Abstract
Background
Evidence is growing about the benefits of laparoscopic resection with primary anastomosis (RPA) in perforated diverticulitis. However, the role of a diverting ileostomy in this setting is unclear. The aim of this study was to analyze the outcomes of laparoscopic RPA with or without a proximal diversion in Hinchey III diverticulitis.
Methods
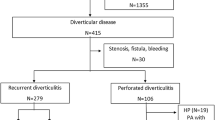
This is a retrospective analysis of patients undergoing laparoscopic sigmoidectomy for perforated Hinchey III diverticulitis during the period 2000–2019. The sample was divided into two groups: RPA without diversion (G1) and RPA with protective ileostomy (G2). Primary outcomes of interest were 30-day overall morbidity, mortality, length of hospital stay (LOS), and urgent reoperation rates. Secondary outcomes of interest included operative time, readmission, and anastomotic leak rates.
Results
Laparoscopic RPA was performed in 94 patients: 76 without diversion (G1) and 18 with proximal loop ileostomy (G2). Mortality (G1: 1.3% vs. G2: 0%, p = 0.6), urgent reoperation (G1: 7.9% vs. G2: 5.6%, p = 0.73), and anastomotic leak rates (G1: 5.3% vs. G2: 0%, p = 0.32) were comparable between groups. Higher overall morbidity (G1: 27.6% vs. G2: 55.6%, p = 0.02) and readmission rates (G1: 1.3% vs. G2: 11.1%, p = 0.03), and longer LOS (G1: 6.3 vs. G2: 9.2 days, p = 0.02) and operative time (G1: 182.4 vs. G2: 230.2 min, p = 0.003) were found in patients with proximal diversion.
Conclusion
Laparoscopic RPA had favorable outcomes in selected patients with Hinchey III diverticulitis. The addition of a proximal ileostomy resulted in increased morbidity, readmissions, and length of stay. Further investigation is needed to establish which patients might benefit from proximal diversion.

Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Nguyen GC, Sam J, Anand N (2011) Epidemiological trends and geographic variation in hospital admissions for diverticulitis in the United States. World J Gastroenterol 17:1600–1605
Ricciardi R, Baxter NN, Read TE, Marcello PW, Hall J, Roberts PL (2009) Is the decline in the surgical treatment for diverticulitis associated with an increase in complicated diverticulitis? Dis Colon Rectum 52:1558–1563
Morris CR, Harvey IM, Stebbings WS, Hart AR (2008) Incidence of perforated diverticulitis and risk factor for death in UK population 95:876–881
Constantinides VA, Tekkis PP, Senapati A (2006) A prospective multicenter evaluation of adverse outcomes following treatment for complicated diverticular disease. BJS 93:1503–1513
Abbas S (2007) Resection and primary anastomosis in acute complicated diverticulitis, a systematic review of the literature. Int J Colorectal Dis 22:351–357
Maggard MA, Zingmond D, O´Connell JB, Ko CY (2004) What proportion of patients with an ostomy (for diverticulitis) get reversed? Am Surg 70:928–931
Banerjee S, Leather AJ, Rennie JA, Samano N, Gonzalez JG, Papagrigoriadis S (2005) Feasibility and morbidity of reversal of Hartmann´s. Colorectal Dis 7:454–459
Binda GA, Karas JR, Serventi A, Sokmen S, Amato A, Hydo L, Bergamaschi R, Study group on diverticulitis (2012) Primary anastomosis vs nonrestorative resection for perforated diverticulitis with peritonitis: a prematurely terminated randomized controlled trial. Colorectal Dis 14(11):1403–1410
Oberkofler CE, Rickenbacher A, Raptis DA, Lehmann K, Villiger P, Buchli C, Grieder F, Gelpke H, Decurtins M, Tempia-Caliera AA, Demartines N, Hahnloser D, Clavien PA, Breitenstein S (2012) A multicenter randomized clinical trial of primary anastomosis or Hartmann’s procedure for perforated left colonic diverticulitis with purulent or fecal peritonitis. Ann Surg 256:819–826
Bridoux V, Regimbeau JM, Ouaissi M, Mathonnet M, Mauvais F, Houivet E, Schwarz L, Mege D, Sielezneff I, Sabbagh C, Tuech JJ (2017) Hartmann’s procedure or primary anastomosis for generalized peritonitis due to perforated diverticulitis: a prospective multicenter randomized trial (DIVERTI). J Am Coll Surg 225:798–805
Lambrichts DPV, Vennix S, Musters GD, Mulder IM, Swank HA, Hoofwijk AGM, Belgers EHJ, Stockmann HBAC, Eijsbouts QAJ, Gerhards MF, van Wagensveld BA, van Geloven AAW, Crolla RMPH, Nienhuijs SW, Govaert MJPM, di Saverio S, D’Hoore AJL, Consten ECJ, van Grevenstein WMU, Pierik REGJM, Kruyt PM, van der Hoeven JAV, Steup WH, Catena F, Konsten JLM, Vermeulen J, van Dieren S, Bemelman WA, Lange JF, LADIES trial collaborators, (2019) Hartmann’s procedure versus sigmoidectomy with primary anastomosis for perforated diverticulitis with purulent or faecal peritonitis (LADIES): a multicentre, parallel-group, randomised, open-label, superiority trial. Lancet Gastroenterol Hepatol 4:599–610
Gachabayov M, Tuech JJ, Tulina I, Coget J, Bridoux V, Bergamaschi R (2020) Primary anastomosis and nonrestorative resection for perforated diverticulitis with peritonitis: meta-analysis of randomized trials. Colorectal Dis. https://doi.org/10.1111/codi.15016
Halim H, Askari A, Nunn R, Hollingshead J (2019) Primary resection anastomosis versus Hartmann’s procedure in Hinchey III and IV diverticulitis. World J Emerg Surg 14:32
Ryan OK, Ryan EJ, Creavin B, Boland MR, Kelly ME, Winter DC (2020) Systematic review and meta-analysis comparing primary resection and anastomosis versus Hartmann’s procedure for the management of acute perforated diverticulitis with generalized peritonitis. Tech Coloproctol. https://doi.org/10.1007/s10151-020-02172-2
Giannakopoulos GF, Veenhof AA, van der Peet DL, Sietses C, Meijerink WJ, Cuesta MA (2009) Morbidity and complications of protective loop ileostomy. Colorectal Dis 11:609–612
Dreifuss NH, Schlottmann F, Piatti JM, Bun ME, Rotholtz NA (2019) Safety and feasibility of laparoscopic sigmoid resection without diversion in perforated diverticulitis. Surg Endosc 34:1336–1342
Vennix S, Boersema GS, Buskens CJ, Menon AG, Tanis PJ, Lange JF, Bemelman WA (2016) Emergency laparoscopic sigmoidectomy for perforated diverticulitis: a systematic review. Dig Surg 33:1–7
Hall J, Hardiman K, Lee S, Lightner A, Stocchi L, Paquette I, Steele SR, Feingold D (2020) The American Society of Colon and Rectal Surgeons clinical practice guidelines for the treatment of left-sided colonic diverticulitis. Dis Colon Rectum 63:728–747
Francis NK, Sylla P, Abou Khalil M, Arolfo S, Berler D, Curtis NJ, Dolejs SC, Garfinkle R, Gorter-Stam M, Hashimoto DA, Hassinger TE, Molenaar CJL, Pucher PH, SchuermansV AA, Agresta F, Antoniou SA, Arulampalam T, Boutros M, Bouvy N, Campbell K, Francone T, Haggerty SP, Hedrick TL, Stefanidis D, Truitt MS, Kelly J, Ket H, Dunkin BJ, Pietrabissa A (2019) EAES and SAGES 2018 consensus conference on acute diverticulitis management: evidence-based recommendations for clinical practice. Surg Endosc 33:2726–2741
Sartelli M, Catena F, Ansaloni L, Coccolini F et al (2016) WSES guidelines for the management of acute left side colonic diverticulitis in the emergency setting. World J Emerg Surg 11:37
Lee JM, Chang BP, J, El Hechi M, Kongkaewpaisan N, Bonde A, Mendoza AE, Saillant NN, Fagenholz PJ, Velmahos G, Kaafarani HM, (2019) Hartmann’s procedure vs primary anastomosis with diverting loop ileostomy for acute diverticulitis: nationwide analysis of 2729 surgery patients. J Am Coll Surg 229:48–55
Baldock TE, Brown LR, McLean RC (2019) Perforated diverticulitis in the North of England: trends in patient outcomes, management approach and the influence of subspecialisation. Ann R Coll Surg Engl 101:563–570
Dreifuss NH, Schlottmann F, Bun ME, Rotholtz NA (2020) Emergent laparoscopic sigmoid resection for perforated diverticulitis: can it be safely performed by residents? Colorectal Dis. https://doi.org/10.1111/codi.14973
Hanna MH, Vinci A, Pigazzi A (2015) Diverting ileostomy in colorectal surgery: when is it necessary. Langenbecks Arch Surg 400:145–152
Thalheimer A, Bueter M, Kortuem M, Thiede A, Meyer D (2006) Morbidity of temporary loop ileostomy in patients with colorectal cancer. Dis Colon Rectum 49:1011–1017
Wise KB, Merchea A, Cima RR, Colibaseanu DT, Thomsen KM, Habermann EB (2015) Proximal intestinal diversion is associated with increased morbidity in patients undergoing elective colectomy for diverticular disease: an ACS-NSQIP study. J Gastrointest Surg 19:535–542
Funding
None.
Author information
Authors and Affiliations
Contributions
All authors contributed to conception and design, acquisition, analysis and interpretation of data, drafting and revising of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors have no conflicts of interest, financial ties, or funding/support to disclose.
Ethics approval/consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the IRB of our institution.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dreifuss, N.H., Bras Harriott, C., Schlottmann, F. et al. Laparoscopic resection and primary anastomosis for perforated diverticulitis: with or without loop ileostomy?. Updates Surg 73, 555–560 (2021). https://doi.org/10.1007/s13304-020-00952-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00952-x