Abstract
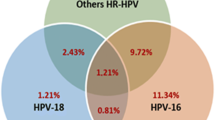
We have studied an automated in situ hybridization (ISH) method as a possible alternative approach for detecting high-risk human papillomavirus (HPV) in monolayer (ThinPrep) cervico-vaginal samples, comparing the results with those obtained by polymerase chain reaction (PCR) using consensus primers and studying the relationship between the ISH staining pattern and the viral integration in HPV 16-positive cases. Eighty atypical squamous cells of undetermined significance (ASCUS) and low-grade squamous intraepithelial lesion (LSIL) cases were used for our purposes. The patients were monitored through periodic cytologies. ISH with was performed with an automated Ventana System, analysis by PCR was performed with consensus primers and integration of HPV16 was performed by realtime PCR analyzing E2 and E6 genes. Additionally, 27 HSIL cases were also studied to observe the ISH staining patterns. HPV infection was detected by ISH in 21.7% of the ASCUS cases and 55.8% of the LSIL cases. Two distinct staining patterns were observed: multipunctated (MP) and diffuse (DI). In some cases, a mixed pattern (MP + DI) was observed and these cases were considered as MP. The MP pattern increased with the degree of lesion and seemed to have a prognostic value in ASCUS/LSIL cases. The lesion in MP pattern cases persisted throughout the entire study in 77% of cases, whereas in cases with a DI staining pattern, only 41% of them showed persistence of the lesion (p < 0.001). No correlation was found between HPV integration and the ISH staining pattern. Given the lower sensitivity and negative predictive value of ISH and its incapacity to demonstrate the integration of high-risk HPV in ASCUS and LSIL cases using liquid-based cytology, we do not recommend this technique for the triage of ASCUS and LSIL cases.



Similar content being viewed by others
References
The Atypical Squamous Cells of Undetermined Significance/Low Grade Squamous Intraepithelial Lesions Triage Study (ALTS) Group. Human papillomavirus testing for triage of women with cytology evidence of low-grade squamous intraepithelial lesions. Baseline data from a randomized trial. J Natl Cancer Inst. 2000;92(5):397–402.
Ring M, Bolger N, O’Donell M, Malkin A, Bermingham N, Akpan E, et al. Evaluation of liquid-based cytology in cervical screening of high-risk populations: a split study of colposcopy and genito-urinary medicine populations. Cytopathology. 2002;13:152–9.
Schorge JO, Hossein Saboorian M, Hynan L, Ashfaq R. ThinPrep detection of cervical and endometrial adenocarcinoma. A retrospective cohort study. Cancer (Cancer Cytopathol). 2002;96:338–43.
Klinkhamer PJJM, Meerding WJ, Rosier PEWM, Hanselaar AGJM. Liquid- based cervical cytology. A review of the literature with methods of evidence-based medicine. Cancer (Cancer Cytopathol). 2003;99:263–71.
Bolick DR. Laboratory implementation of human papillomavirus testing. Arch Pathol Lab Med. 2003;127:984–90.
Baunoch DA. In search of a paradigm: molecular and morphologic methods for human papillomavirus. Adv Adm Lab. 2001;10(5):1–10.
Hopman AHN, Theelen W, Hommelberg PPH, Kamps MAF, Herrington CS, Morrison LE, et al. Genomic integration of oncogenic HPV and gain of the human telomerase gene TERC at 3q26 are strongly associated events in the progression of uterine cervical dysplasia to invasive cancer. J Pathol. 2006;210:412–9.
Algeciras-Schmnich A, Policht F, Sitailo S, Song M, Morrison L, Sokolova I. Evaluation of quality and staining pattern of HPV infected epithelial cells in thin-layer cerviucal specimens using optimized HPV-Card assay. Cancer (Cancer Cytopathol). 2007;111:330–8.
Cavuslu S, Mant C, Starkey WG, Bible JM, Biswas C, Kell B, et al. Analytic sensitivities of hybrid-capture, consensus and type-specific polymerase chain reactions for the detection of human papillomavirus type 16DNA. J Med Virol. 1996;49(4):319–24.
Vernon SD, Unger ER, Williams D. Comparison of human papillomavirus detection and typing by cycle sequencing, line brotting, and hybrid capture. J Clin Microbiol. 2000;38(2):651–5.
Kosel S, Burggraf S, Mommsen J, Engelhardt W, Olgemoller B. Type-specific detection of human papillomaviruses in a routine laboratory setting-improved sensitivity and specificity of PCR and sequence analysis compared to direct hybridisation. Clin Chem Lab Med. 2003;41(6):787–91.
Nuovo GJ. Detection of human papillomavirus in papanicolau smears: correlation with pathologic findings and clinical outcome. Diagn Mol Pathol. 1998;7(3):158–63.
Layfiel LJ, HPV QN. DNA, testing in the triage of atypical squamous cells of undetermined significance (ASCUS). Cost comparison of two methods. Diagn Cytopathol. 2005;33(2):138–43.
Qureshi MN, Rudelli RD, Tubbs RR, Biscotti CV, Layfield LJ. Role of HPV DNA testing in predicting cervical intraepithelial lesions: comparison of HC HPV and ISH HPV. Diagn Cytopathol. 2003;29:149–55.
Quredshi MN, Bolick D, Ringer PJ, Spagler FL, Zimmerman G. HPV testing in liquid cytology specimens: comparison of analytic sensitivity and specificity for in situ hybridization and chemiluminescent nucleic acid testing. Acta Cytol. 2005;49(2):120–6.
Stoler MH. HPV testing in cervical cytology practice. It’s all about choice. Acta Cytol. 2005;49:117–9.
Evans MF, Mount SL, Beatty BG, Cooper K. Biotinyl-tyramide-based in situ hybridization signal patterns distinguish human papillomavirus type and grade of cervical lntraepithelial neoplasia. Mod Pathol. 2002;15(12):1339–47.
Birner P, Bachtiary B, Dreier B, Schindi M, Joura EA, Breitenecker G, et al. Signal-amplified colorimetric in situ hybridization for assessment of human papillomavirus infection in cervical lesions. Mod Pathol. 2001;14(7):702–9.
Sano T, Hikino T, Niwa Y, Kashiwabara K, Oyama T, Pukuda T, et al. In situ hybridization with biotinylated tyramide amplification: detection of human papillomavirus DNA in cervical neoplastic lesions. Mod Pathol. 1998;11(1):19–23.
Nasar Qureshi M, Rudelli RD, Ringer P. Analysis of HPV in situ hybridization assay (INFORM HPV, Ventana Medical Systems Inc.) by the automated cellular imaging systems ACIS (ChromaVision Medical Systems Inc). Poster accepted for presentation in 2003 USCAP.
Tjalma WA, Wan Waes TR, Van den Eeden LE, Bogers JJ. Role of human papillomavirus in the carcinogenesis of squamous cell carcinoma and adenocarcinoma of the cervix. Best Pract Res Clin Obstet Gynaecol. 2005;19(4):469–83.
Gallo G, Bibbo M, Bagella L, Zamparelli A, Sanseverino F, Giovanoli MR, et al. Study of viral integration of HPV-16 in young patients with LSIL. J Clin Pathol. 2003;56(7):532–6.
Hopman AH, Kamps MA, Smedts F, Speel EJ, Herrington CS, Ramaekers FC. HPV in situ hybridization: impact of different protocols on the detection of integrated HPV. Int J Cancer. 2005;115(3):419–28.
Guo M, Gong Y, Deavers M, Silva ES, Jan YJ, Cogdell DE, et al. Evaluation of commercialized in situ hybridization assay for detecting HPB DNA in tissue specimens from patients with cervical intraepithelial neoplasia and cervical carcinoma. J Clin Microbiol. 2008;46(1):274–80.
De Marchi Triglia R, Metze K, Zeferino LC, de Lucci de Angelo Andrade LA. HPV in situ hibridization signal patterns as a marker for cervical intraepithelial neoplasia progression. Gynecol Oncol. 2009;112:114–8.
Conflicts of interest
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Alameda, F., Mariñoso, M.L., Bellosillo, B. et al. Detection of HPV by in situ hybridization in thin-layer (ThinPrep) cervicovaginal samples. Tumor Biol. 32, 603–609 (2011). https://doi.org/10.1007/s13277-011-0159-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13277-011-0159-4