Abstract
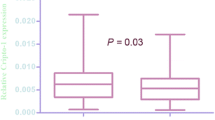
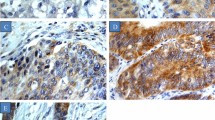
The present study was to investigate the expression and prognostic value of constitutive photomorphogenic 1 (COP1) in bladder cancer. In our study, real-time quantitative PCR (RT-PCR) was performed to detect 10 pairs of fresh bladder cancer (BCa) and adjacent noncancerous tissues. In addition, immunohistochemistry was utilized to detect the expression of COP1 in 174 clinical bladder cancer samples. What is more, the correlation of COP1 expression and clinicopathological features and clinical outcomes were analyzed. The expression levels of COP1 in clinical bladder cancer were much higher than that in paired adjacent noncancerous tissues (p < 0.0001). High expression of COP1 was closely related with differentiation (p = 0.040) and recurrence (p = 0.001) of patients with bladder cancer. Kaplan-Meier analysis revealed that the expression of COP1 was closely correlated with overall survival (p = 0.048) of bladder cancer, while, recurrence-free survival (p = 0.201). Moreover, Cox multivariate regression analyses showed that COP1 expression was an independent predictor of overall survival (OS; p = 0.027, hazard ratio = 2.127, confidence interval 0.814 to 9.736). Based on our data, the present study suggests that high expression of COP1 may be a novel biological indicator for evaluation of poor prognosis in bladder cancer.



Similar content being viewed by others
References
Stenzl A, Cowan NC, De Santis M, et al. Treatment of muscle-invasive and metastatic bladder cancer: update of the EAU guidelines. Eur Urol. 2011;59(6):1009–18.
Zhu Z, Wang X, Shen Z, Lu Y, Zhong S, Xu C. Risk of bladder cancer in patients with diabetes mellitus: an updated meta-analysis of 36 observational studies. BMC Cancer. 2013;13:310.
Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer Journal international du cancer. 2015;136(5):E359–386.
van Rhijn BW, Burger M, Lotan Y, et al. Recurrence and progression of disease in non-muscle-invasive bladder cancer: from epidemiology to treatment strategy. Eur Urol. 2009;56(3):430–42.
Ather MH, Nazim SM. New and contemporary markers of prognosis in nonmuscle invasive urothelial cancer. Korean J Urology. 2015;56(8):553–64.
Oderda M, Ricceri F, Pisano F, et al. Prognostic factors including Ki-67 and p53 in Bacillus Calmette-Guerin-treated non-muscle-invasive bladder cancer: a prospective study. Urol Int. 2013;90(2):184–90.
Lokeshwar VB, Schroeder GL, Selzer MG, et al. Bladder tumor markers for monitoring recurrence and screening comparison of hyaluronic acid-hyaluronidase and BTA-Stat tests. Cancer. 2002;95(1):61–72.
Jones A, Crew J. Vascular endothelial growth factor and its correlation with superficial bladder cancer recurrence rates and stage progression. Urol Clin North Am. 2000;27(1):191–7.
Soloway MS, Briggman V, Carpinito GA, et al. Use of a new tumor marker, urinary NMP22, in the detection of occult or rapidly recurring transitional cell carcinoma of the urinary tract following surgical treatment. J Urol. 1996;156(2 Pt 1):363–7.
Deng XW, Caspar T, Quail PH. cop1: a regulatory locus involved in light-controlled development and gene expression in Arabidopsis. Genes Dev. 1991;5(7):1172–82.
Dornan D, Wertz I, Shimizu H, et al. The ubiquitin ligase COP1 is a critical negative regulator of p53. Nature. 2004;429(6987):86–92.
Li YF, Wang DD, Zhao BW, et al. High level of COP1 expression is associated with poor prognosis in primary gastric cancer. Int J Biol Sci. 2012;8(8):1168–77.
Dornan D, Bheddah S, Newton K, et al. COP1, the negative regulator of p53, is overexpressed in breast and ovarian adenocarcinomas. Cancer Res. 2004;64(20):7226–30.
Azemar MD, Comperat E, Richard F, Cussenot O, Roupret M. Bladder recurrence after surgery for upper urinary tract urothelial cell carcinoma: frequency, risk factors, and surveillance. Urol Oncol. 2011;29(2):130–6.
Corcoran CA, Huang Y, Sheikh MS. The p53 paddy wagon: COP1, Pirh2 and MDM2 are found resisting apoptosis and growth arrest. Cancer Biol Ther. 2004;3(8):721–5.
Mariani O, Brennetot C, Coindre JM, et al. JUN oncogene amplification and overexpression block adipocytic differentiation in highly aggressive sarcomas. Cancer Cell. 2007;11(4):361–74.
Wei W, Kaelin Jr WG. Good COP1 or bad COP1? In vivo veritas. J Clin Invest. 2011;121(4):1263–5.
Marine JC. Spotlight on the role of COP1 in tumorigenesis. Nat Rev Cancer. 2012;12(7):455–64.
Vitari AC, Leong KG, Newton K, et al. COP1 is a tumour suppressor that causes degradation of ETS transcription factors. Nature. 2011;474(7351):403–6.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no competing interests.
Additional information
Jianlong Li and Longwang Wang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Li, J., Wang, L., Xiao, R. et al. High expression of constitutive photomorphogenic 1 (COP1) is associated with poor prognosis in bladder cancer. Tumor Biol. 37, 8917–8922 (2016). https://doi.org/10.1007/s13277-015-4765-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-4765-4