Abstract
Introduction
The role of mobile technology in patient-reported outcomes (PRO) and glycemic control in adults with type 1 diabetes (T1D) needs further evaluation.
Methods
The single-center, prospective, 6-month, open-label, investigator-initiated study randomized 100 subjects with T1D in a 1:1 fashion to a control group using self-monitoring of blood glucose (SMBG) with Accu-Chek Nano® and an intervention group using SMBG with iPhone plus glucose meter (iBGStar®). The primary endpoint was the change in PRO (hypoglycemia fear score, behavior and worry subscores). Secondary outcomes were the improvement in glycemic variability indices and the reduction in A1c values.
Results
Baseline demographics and glycosylated hemoglobin (A1c) values were similar in the two groups. There was a significant decrease in A1c value at 6 months in iBGStar® group compared to the control group (−0.16 vs. −0.51, p = 0.04). The total insulin dose increased significantly in the iBGStar® group at 3 months but did not change at 6 months. The hypoglycemia fear scale (PRO) improved in both groups at 6 months (−1.4 ± 10.0 vs. −3.9 ± 12.5, p = 0.32).
Conclusion
The use of iBGStar® resulted in better glycemic control and improvement in some PRO (hypoglycemia fear and behavior scores) compared to the control group at 6 months with no increased risk of hypoglycemia.
Clinical trial registration
ClinicalTrials.gov: NCT01825382.
Funding
Sanofi.
Similar content being viewed by others
Introduction
With increasing incidence of type 1 diabetes (T1D) by 2–5% annually, 5 million people are estimated to have T1D by 2050 in the USA [1, 2]. Though intensive insulin therapy (IIT) has been shown to reduce the risk of micro- and macrovascular complications of diabetes, it is associated with a significant increase in the risk for severe hypoglycemia [3]. Even fear of hypoglycemia itself poses a significant psychological factor in patients with T1D, preventing them from achieving good glycemic control [4]. Despite increases in diabetes care, less than 20% of patients with T1D achieve good glycemic control [as defined by a glycosylated hemoglobin (A1c) of less than 7%] [5].
Self-monitoring of blood glucose (SMBG) is a valuable tool for decision-making for both patients and clinicians. Frequent SMBG has been shown to improve A1c and reduce hypoglycemia and hypoglycemia fear in patients with type 1 diabetes [6, 7]. The American Diabetes Association (ADA) recommends that patients whose medication regimen includes multiple daily insulin injections or insulin pumps should test their blood glucose three times or more per day [8]. However, not all patients with diabetes test blood glucose three times or more a day [5]. Hurdles in poor adherence to SMBG include (a) inaccurate meters, (b) big and bulkier devices, (c) need to poke a finger multiple times, (d) need to carry an additional device all the time, and (e) paper log book entry [6, 7, 9, 10]. These difficulties result in poor compliance and inadequate glucose control with wide glucose excursions.
The ubiquity of smartphones and increasing availability of diabetes management mobile applications present a potential method to reduce the daily time and effort required to perform SMBG tasks and share data with a healthcare provider. Small studies have shown improvement in glycemic control with the use of electronic log book and Internet-based glucose monitoring systems [11]. However, these studies are limited by small sample size and short duration and no reporting of hypoglycemic events [11]. Using mobile technology to facilitate the review of blood glucose data by both patients and providers could provide an opportunity to reduce glycemic variability and its associated complications [12]. The iBGStar® system is a blood glucose meter that attaches to an iPhone as a peripheral device. Using the iBGStar® with the Diabetes Manager App, a user’s iPhone can function as a glucometer. The Diabetes Manager App takes advantage of the existing user interface and communication capabilities of the iPhone to provide IMBG functionality on a mobile device. This study examined the effect of iBGStar® in combination with Diabetes Manager mobile application on patient-reported outcomes (PRO) and glycemic control in adults with T1D.
Methods
Patient Selection
This study was a single-center, prospective, randomized, open-label, and conducted at the Barbara Davis Center for Diabetes. The protocol was approved by Colorado Multiple Institutional Review Board at the University of Colorado. Adults (≥18 years) with T1D of more than 1-year duration and A1c below 10% were enrolled. Pregnant women and those who intended to conceive during the study period were excluded. Participants with T1D on systemic or inhaled steroids, history of severe hypoglycemia in the last 6 months, history of anemia or hemoglobinopathies, history of pancreatitis, history of skin disease, or allergy to adhesives and bandages precluding continuous glucose monitor (CGM) use were also excluded from the study.
Study Design, Treatment, and Follow-Up
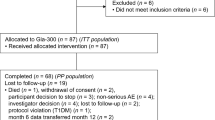
Subjects were randomized on a 1:1 basis to either the control group or intervention group using stratified block randomization based on a screening A1c <8.5 or ≥8.5 to reduce the possibility of sampling error and ensure that randomization resulted in similar A1c results in each group. The control group were provided with Accu-Chek Nano® meters and trained on their use at baseline and reinforced at week 1. The iBGStar®, an iPhone 4 or 4S, and the Diabetes Manager App were provided to the intervention group. All subjects were provided with a Dexcom SEVEN Plus® blinded CGM sensor. The provider maintained contact with the subjects by electronic communication (email, text, or phone) every 7–14 days during the study. Subjects in the control group were encouraged to contact their provider as needed by traditional communication (email, fax, or phone). Those in the intervention group were invited to contact the research site if their blood glucose reading was below 60 or above 300 mg/dL using the Diabetes Manager App, which sends a notification text from the iPhone to the provider. All diabetes treatment decisions were based on SMBG readings from either the iBGStar® or Accu-Chek Nano® glucometer, depending on group assignment. Subjects were trained to use glucose log books and instructed to check blood glucose at least three times per day during the study.
All subjects had similar clinic and phone visits for 3 months, with a 3-month extension. A total of eight visits were required—a screening visit, four in-clinic visits, and three phone calls. A Dexcom SEVEN Plus® blinded CGM sensor was inserted each clinic visit starting from visit 2 for a total of four visits (for four separate 7-day periods of blinded CGM at visits 2, 4, 6, and 8). During the week of blinded CGM use, subjects were not allowed to use their own real-time CGMs. Subjects were instructed not to take acetaminophen during blinded CGM period as per the label.
All the participants were trained on glucose diaries and were asked to check blood glucose at least three times a day during the study period. All diabetes treatment decisions were based on SMBG readings from iBGStar® in the intervention group and Accu-Chek Nano® glucose meter in the control group. The study design and visits are shown in Fig. 1. All participants completed the study and attended to all visits.
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all participants for being included in the study.
Outcome Measurements
A1C, complete metabolic panel, and complete cell counts were measured at baseline, 1, 3, and 6 months. A1c was measured by DCA 2000. Data on insulin dose was collected from participants by self-report based on logbook entries. The PRO directly describes the patient’s perception of a disease and its treatment without the interpretation of responses by a physician. Hypoglycemia perspective questionnaire and hypoglycemia fear score are the most common tools used for hypoglycemia assessment. Hypoglycemia fear was measured using a 27-question instrument (score range 27–135) with subscales for behavior (10 questions) and worry (17 questions) at the screening and 3- and 6-month visits [13] (Supplement 1). Measurements of average blood glucose and glucose variability were carried out from blinded CGM tracings.
Statistical Analysis
The analysis was conducted with the intent-to-treat concept. The primary efficacy endpoint was patient-reported outcomes, including the change in the hypoglycemia fear questionnaire score from baseline to 3 and 6 months. Secondary outcomes were the improvement in glycemic variability indices and the reduction in A1c values. Improvement in glycemic control was measured as the difference in the change in A1c laboratory values of the two arms of the study between baseline and 3 and 6 months. Changes in the primary and secondary efficacy endpoints were assessed using paired t tests examining changes from baseline to 3 months and baseline to 6 months. Linear regression mixed models were used to assess changes in the primary and secondary endpoints over time, using repeated measures analyses. As this was a pilot study, formal power calculations were not performed for the primary or secondary endpoints. Statistical significance was defined as p < 0.05. All analyses were performed using SAS, version 9.4 (SAS Institute, Cary, NC, USA).
Results
Fifty participants with T1D were randomized to the intervention arm (iBGStar®), and an equal number of participants were randomized to the control group (Accu-Chek Nano®). The mean age, duration of diabetes, body mass index (BMI), A1c level, the number of self-monitored blood glucose (SMBG) measures, daily insulin basal and bolus dose, and total daily insulin dose per day were similar between control and intervention groups (Table 1). Similarly, there was no difference in hypoglycemia fear scale, behavior scale, and worry scale between the control and intervention groups at baseline (Table 1).
As shown in Table 2, there were decreases in the overall hypoglycemia fear score in both groups after 3 months, but these decreases were no longer significant at 6 months. There was no difference in the magnitude of the changes in hypoglycemia fear in the study group at either 3 or 6 months. When examined by subscore, hypoglycemia fear behavior score decreased in only the iBGStar® group at 3 months, but this change did not persist at 6 months. The hypoglycemia fear worry score declined in both groups at 3 months and remained significantly reduced only in the control group at 6 months. However, the changes in scores for both subscales did not differ by the study group. The total insulin dose increased significantly in the iBGStar® group at 3 months but did not change at 6 months. There was no statistically significant difference between iBGStar® and control groups regarding the number of hypoglycemic events and the average number of SMBG/day.
There was a decrease in A1c among both the control and iBGStar® groups at 3 months, although the amount of change in A1c was not different between groups (−0.21 vs. −0.4, p = 0.20) (Fig. 2). However, at 6 months, there was a significant decrease in A1c from baseline only in the iBGStar® group, and the amount of change was significantly greater in the iBGStar group than in the control group (−0.16 vs. −0.51, p = 0.04) (Fig. 2). The percentage of time spent in hypoglycemia (<70 mg/dl) did not differ by study group (Fig. 3). There was no BMI change at 3 and 6 months in groups.
In addition to the univariate analyses, linear mixed modeling was used to examine the change in primary and secondary endpoints over the three study visits using a repeated measures analysis. Hypoglycemia fear score was examined, adjusting for group, age, diabetes duration, sex, BMI, daily insulin dose per kilogram body weight, and A1c. There remained no significant differences by group either overall (p = 0.77) or across visits (p = 0.55), but hypoglycemia fear score was significantly lower in men than in women (estimate −5.9, p = 0.046) and was negatively associated with insulin dose (estimate −6.2, p = 0.04). Hypoglycemia fear score was not associated with age (p = 0.88), diabetes duration (p = 0.50), BMI (p = 0.68), or A1c (p = 0.41) (Table 3).
Similarly, linear mixed modeling was used to examine change in A1c across the three visits, adjusted for group, age, diabetes duration, sex, BMI, and daily insulin dose per kilogram body weight. In this model, there remained no significant difference by study group either overall (p = 0.60) or across visits (p = 0.14), although the change in A1c was significantly associated with insulin dose (estimate 0.5193, p = 0.02). There was no association between A1c across study visits and age (p = 0.22), diabetes duration (p = 0.76), sex (p = 0.21), or BMI (p = 0.76) (Table 4).
In a post-study survey, 88% of the subjects who used iBGStar® were satisfied with the system. Seventy-five percent of the subjects found the iBGStar® system with the Diabetes Manager App on the iPhone easier than their conventional glucometer for managing their diabetes. Diabetes Manager App was found to be very user-friendly by about 90% of the subjects.
Discussion
Blood glucose monitoring is an important part of diabetes management, especially in patients on insulin. The Diabetes Control and Complications Trial showed that frequent blood glucose monitoring along with intensive therapy is required to maintain tight glycemic control [14].
Communication errors between the patients and the providers, absence of documentation of blood glucose results, and failure of downloading glucometers in care centers are common difficulties in diabetes care. New technologies require a better understanding by both patients and healthcare workers [15]. An accurate and convenient way for routine blood glucose monitoring and reporting is essential for following the treatment and making necessary therapeutic changes. Integration of smartphones into our life brought new opportunities in healthcare. The use of the Diabetes Manager App with the iBGStar® facilitated electronic communication between participants and providers. The precision of iBGStar® was shown previously in an in vitro diagnostic device study [16]. Diabetes Manager App allowed participants to upload and review SMBG data on an iPhone. Even though there was no significant difference between hypoglycemia fear or behavior scales, the subjects indicated that they felt more comfortable using the iBGStar® system. Ease of use and convenience probably resulted in greater patient satisfaction at the post-study survey. The app allowed the patient to filter and dynamically interact with log book data, graph trends, and view statistics. Rather than searching through a report, the user can take advantage of features in the app to produce specific queries related to their needs.
In our study, using the iBGStar® system improved A1c at 3 months which was maintained at 6 months when compared to the control group. Increased insulin requirements may partially explain the decrease of A1C in the iBGStar® group.
This was a pilot study. One of the strengths of this study was that no one had previously evaluated the role of mobile technology in diabetes care. Our goal was to learn from this study and plan for a much larger study using social media in the future after implementing changes that would be learned from this pilot study. We had objective measures of patient-reported outcomes and treatment satisfaction using validated tools.
Limitations of this study were that this was a short-term (6 months) study in a single center and we only focused on hypoglycemia risk at CGM and we did not analyze the other blood glucose variabilities. Therefore, the results may not be generalized.
Conclusions
The use of iBGStar® in combination with Diabetes Manager mobile application improved some PRO (hypoglycemia fear and behavior score) and glycemic control at 6 months without an increased risk of hypoglycemia. Further studies would be required to determine the effects of iBGStar® system and Diabetes Manager App in the long term.
References
Dabelea D, Mayer-Davis EJ, Saydah S, et al. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014;311(17):1778–86.
Imperatore G, Boyle JP, Thompson TJ, et al. Projections of type 1 and type 2 diabetes burden in the U.S. population aged <20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care. 2012;35(12):2515–20.
Shah VN, Shoskes A, Tawfik B, Garg SK. Closed-loop system in the management of diabetes: past, present, and future. Diabetes Technol Ther. 2014;16(8):477–90.
Majidi S, Driscoll KA, Raymond JK. Anxiety in children and adolescents with type 1 diabetes. Curr Diab Rep. 2015;15(8):47.
Miller KM, Foster NC, Beck RW, et al. Current state of type 1 diabetes treatment in the U.S.: updated data from the T1D exchange clinic registry. Diabetes Care. 2015;38(6):971–8.
Miller KM, Beck RW, Bergenstal RM, et al. Evidence of a strong association between frequency of self-monitoring of blood glucose and hemoglobin A1c levels in T1D exchange clinic registry participants. Diabetes Care. 2013;36(7):2009–14.
Garg S, Hirsch IB. Self-monitoring of blood glucose. Int J Clin Pract Suppl. 2010;166:1–10.
American Diabetes Association. Standards of medical care in diabetes-2015. Diabetes Care. 2015;38:S1–90.
Spollet GR. Self-monitoring of blood glucose: an underutilized tool. Clin Diabetes. 2010;28:127–9.
Moser EG, Morris AA, Garg SK. Emerging diabetes therapies and technologies. Diabetes Res Clin Pract. 2012;97(1):16–26.
Kirwan M, Vandelanotte C, Fenning A, Duncan MJ. Diabetes self-management smartphone application for adults with type 1 diabetes: randomized controlled trial. J Med Int Res. 2013;15(11):e235.
Overland J, Abousleiman J, Chronopoulos A, Leader N, Molyneaux L, Gilfillan C. Improving self-monitoring of blood glucose among adults with type 1 diabetes: results of the Mobile™ study. Diabetes Ther. 2014;5(2):557–65.
Cox DJ, Irvine A, Gonder-Frederick L, Nowacek G, Butterfield J. Fear of hypoglycemia: quantification, validation, and utilization. Diabetes Care. 1987;10(5):617–21.
Nathan DM, Genuth S, Lachin J, et al. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–86.
Garg SK. Role of emerging new technologies. Diabetes Technol Ther. 2008;10(5):413–4.
Ramljak S, Musholt PB, Schipper C, et al. The precision study: examining the inter- and intra-assay variability of replicate measurements of BGStar, iBGStar and 12 other blood glucose monitors. Expert Opin Med Diagn. 2013;7(6):511–6.
Acknowledgements
Sponsorship for this study was funded by Sanofi as an Investigator Sponsored Study. Article processing charges were funded by the authors. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work, and have given final approval for the version to be published. All authors had full access to all the data in this study and took complete responsibility for the integrity of the data and accuracy of the data analysis.
Disclosures
Halis K. Akturk, Christie Beatson, and Janet K Snell-Bergeon have nothing to disclose. Viral N. Shah’s employer received research Grants from Sanofi, T1D Exchange program. Viral N. Shah had received speaking fees from the Dexcom Inc. Satish K. Garg had research Grants from Eli Lilly, Novo-Nordisk, Merck, Lexicon, Medtronic, Dario, NCI, T1D Exchange, NIDDK, JDRF, and Sanofi. Satish K. Garg was on the advisory board and received consulting and travel fees from Medtronic, Roche, Merck, Lexicon, Novo-Nordisk, Sanofi, JNJ, Mannkind, and Eli Lilly. None of the authors have any stocks or equity in any device or pharmaceutical company.
Compliance with Ethics Guidelines
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1964, as revised in 2013. Informed consent was obtained from all participants for being included in the study. The protocol was approved by Colorado Multiple Institutional Review Board at the University of Colorado, Aurora, CO, USA.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content To view enhanced content for this article go to http://www.medengine.com/Redeem/4598F0606F7F5B58.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Garg, S.K., Shah, V.N., Akturk, H.K. et al. Role of Mobile Technology to Improve Diabetes Care in Adults with Type 1 Diabetes: The Remote-T1D Study iBGStar® in Type 1 Diabetes Management. Diabetes Ther 8, 811–819 (2017). https://doi.org/10.1007/s13300-017-0272-5
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13300-017-0272-5