Abstract
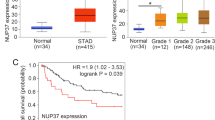
KPNβ1, also known as importin β, P97, is reported as one of soluble transport factors that mediates transportion of proteins and RNAs between the nucleus and cytoplasm in cellular process. Recent studies show that KPNβ1 is a tumor gene which is highly expressed in several malignant tumors such as ovarian cancer, cervical tumor, neck cancer, and lung cancer via promoting cell proliferation or inhibiting cell apoptotic pathways. However, the the role of KPNβ1 in gastric cancer remains unclear. In this study, Western blot and immunohistochemistrical analyses showed that KPNβ1 was significantly upregulated in clinical gastric cancer specimens compared with adjacent noncancerous tissues. KPNβ1 was positively correlated with tumor grade, Ki-67, and predicted poor prognosis of gastric cancer. More importantly, through starvation-refeeding model, CCK8 assay, flow cytometry, colony formation assays, the vitro studies demonstrated that KPNβ1 promoted proliferation of gastric cancer cells, while KPNβ1 knockdown led to decreased cell proliferation and arrested cell cycle at G1 phase. Furthermore, our results also indicated that KPNβ1 expression could result in docetaxel resistance. And, KPNβ1 could interact with Stat1, contributed to its nucleus import in gastric cancer cells. These findings provided a novel promising therapeutic targets for clinical treatment against human gastric cancer.







Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. CA Cancer J Clin. 2012;62:10–29.
Zhang D, Sun L, Zhu H, Wang L, Wu W, Xie J, et al. Microglial lox-1 reacts with extracellular hsp60 to bridge neuroinflammation and neurotoxicity. Neurochem Int. 2012;61:1021–35.
Cao Y, DePinho RA, Ernst M, Vousden K. Cancer research: past, present and future. Nat Rev Cancer. 2011;11:749–54.
de Martel C, Forman D, Plummer M. Gastric cancer: epidemiology and risk factors. Gastroenterol Clin N Am. 2013;42:219–40.
Gorlich D, Kutay U. Transport between the cell nucleus and the cytoplasm. Annu Rev Cell Dev Biol. 1999;15:607–60.
Kutay U, Izaurralde E, Bischoff FR, Mattaj IW, Gorlich D. Dominant-negative mutants of importin-beta block multiple pathways of import and export through the nuclear pore complex. EMBO J. 1997;16:1153–63.
Kau TR, Way JC, Silver PA. Nuclear transport and cancer: from mechanism to intervention. Nat Rev Cancer. 2004;4:106–17.
Harel A, Forbes DJ. Importin beta: conducting a much larger cellular symphony. Mol Cell. 2004;16:319–30.
van der Watt PJ, Stowell CL, Leaner VD. The nuclear import receptor kpnbeta1 and its potential as an anticancer therapeutic target. Crit Rev Eukaryot Gene Expr. 2013;23:1–10.
Moroianu J. Distinct nuclear import and export pathways mediated by members of the karyopherin beta family. J Cell Biochem. 1998;70:231–9.
Quan Y, Ji ZL, Wang X, Tartakoff AM, Tao T. Evolutionary and transcriptional analysis of karyopherin beta superfamily proteins. Mol Cell Proteomics. 2008;7:1254–69.
van der Watt PJ, Ngarande E, Leaner VD. Overexpression of kpnbeta1 and kpnalpha2 importin proteins in cancer derives from deregulated e2f activity. PLoS One. 2011;6:e27723.
van der Watt PJ, Maske CP, Hendricks DT, Parker MI, Denny L, Govender D, et al. The karyopherin proteins, crm1 and karyopherin beta1, are overexpressed in cervical cancer and are critical for cancer cell survival and proliferation. Int J Cancer. 2009;124:1829–40.
Martens-de Kemp SR, Nagel R, Stigter-van Walsum M, van der Meulen IH, van Beusechem VW, Braakhuis BJ, et al. Functional genetic screens identify genes essential for tumor cell survival in head and neck and lung cancer. Clin Cancer Res. 2013;19:1994–2003.
Ji Y, Tao T, Cheng C, Yang H, Wang Y, Yang J, et al. Ssecks is a suppressor in schwann cell differentiation and myelination. Neurochem Res. 2010;35:219–26.
Liu Y, Chen Y, Lu X, Wang Y, Duan Y, Cheng C, et al. Scyl1bp1 modulates neurite outgrowth and regeneration by regulating the mdm2/p53 pathway. Mol Biol Cell. 2012;23:4506–14.
Roth AD, Ajani J. Docetaxel-based chemotherapy in the treatment of gastric cancer. Ann Oncol. 2003;14 Suppl 2:ii41–4.
Ajani JA. Docetaxel for gastric and esophageal carcinomas. Oncology. 2002;16:89–96.
Adamkova L, Souckova K, Kovarik J. Transcription protein stat1: biology and relation to cancer. Folia Biol. 2007;53:1–6.
Deng H, Zhen H, Fu Z, Huang X, Zhou H, Liu L. The antagonistic effect between stat1 and survivin and its clinical significance in gastric cancer. Oncol Lett. 2012;3:193–9.
Milne AN, Carneiro F, O’Morain C, Offerhaus GJ. Nature meets nurture: molecular genetics of gastric cancer. Hum Genet. 2009;126:615–28.
Zhang P, Yang X, Ma X, Ingram DR, Lazar AJ, Torres KE, et al. Antitumor effects of pharmacological ezh2 inhibition on malignant peripheral nerve sheath tumor through the mir-30a and kpnb1 pathway. Mol Cancer. 2015;14:55.
Liang P, Zhang H, Wang G, Li S, Cong S, Luo Y, et al. Kpnb1, xpo7 and ipo8 mediate the translocation ofnf-kappab/p65 into the nucleus. Traffic. 2013;14:1132–43.
Perlson E, Hanz S, Ben-Yaakov K, Segal-Ruder Y, Seger R, Fainzilber M. Vimentin-dependent spatial translocation of an activated map kinase in injured nerve. Neuron. 2005;45:715–26.
Malki S, Nef S, Notarnicola C, Thevenet L, Gasca S, Mejean C, et al. Prostaglandin d2 induces nuclear import of the sex-determining factor sox9 via its camp-pka phosphorylation. EMBO J. 2005;24:1798–809.
Kurisaki A, Kose S, Yoneda Y, Heldin CH, Moustakas A. Transforming growth factor-beta induces nuclear import of smad3 in an importin-beta1 and ran-dependent manner. Mol Biol Cell. 2001;12:1079–91.
Bowman T, Garcia R, Turkson J, Jove R. Stats in oncogenesis. Oncogene. 2000;19:2474–88.
Stronach EA, Alfraidi A, Rama N, Datler C, Studd JB, Agarwal R, et al. Hdac4-regulated stat1 activation mediates platinum resistance in ovarian cancer. Cancer Res. 2011;71:4412–22.
McDermott U, Longley DB, Galligan L, Allen W, Wilson T, Johnston PG. Effect of p53 status and stat1 on chemotherapy-induced, fas-mediated apoptosis in colorectal cancer. Cancer Res. 2005;65:8951–60.
Gooch JL, Herrera RE, Yee D. The role of p21 in interferon gamma-mediated growth inhibition of human breast cancer cells. Cell Growth Differ. 2000;11:335–42.
Acknowledgments
This work was supported by the National Natural Science Foundation of China (No.81302285, No. 81402015); the Natural Science Foundation of Nantong University (No.12Z009).
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Jia Zhu and Yingying Wang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhu, J., Wang, Y., Huang, H. et al. Upregulation of KPNβ1 in gastric cancer cell promotes tumor cell proliferation and predicts poor prognosis. Tumor Biol. 37, 661–672 (2016). https://doi.org/10.1007/s13277-015-3839-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-015-3839-7