AP. If the full range of specialists is not available in the receiving hospital, the nominated team should coordinate local management where possible, and the referral to a specialist unit where appropriate. Moreover, in every hospital, the nominated team should maintain regular audit of all patients with AP under a coordination at a regional level [14]. Similarly, the International Association of Pancreatology (IAP) and the American Pancreatic Association (APA) stated that management in, or referral to, a specialist center is necessary for patients with severe AP and for those who may need interventional radiologic, endoscopic, or surgical operation. A specialist center in the management of AP is defined as a high-volume center with intensive-care facilities and with daily access to interventional radiology, interventional endoscopy with EUS and ERCP assistance, as well as surgical expertise in managing necrotizing AP. A minimum of two specialists should be available in all field of expertise (interventional endoscopy, interventional radiology, critical care medicine, and surgery) to allow for minimum coverage [15].
On these premises, we have started the MANCTRA project, a global research alliance aiming to improve the care of biliary AP worldwide. The MANCTRA-1 retrospective cohort study represents the first step of the project, and it has been launched to summarize the contemporary main areas of sub-optimal care due to the lack of compliance with current guidelines. Unlike the earlier studies that involved primarily surgeons within particular national societies, in the MANCTRA-1 study, we involved different healthcare specialists that handle patients with biliary AP. The results of the MANCTRA-1 study will be analyzed with the perspective to provide the basis for introducing a number of bundles in biliary AP patients' management to be implemented during the next years. Following the introduction of the AP bundles in 2022, the MANCTRA-2 prospective international study will be launch in 2025 to assess the potential advancements for biliary AP patients’ care in those centers that have taken part in the project.
Conclusion
Biliary AP represents a therapeutic challenge and a significant burden for the healthcare systems. Sub-optimal care of AP patients due to the lack of compliance with current guidelines is related with an increasing rate of adverse events. A global effort is necessary to improve biliary AP patients care. The MANCTRA-1 international retrospective cohort study will evaluate which items of the current AP guidelines, will correlate, if disregarded, with negative clinical outcomes according to the different clinical presentations of the disease, ultimately aiming to introduce new improvement strategies for the care of patients suffering from biliary AP.
Data availability
The data that support the findings of this study will be available on request from the principal investigator [M.P.].
Code availability
Not applicable.
Abbreviations
- AP:
-
Acute pancreatitis
- IAP:
-
International Association of Pancreatology
- APA:
-
American Pancreatic Association (APA)
- ANP:
-
Acute necrotizing pancreatitis
- RCTs:
-
Randomized-controlled trials
- Covid-19:
-
Coronavirus disease 2019
- ERCP:
-
Endoscopic retrograde cholangiopancreatography
- CRP:
-
C-reactive protein
- CT:
-
Computed tomography
- MRCP:
-
Magnetic resonance cholangiopancreatography
- WON:
-
Walled-off necrosis
- CRF:
-
Case report form
- HPB:
-
Hepato-pancreato-biliary
References
Krishna SG, Kamboj AK, Hart PA, Hinton A, Conwell DL (2017) The changing epidemiology of acute pancreatitis hospitalizations: a decade of trends and the impact of chronic pancreatitis. Pancreas 46:482–488
Koutroumpakis E, Slivka A, Furlan A, Dasyam AK, Dudekula A, Greer JB, Whitcomb DC, Yadav D, Papachristou GI (2017) Management and outcomes of acute pancreatitis patients over the last decade: a US tertiary-center experience. Pancreatology 17:32–40
Singh VK, Bollen TL, Wu BU, Repas K, Maurer R, Yu S, Mortele KJ, Conwell DL, Banks PA (2011) An assessment of the severity of interstitial pancreatitis. Clin Gastroenterol Hepatol 9:1098–1103
van Santvoort HC, Bakker OJ, Bollen TL, Besselink MG, Ahmed Ali U, Schrijver AM, Boermeester MA, van Goor H, Dejong CH, van Eijck CH, van Ramshorst B, Schaapherder AF, van der Harst E, Hofker S, Nieuwenhuijs VB, Brink MA, Kruyt PM, Manusama ER, van der Schelling GP, Karsten T, Hesselink EJ, van Laarhoven CJ, Rosman C, Bosscha K, de Wit RJ, Houdijk AP, Cuesta MA, Wahab PJ, Gooszen HG, Dutch Pancreatitis Study Group (2011) A conservative and minimally invasive approach to necrotizing pancreatitis improves outcome. Gastroenterology 141:1254–1263
Trikudanathan G, Wolbrink DRJ, van Santvoort HC, Mallery S, Freeman M, Besselink MG (2019) Current concepts in severe acute and necrotizing pancreatitis: an evidence-based approach. Gastroenterology 156:1994-2007.e3. https://doi.org/10.1053/j.gastro.2019.01.269
Baron TH, DiMaio CJ, Wang AY, Morgan KA (2020) American gastroenterological association clinical practice update: management of pancreatic necrosis. Gastroenterology 158:67-75.e1. https://doi.org/10.1053/j.gastro.2019.07.064
Lim CL, Lee W, Liew YX, Tang SS, Chlebicki MP, Kwa AL (2015) Role of antibiotic prophylaxis in necrotizing pancreatitis: a meta-analysis. J Gastrointest Surg 19:480–491
Baltatzis M, Jegatheeswaran S, O’Reilly DA, Siriwardena AK (2016) Antibiotic use in acute pancreatitis: global overview of compliance with international guidelines. Pancreatology 6:189–193
COVIDSurg Collaborative (2020) Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet 396:27–38
Pandanaboyana S, Moir J, Leeds JS, Oppong K, Kanwar A, Marzouk A, Belgaumkar A, Gupta A, K Siriwardena A, Haque AR, Awan A, Balakrishnan A, Rawashdeh A, Ivanov B, Parmar C, M Halloran C, Caruana C, Borg CM, Gomez D, Damaskos D, Karavias D, Finch G, Ebied H, K Pine J, Raa Skipworth J, Milburn J, Latif J, Ratnam Apollos J, El Kafsi J, Windsor JA, Roberts K, Wang K, Ravi K, Vee Coats M, Hollyman M, Phillips M, Okocha M, Sj Wilson M, A Ameer N, Kumar N, Shah N, Lapolla P, Magee C, Al-Sarireh B, Lunevicius R, Benhmida R, Singhal R, Balachandra S, Demirli Atıcı S, Jaunoo S, Dwerryhouse S, Boyce T, Charalampakis V, Kanakala V, Abbas Z, Nayar M (2021) SARS-CoV-2 infection in acute pancreatitis increases disease severity and 30-day mortality: COVID PAN collaborative study. Gut. https://doi.org/10.1136/gutjnl-2020-323364
Bracale U, Podda M, Castiglioni S, Peltrini R, Sartori A, Arezzo A, Corcione F, Agresta F, CLOUD-19 Collaborative Group (2021) Changes in surgical behaviors during the covid-19 pandemic. The SICE CLOUD19 Study. Updates Surg. https://doi.org/10.1007/s13304-021-01010-w
Leppäniemi A, Tolonen M, Tarasconi A, Segovia-Lohse H, Gamberini E, Kirkpatrick AW, Ball CG, Parry N, Sartelli M, Wolbrink D, van Goor H, Baiocchi G, Ansaloni L, Biffl W, Coccolini F, Di Saverio S, Kluger Y, Moore E, Catena F (2019) 2019 WSES guidelines for the management of severe acute pancreatitis. World J Emerg Surg 13(14):27. https://doi.org/10.1186/s13017-019-0247-0
Crockett SD, Wani S, Gardner TB, Falck-Ytter Y, Barkun AN, Committee AGAICG (2018) American Gastroenterological Association Institute Guideline on Initial Management of Acute Pancreatitis. Gastroenterology 154:1096–1101
Working Party of the British Society of Gastroenterology; Association of Surgeons of Great Britain and Ireland; Pancreatic Society of Great Britain and Ireland; Association of Upper GI Surgeons of Great Britain and Ireland (2005) UK guidelines for the management of acute pancreatitis. Gut 54(Suppl 3):iii1-9. https://doi.org/10.1136/gut.2004.057026
Working Group IAP/APA Acute Pancreatitis Guidelines (2013) IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology 13:e1-15. https://doi.org/10.1016/j.pan.2013.07.063
Tenner S, Baillie J, DeWitt J, Vege SS, American College of Gastroenterology (2013) American College of Gastroenterology guideline: management of acute pancreatitis. Am J Gastroenterol 108:1400–1415
Italian Association for the Study of the Pancreas (AISP), Pezzilli R, Zerbi A, Campra D, Capurso G, Golfieri R, Arcidiacono PG, Billi P, Butturini G, Calculli L, Cannizzaro R, Carrara S, Crippa S, De Gaudio R, De Rai P, Frulloni L, Mazza E, Mutignani M, Pagano N, Rabitti P, Balzano G (2015) Consensus guidelines on severe acute pancreatitis. Dig Liver Dis 47:532–543
Yokoe M, Takada T, Mayumi T, Yoshida M, Isaji S, Wada K, Itoi T, Sata N, Gabata T, Igarashi H, Kataoka K, Hirota M, Kadoya M, Kitamura N, Kimura Y, Kiriyama S, Shirai K, Hattori T, Takeda K, Takeyama Y, Hirota M, Sekimoto M, Shikata S, Arata S, Hirata K (2015) Japanese guidelines for the management of acute pancreatitis: Japanese Guidelines 2015. J Hepatobiliary Pancreat Sci 22:405–432
Vivian E, Cler L, Conwell D, Coté GA, Dickerman R, Freeman M, Gardner TB, Hawes RH, Kedia P, Krishnamoorthi R, Oduor H, Pandol SJ, Papachristou GI, Ross A, Sethi A, Varadarajulu S, Vege SS, Wassef W, Wilcox CM, Whitcomb DC, Wu BU, Yadav D, Ellison A, Habash S, Rastegari S, Reddy R, Yen T, Brooks MR, Tarnasky P (2019) Acute pancreatitis task force on quality: development of quality indicators for acute pancreatitis management. Am J Gastroenterol 114:1322–1342
Toh SK, Phillips S, Johnson CD (2000) A prospective audit against national standards of the presentation and management of acute pancreatitis in the South of England. Gut 46:239–243
Gurusamy KS, Farouk M, Tweedie JH (2005) UK guidelines for management of acute pancreatitis: is it time to change? Gut 54:1344–1345
Lankisch PG, Weber-Dany B, Lerch MM (2005) Clinical perspectives in pancreatology: compliance with acute pancreatitis guidelines in Germany. Pancreatology 5:591–593
Cavallini G, Frulloni L, Bassi C, Gabbrielli A, Castoldi L, Costamagna G, De Rai P, Di Carlo V, Falconi M, Pezzilli R, Uomo G, ProInf-AISP Study Group (2004) Prospective multicentre survey on acute pancreatitis in Italy (ProInf-AISP): results on 1005 patients. Dig Liver Dis 36:205–211
Talukdar R, Tsuji Y, Jagtap N, Pradeep R, Rao GV, Reddy DN (2021) Non-compliance to practice guidelines still exist in the early management of acute pancreatitis: time for reappraisal? Pancreatology. https://doi.org/10.1016/j.pan.2021.05.301
Andersson B, Andrén-Sandberg A, Nilsson J, Andersson R (2012) Survey of the management of acute pancreatitis in surgical departments in Sweden. Scand J Gastroenterol 47:1064–1070
Aly EA, Milne R, Johnson CD (2002) Non-compliance with national guidelines in the management of acute pancreatitis in the United kingdom. Dig Surg 19:192–198
Green R, Charman SC, Palser T (2017) Early definitive treatment rate as a quality indicator of care in acute gallstone pancreatitis. Br J Surg 104:1686–1694
Tan JW, Gao Y, Kow AWC, Bonney G, Madhavan K, Windsor JA, Iyer SG (2019) Clinical management and outcomes of acute pancreatitis: identifying areas for quality improvement in a tertiary Asian setting. Pancreatology 19:507–518
Greenberg JA, Hsu J, Bawazeer M, Marshall J, Friedrich JO, Nathens A, Coburn N, Huang H, McLeod RS (2016) Compliance with evidence-based guidelines in acute pancreatitis: an audit of practices in University of Toronto Hospitals. J Gastrointest Surg 20:392–400
Jakobsen HL, Rosenberg J, Schulze S, Kristiansen VB (2005) Behandlingen af galdestenspankreatitis i Danmark [Treatment of gallstone pancreatitis in Denmark]. Ugeskr Laeger 167:2651–2653
Pezzilli R, Uomo G, Gabbrielli A, Zerbi A, Frulloni L, De Rai P, Castoldi L, Cavallini G, Di Carlo V, ProInf-AISP Study Group (2007) A prospective multicentre survey on the treatment of acute pancreatitis in Italy. Dig Liver Dis 39:838–846
Ragnarsson T, Andersson R, Ansari D, Persson U, Andersson B (2017) Acute biliary pancreatitis: focus on recurrence rate and costs when current guidelines are not complied. Scand J Gastroenterol 52:264–269
Chan A-W, Tetzlaff JM, Gøtzsche PC, Altman DG, Mann H, Berlin J, Dickersin K, Hróbjartsson A, Schulz KF, Parulekar WR, Krleža-Jerić K, Laupacis A, Moher D (2013) SPIRIT 2013 explanation and elaboration: Guidance for protocols of clinical trials. BMJ 346:e7586
Banks PA, Bollen TL, Dervenis C, Gooszen HG, Johnson CD, Sarr MG, Tsiotos GG, Vege SS, Acute Pancreatitis Classification Working Group (2013) Classification of acute pancreatitis–2012: revision of the Atlanta classification and definitions by international consensus. Gut 62:102–111
Collaborative EuroSurg (2016) EuroSurg: a new European student-driven research network in surgery. Colorectal Dis 18:214–215
Rebours V, Lévy P, Bretagne JF, Bommelaer G, Hammel P, Ruszniewski P (2012) Do guidelines influence medical practice? Changes in management of acute pancreatitis 7 years after the publication of the French guidelines. Eur J Gastroenterol Hepatol 24:143–148
Singla A, Csikesz NG, Simons JP, Li YF, Ng SC, Tseng JF, Shah SA (2009) National hospital volume in acute pancreatitis: analysis of the Nationwide Inpatient Sample 1998–2006. HPB (Oxford) 11:391–397
Singla A, Simons J, Li Y, Csikesz NG, Ng SC, Tseng JF, Shah SA (2009) Admission volume determines outcome for patients with acute pancreatitis. Gastroenterology 137:1995–2001
Acknowledgements
This study has been endorsed by: The World Society of Emergency Surgery (WSES), the Italian Society of Endoscopic Surgery and New Technologies (SICE), the Association of Italian Surgeons in Europe (ACIE), the Italian Surgical Research Group (ItSurg), the American College of Surgeons (ACS)—Italy Chapter, and the Association of Spanish Surgeons—HPB Section (AEC).
Funding
This research has not received any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All the authors equally contributed in the conception and design of the work, drafted the study protocol and revised it critically for important intellectual content, approved the version to be published, and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the study protocol are appropriately assessed and resolved.
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest.
Ethical approval
All the investigators will conduct the study in accordance with the principles of the Declaration of Helsinki of 1975 (as revised in 2008) and in accordance with the ethical standards of the responsible committee on human experimentation (Independent Ethical Committee for Clinical Trials of Cagliari University Hospital, Italy). All the investigators will conduct the study according to the rules of the ethics committee regarding retrospective collection of data. Ethics Committee approval was obtained (Acceptance Code: Independent Ethics Committee of the University of Cagliari, Prot. PG/2021/7108) from the coordinating center.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Podda, M., Pellino, G., Coccolini, F. et al. Compliance with evidence-based clinical guidelines in the management of acute biliary pancreatitis: the MANCTRA-1 study protocol. Updates Surg 73, 1757–1765 (2021). https://doi.org/10.1007/s13304-021-01118-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-021-01118-z