Abstract
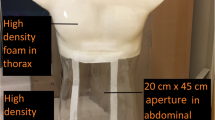
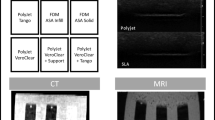
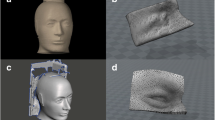
The fabrication of brachytherapy surface moulds is considered laborious and time consuming that often result in repeated attempts due to incorrect catheter positioning or the presence of air gaps. 3-dimensional printing using low-cost and reliable materials has allowed the rapid creation of patient-specific surface mould applicators to be achieved using patient imaging data obtained via CT scan. In this study we investigate whether an alternative approach using photogrammetry techniques can improve this process and how camera settings and object texture affect the reconstructions. Two humanoid phantoms, an anthropomorphic RANDO phantom and a Laerdal Little Anne CPR training manikin were used in this study. Both were imaged using a Nikon D5600 DSLR and Nokia 3.1 smartphone camera and reconstructed using Agisoft Metashape software. CT scans of both phantoms were taken as references for comparing the photogrammetry reconstructions. Models were reconstructed from different photo sets and assessed by distance to agreement with the CT models. Both phantoms were effectively reconstructed for most experiments. Increasing the number of photos used produced the better reconstructions while in general, reconstructions using video data were poor. The two phantoms were reconstructed at a similar quality. Background light that caused undesirable reflections significantly reduced reconstruction quality. Applying a non-reflective tape to the affected regions provided a suitable method for reducing their effects. Photogrammetry techniques were effectively able to reconstruct 3-dimensional models of both phantom. The camera settings and lighting did have a profound effect on the reconstruction quality and should be chosen appropriately depending on the scene.










Similar content being viewed by others
Data availability
All data will be made available on request.
Code availability
All codes used will be made available on request.
References
Clarke S (2016) 3D printed surface applicators for high dose rate brachytherapy. MSc Thesis Dalhousie University
Harris BD, Nilsson S, Poole CM (2015) A feasibility study for using ABS plastic and a low-cost 3D printer for patient-specific brachytherapy mould design. Australassian Physical & Engineering Scinces in Medicine 38(3):399–412. https://doi.org/10.1007/s13246-015-0356-3
Zhao Y, Moran K, Yewondwossen M, Allan J, Clarke S, Rajaraman M, Wilke D, Joseph P, Robar JL (2017) Clinical applications of 3-dimensional printing in radiation therapy. Med Dosim 42(2):150–155. https://doi.org/10.1016/j.meddos.2017.03.001
Boman EL, Paterson DB, Pearson S, Naidoo N, Johnson C (2018) Dosimetric comparison of surface mould HDR brachytherapy with VMAT. Journal of Medical Radiation Sciences 65(4):311–318. https://doi.org/10.1002/jmrs.301
Allen Li X, Yu C, Holmes T (2000) A systematic evaluation of air cavity dose perturbation in megavoltage x-ray beams. Med Phys 27(5):1011–1017. https://doi.org/10.1118/1.598966
Sharma SC, Johnson MW (1993) Surface dose perturbation due to air gap between patient and bolus for electron beams. Med Phys 20(2):377–378. https://doi.org/10.1118/1.597079
Fowler TL, Buyyounouski MK, Jenkins CH, Fahimian BP (2016) Clinical implementation of 3D printing for brachytherapy: techniques and emerging applications. Brachytherapy. https://doi.org/10.1016/j.brachy.2016.04.297
Jones EL, Tonino Baldion A, Thomas C, Burrows T, Byrne N, Newton V, Aldridge S (2017) Introduction of novel 3D-printed superficial applicators for high-dose-rate skin brachytherapy. Brachytherapy 16(2):409–414. https://doi.org/10.1016/j.brachy.2016.11.003
Lecornu M, Silva M, Barraux V, Stefan D, Kao W, Thariat J, Loiseau C (2019) Digital applicator by 3D printing in contact brachytherapy. Cancer/Radiotherapie 23(4):328–333. https://doi.org/10.1016/j.canrad.2019.03.008
Ricotti R, Vavassori A, Bazani A, Ciardo D, Pansini F, Spoto R, Sammarco V, Cattani F, Baroni G, Orecchia R, Jereczek-Fossa BA (2016) 3D-printed applicators for high dose rate brachytherapy: Dosimetric assessment at different infill percentage. Physica Med 32(12):1698–1706. https://doi.org/10.1016/j.ejmp.2016.08.016
Schumacher M, Lasso A, Cumming I, Rankin A, Falkson CB, Schreiner LJ, Joshi C, Fichtinger G (2015) 3D-printed surface mould applicator for high-dose-rate brachytherapy. SPIE Medical Imaging 9415:91452E. https://doi.org/10.1117/12.2082543
Bassi S, Langan B, Malone C (2019) Dosimetry assessment of patient-specific 3D printable materials for HDR surface brachytherapy. Physica Med 67:166–175. https://doi.org/10.1016/j.ejmp.2019.10.035
Arenas M, Sabater S, Sintas A, Arguis M, Hernandez V, Arquez M, Lopez I, Rovirosa A, Puig D (2017) Individualized 3D scanning and printing for non-melanoma skin cancer brachytherapy: a financial study for its integration into clinical workflow. Journal of Contemporary Brachytherapy 9(3):270–276. https://doi.org/10.5114/jcb.2017.68134
Burleson S, Baker J, Hsia AT, Xu Z (2015) Use of 3D printers to create a patient-specific 3D bolus for external beam therapy. J Appl Clin Med Phys 16(3):166–178. https://doi.org/10.1120/jacmp.v16i3.5247
LeCompte MC, Chung SA, McKee MM, Marshall TG, Frizzell B, Parker M, Blackstock AW, Farris MK (2019) Simple and Rapid Creation of Customized 3-dimensional Printed Bolus Using iPhone X True Depth Camera. Pract Radiat Oncol 9(4):e417–e421. https://doi.org/10.1016/j.prro.2019.03.005
Su S, Moran K, Robar JL (2014) Design and production of 3D printed bolus for electron radiation therapy. J Appl Clin Med Phys 15(4):194–211. https://doi.org/10.1120/jacmp.v15i4.4831
Douglass MJJ, Caraça Santos AM (2019) Application of optical photogrammetry in radiation oncology: HDR surface mold brachytherapy. Brachytherapy. https://doi.org/10.1016/j.brachy.2019.05.006
Baltsavias EP (1999) A comparison between photogrammetry and laser scanning. ISPRS J Photogramm Remote Sens 54(2–3):83–94. https://doi.org/10.1016/S0924-2716(99)00014-3
Barry P, Coakley R (2013) Field accuracy test of RPAS photogrammetry. International Archives of the Photogrammetry, Remote Sensing and Spatial Information Sciences - ISPRS Archives 40:27–31
Falkingham PL (2012) Acquisition of high resolution three-dimensional models using free, open-source, photogrammetric software. Palaeontol Electron 15(1):1–15
Guarnieri A, Vettore A, El-Hakim S, Gonzo L (2004) Digital photogrammetry and laser scanning in cultural heritage survey. International Archives of the Photogrammetry, Remote Sensing and Spatial Information Sciences - ISPRS Archives 35:154–158
Kadobayashi R, Kochi N, Otani H, Furukawa R (2004) Comparison and evaluation of laser scanning and photogrammetry and their combined use for digital recording of cultural heritage. International Archives of the Photogrammetry, Remote Sensing and Spatial Information Sciences - ISPRS Archives 35:401–406
Morgan B, Ford ALJ, Smith MJ (2019) Standard methods for creating digital skeletal models using structure-from-motion photogrammetry. Am J Phys Anthropol 169(1):152–160. https://doi.org/10.1002/ajpa.23803
Peña-Villasenín S, Gil-Docampo M, Ortiz-Sanz J (2020) Desktop vs cloud computing software for 3D measurement of building façades: The monastery of San Martín Pinario Measurement. J Inter Meas Confederation. https://doi.org/10.1016/j.measurement.2019.106984
Porter ST, Roussel M, Soressi M (2017) A Simple Photogrammetry Rig for the Reliable Creation of 3D Artifact Models in the Field. Adv Archaeol Pract 4(1):71–86. https://doi.org/10.7183/2326-3768.4.1.71
Remondino F (2011) Heritage recording and 3D modeling with photogrammetry and 3D scanning. Remote Sen 3(6):1104–1138. https://doi.org/10.3390/rs3061104
Remondino F, Guarnieri A, Vettore A (2005) 3D modeling of close-range objects: Photogrammetry or laser scanning? Proc SPIE 5665:216–225. https://doi.org/10.1117/12.586294
Vacca G (2019) Overview of open source software for close range photogrammetry. International Archives of the Photogrammetry, Remote Sensing and Spatial Information Sciences - ISPRS Archives 42:239–245. https://doi.org/10.5194/isprs-archives-XLII-4-W14-239-2019
Vlachos M, Berger L, Mathelier R, Agrafiotis P, Skarlatos D (2019) Software comparison for underwater archaeological photogrammetric applications. Inter Archives Photogrammetry, Remote Sensing and Spatial Information Sciences - ISPRS Archives 42:1195–1201. https://doi.org/10.5194/isprs-archives-XLII-2-W15-1195-2019
Weinberg SM, Naidoo S, Govier DP, Martin RA, Kane AA, Marazita ML (2006) Anthropometric precision and accuracy of digital three-dimensional photogrammetry: Comparing the genex and 3dMD imaging systems with one another and with direct anthropometry. J Craniofacial Surg 17(3):477–483. https://doi.org/10.1097/00001665-200605000-00015
Westoby MJ, Brasington J, Glasser NF, Hambrey MJ, Reynolds JM (2012) “Structure-from-Motion” photogrammetry: A low-cost, effective tool for geoscience applications. Geomorphology 179:300–314. https://doi.org/10.1016/j.geomorph.2012.08.021
Wong JY, Oh AK, Ohta E, Hunt AT, Rogers GF, Mulliken JB, Deutsch CK (2008) Validity and reliability of craniofacial anthropometric measurement of 3D digital photogrammetric images. Cleft Palate Craniofac J 45(3):232–239. https://doi.org/10.1597/06-175
Liba N, Metsoja K, Järve I, Miljan J (2019) Making 3D models using close-range photogrammetry: comparison of cameras and software. Int Multidiscip Sci GeoConf SGEM 19:561–568. https://doi.org/10.5593/sgem2019/2.2/S10.069
Slaker BA, Mohamed KM (2017) A practical application of photogrammetry to performing rib characterization measurements in an underground coal mine using a DSLR camera. Int J Min Sci Technol 27(1):83–90. https://doi.org/10.1016/j.ijmst.2016.09.032
Zhongming A (2017) Accuracy Assessment of 3D Point Clouds Generated by Photogrammetry From Different Distances. MSc Thesis:Michigan Technological University
Jennings A, Black J (2012) Texture-based photogrammetry accuracy on curved surfaces. AIAA J 50(5):1060–1071. https://doi.org/10.2514/1.J050956
Blender Online Community (2020) Blender – a 3D modelling and rendering package. Blender Insititute, Amsterdam: Blender Foundation. https://www.blender.org/.
CloudCompare (2020) CloudCompare – 3D point cloud and mesh processing software. Open source project. http://cloudcompare.org/.
Besl PJ, McKay ND (1992) A method for registration of 3-D shapes. IEEE Trans Pattern Anal Mach Intell 14(2):239–256. https://doi.org/10.1109/34.121791
Wu J, Tillett R, McFarlane N, Ju X, Siebert JP, Schofield P (2004) Extracting the three-dimensional shape of live pigs using stereo photogrammetry. Comput Electron Agric 44(3):203–222. https://doi.org/10.1016/j.compag.2004.05.003
Bell T, Li B, Zhang S (2016) Structured Light Techniques and Applications. In: Wiley Encyclopedia of Electrical and Electronics Engineering. pp 1–24. doi:https://doi.org/https://doi.org/10.1002/047134608X.W8298
Zhang S (2013) Handbook of 3D machine vision: Optical metrology and imaging. CRC press
Acknowledgements
Corey Bridger acknowledges the support he has received for his research through the provision of an Australian Government Research Training Program Scholarship. The authors wish to acknowledge the Medical Physics Department at the Royal Adelaide Hospital for providing the anthropomorphic RANDO phantom and Laerdal Little Anne CPR training manikin used throughout this work.
Funding
Corey Bridger acknowledges the support he has received for his research through the provision of an Australian Government Research Training Program Scholarship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval
This study used anthropomorphic phantoms and no human participants. No ethics approval was required.
Informed Consent
This study used anthropomorphic phantoms and no human participants. No informed consent was required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Bridger, C.A., Douglass, M.J.J., Reich, P.D. et al. Evaluation of camera settings for photogrammetric reconstruction of humanoid phantoms for EBRT bolus and HDR surface brachytherapy applications. Phys Eng Sci Med 44, 457–471 (2021). https://doi.org/10.1007/s13246-021-00994-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13246-021-00994-4