Abstract
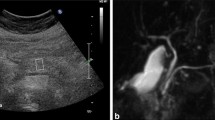
The clinical usefulness of pancreatic elastography (PE) in the assessment of the pancreatic texture before pancreatic resection still remains uncertain. The aims are: to evaluate the value of pancreatic stiffness in both healthy volunteers and patients affected by pancreatic tumor; to evaluate the ability of PE in predicting clinically relevant postoperative pancreatic fistula (CR-POPF). Pancreatic stiffness of healthy subjects was compared with those of pancreatic tumors measuring shear wave velocity (SWV). In the last group, the ability of preoperative SWV in predicting CR-POPF was evaluated using linear regression. Ninety subjects were consecutively enrolled. No difference was found in SWV in the two groups (1.33 ± 0.31 vs 1.26 ± 0.30, p = 0.337). Multivariate analyses showed that male gender was associated with a softer pancreas (OR 0.74, CI 0.55–0.98, p = 0.035). In the 45 patients suitable for a secondary endpoint, the presence of soft pancreas assessed by surgeon’s palpation (OR 61.21; CI 2.14– > 1000; p = 0.016) and preoperative risk score (OR 1.72; CI 1.01–2.96; p = 0.049) was predictors of CR-POPF. SWV showed a trend in predicting CR-POPF. The pancreatic stiffness far to the pancreatic neoplasm is the same as healthy controls. SWV showed a trend in predicting CR-POPF but the clinical utility is limited.

Similar content being viewed by others
References
Casadei R, Ricci C, Taffurelli G, D’Ambra M, Pacilio CA, Ingaldi C et al (2015) Are there preoperative factors related to a “soft pancreas” and are they predictive of pancreatic fistulas after pancreatic resection? Surg Today 45(6):708–714
Shrikhande SV, Sivasanker M, Vollmer CM, Friess H, Besselink MG, Fingerhut A et al (2017) Pancreatic anastomosis after pancreatoduodenectomy: a position statement by the International Study Group of Pancreatic Surgery (ISGPS). Surgery 161(5):1221–1234
Casadei R, Ricci C, Taffurelli G, Pacilio CA, Di Marco M, Pagano N et al (2017) Prospective validation of a preoperative risk score model based on pancreatic texture to predict postoperative pancreatic fistula after pancreaticoduodenectomy. Int J Surg 48:189–194
Sugimoto M, Takahashi S, Kojima M, Kobayashi T, Gotohda N, Konishi M (2017) In patients with a soft pancreas, a thick parenchyma, a small duct, and fatty infiltration are significant risks for pancreatic fistula after pancreaticoduodenectomy. J Gastrointest Surg 21(5):846–854
Peng Y-P, Zhu X-L, Yin L-D, Zhu Y, Wei J-S, Wu J-L et al (2017) Risk factors of postoperative pancreatic fistula in patients after distal pancreatectomy: a systematic review and meta-analysis. Sci Rep 7(1):185
Wellner UF, Kayser G, Lapshyn H, Sick O, Makowiec F, Höppner J et al (2010) A simple scoring system based on clinical factors related to pancreatic texture predicts postoperative pancreatic fistula preoperatively. HPB 12(10):696–702
Callery MP, Pratt WB, Kent TS, Chaikof EL, Vollmer CM (2013) A prospectively validated clinical risk score accurately predicts pancreatic fistula after pancreatoduodenectomy. J Am Coll Surg 216(1):1–14
Lin JW, Cameron JL, Yeo CJ, Riall TS, Lillemoe KD (2004) Risk factors and outcomes in postpancreaticoduodenectomy pancreaticocutaneous fistula. J Gastrointest Surg 8(8):951–959
Mathur A, Pitt HA, Marine M, Saxena R, Schmidt CM, Howard TJ et al (2007) Fatty pancreas. Ann Surg 246(6):1058–1064
Pratt WB, Callery MP, Vollmer CM (2008) Risk prediction for development of pancreatic fistula using the ISGPF classification scheme. World J Surg 32(3):419–428
Gaujoux S, Cortes A, Couvelard A, Noullet S, Clavel L, Rebours V et al (2010) Fatty pancreas and increased body mass index are risk factors of pancreatic fistula after pancreaticoduodenectomy. Surgery 148(1):15–23
Yamamoto Y, Sakamoto Y, Nara S, Esaki M, Shimada K, Kosuge T (2011) A preoperative predictive scoring system for postoperative pancreatic fistula after pancreaticoduodenectomy. World J Surg 35(12):2747–2755
Roberts KJ, Hodson J, Mehrzad H, Marudanayagam R, Sutcliffe RP, Muiesan P et al (2014) A preoperative predictive score of pancreatic fistula following pancreatoduodenectomy. HPB 16(7):620–628
Chen J-Y, Feng J, Wang X-Q, Cai S-W, Dong J-H, Chen Y-L (2015) Risk scoring system and predictor for clinically relevant pancreatic fistula after pancreaticoduodenectomy. World J Gastroenterol 21(19):5926–5933
McMillan MT, Soi S, Asbun HJ, Ball CG, Bassi C, Beane JD et al (2016) Risk-adjusted outcomes of clinically relevant pancreatic fistula following pancreatoduodenectomy. Ann Surg 264(2):344–352
Sugimoto M, Takahashi S, Kojima M, Gotohda N, Kato Y, Kawano S et al (2014) What is the nature of pancreatic consistency? Assessment of the elastic modulus of the pancreas and comparison with tactile sensation, histology, and occurrence of postoperative pancreatic fistula after pancreaticoduodenectomy. Surgery 156(5):1204–1211
Kawada N, Tanaka S (2016) Elastography for the pancreas: current status and future perspective. World J Gastroenterol 22(14):3712–3724
Lee TK, Kang CM, Park M-S, Choi SH, Chung Y-E, Choi JY et al (2014) Prediction of postoperative pancreatic fistulas after pancreatectomy: assessment with acoustic radiation force impulse elastography. J Ultrasound Med 33(5):781–786
Harada N, Ishizawa T, Inoue Y, Aoki T, Sakamoto Y, Hasegawa K et al (2014) Acoustic radiation force impulse imaging of the pancreas for estimation of pathologic fibrosis and risk of postoperative pancreatic fistula. J Am Coll Surg 219(5):887–94.e5
Hatano M, Watanabe J, Kushihata F, Tohyama T, Kuroda T, Koizumi M et al (2015) Quantification of pancreatic stiffness on intraoperative ultrasound elastography and evaluation of its relationship with postoperative pancreatic fistula. Int Surg 100(3):497–502
D’Onofrio M, Tremolada G, De Robertis R, Crosara S, Ciaravino V, Cardobi N et al (2017) Prevent pancreatic fistula after pancreatoduodenectomy: possible role of ultrasound elastography. Dig Surg 35:164
Harada N, Yoshizumi T, Maeda T, Kayashima H, Ikegami T, Harimoto N et al (2017) Preoperative pancreatic stiffness by real-time tissue elastography to predict pancreatic fistula after pancreaticoduodenectomy. Anticancer Res 37(4):1909–1915
Fujita Y, Kitago M, Abe T, Itano O, Shinoda M, Abe Y et al (2018) Evaluation of pancreatic fibrosis with acoustic radiation force impulse imaging and automated quantification of pancreatic tissue components. Pancreas 47:1277–1282
Hirooka Y, Kuwahara T, Irisawa A, Itokawa F, Uchida H, Sasahira N et al (2015) JSUM ultrasound elastography practice guidelines: pancreas. J Med Ultrason 42(2):151–174
Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas J-M, Gilja O et al (2013) EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 2: clinical applications. Ultraschall der Medizin Eur J Ultrasound 34(3):238–253
Bassi C, Marchegiani G, Dervenis C, Sarr M, Abu Hilal M, Adham M et al (2017) The 2016 update of the International Study Group (ISGPS) definition and grading of postoperative pancreatic fistula: 11 Years after. Surgery 161(3):584–591
Wu R, Zou L, Yao M, Xu G, Zhao L, Xu H et al (2015) A preliminary investigation of normal pancreas and acute pancreatitis elasticity using virtual touch tissue quantification (VTQ) imaging. Med Sci Monit 21:1693–1699
Zaro R, Lupsor-Platon M, Cheviet A, Badea R (2016) The pursuit of normal reference values of pancreas stiffness by using acoustic radiation force impulse (ARFI) elastography. Med Ultrason 18(4):425
Arda K, Ciledag N, Aktas E, Arıbas BK, Köse K (2011) Quantitative assessment of normal soft-tissue elasticity using shear-wave ultrasound elastography. Am J Roentgenol 197(3):532–536
Bamber J, Cosgrove D, Dietrich C, Fromageau J, Bojunga J, Calliada F et al (2013) EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography. Part 1: basic principles and technology. Ultraschall der Medizin Eur J Ultrasound 34(2):169–184
Piscaglia F, Salvatore V, Mulazzani L, Cantisani V, Colecchia A, Di Donato R et al (2017) Differences in liver stiffness values obtained with new ultrasound elastography machines and fibroscan: a comparative study. Dig Liver Dis 49:802–808
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Giovanni Marasco and all co-authors declared that they not have a conflict of interest and they did not received funding for the manuscript.
Ethical approval
This study has been approved by the Institutional ethic committee of our hospital, and was in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Research involving human participants and/or animals
This study does not contain any studies with animals performed by any of the authors.
Informed consent
Informed consent was obtained from each patient involved in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Marasco, G., Ricci, C., Grasso, V. et al. Pancreatic ultrasound elastography is not useful to predict the risk of pancreatic fistulas after pancreatic resection. Updates Surg 72, 1081–1087 (2020). https://doi.org/10.1007/s13304-020-00748-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13304-020-00748-z