Abstract
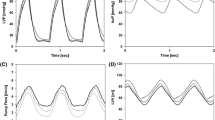
Continuous-flow ventricular assist devices (CF-VADs) defy normal physiologic principles associated with pulsatile flow. Despite being programmed at set speeds, pump flow can be modified by variations in the pressure differential across the pump, termed pressure sensitivity (PS). Currently, PS has been reported using steady-state closed-loop systems that are unable to provide physiologically-relevant assessment of PS or account for partially- or fully-unloaded ventricles. We report a unique model system to examine PS and its influence on efficiency of CF-VADs. A mock-circulation loop was designed that measures low and high extremes of pressure differential. Two axial-flow and two centrifugal-flow VADs were tested. Device output flow rate, preload, and afterload were measured and PS was calculated. Numerical models were implemented to simulate “fully-loaded,” “partially-unloaded,” and “fully-unloaded” cardiac cycles. Our open-loop model successfully generated pressure gradients that were lower than typical when using static, closed-loop systems. All devices exhibit highest PS during early diastole; however, average PS values of centrifugal-flow were 3× greater than axial-flow devices. The average maximum PS for the axial and centrifugal VADs under physiologic conditions was 0.08 and 0.42 L/min/mmHg, respectively. Compared to the axial-flow pumps, the two centrifugal-flow VADs in our study demonstrate increased PS at intermediate to low flow rates. Enhanced device PS allows for more effective self-regulation of device output, thus allowing a given VAD to better mimic the native heart under exercise conditions, and minimize undesirable effects, including ventricular suck-down or atrial collapse.







Similar content being viewed by others
References
Akers, A., M. Gassman, and R. Smith. Hydraulic Power Systems Analysis. Boca Raton: CRC Press, 2006.
Akimoto, T., K. Yamazaki, P. Litwak, et al. Rotary blood pump flow spontaneously increases during exercise under constant pump speed: results of a chronic study. Artif. Organs 23:797–801, 1999.
Akimoto, T., K. Yamazaki, P. Litwak, et al. Relationship of blood pressure and pump flow in an implantable centrifugal blood pump during hypertension. ASAIO J. 46:596–599, 2000.
Bearnson, G. B., G. B. Jacobs, J. Kirk, P. S. Khanwilkar, K. E. Nelson, and J. W. Long. HeartQuest VAD magnetically levitated centrifugal blood pump. Artif. Organs 30:339–346, 2006.
Farrar, D. J., K. Bourque, C. P. Dague, C. J. Cotter, and V. L. Poirier. Design features, developmental status and experimental results with the Heartmate III centrifugal LVAS with magnetically levitated rotor. ASAIO J. 53:310–315, 2007.
Frazier, O. H., H. A. Khalil, R. J. Benkowski, and W. E. Cohn. Optimization of axial-pump pressure sensitivity for a continuous-flow TAH. J. Heart Lung Transpl. 29:687–691, 2010.
Guyton, A. C., and J. E. Hall. Textbook of Medical Physiology (12th ed.). Philadelphia: Saunders, 2011.
Joyce, D. L., L. D. Joyce, and M. Loebe. Mechanical Circulatory Support: Principles and Applications. New York: McGraw-Hill, 2011.
Karassik, I. J., J. P. Messina, P. Cooper, et al. Pump Handbook, 2nd ed. New York: McGraw-Hill, 1986.
Khalil, H. A., W. E. Cohn, R. W. Metcalfe, and O. H. Frazier. Preload sensitivity of the Jarvik 2000 and HeartMate II LVADs. ASAIO J. 54:245–248, 2008.
Korakianitis, T., and Y. Shi. Numerical comparison of hemodynamics with atrium to aorta and ventricular apex to aorta VAD support. ASAIO J. 53:537–548, 2007.
Kormos, R. L., and L. W. Miller. Mechanical Circulatory Support: A Companion to Braunwald’s Heart Disease. Philadelphia: Elsevier, 2011.
Manning, F. S., and R. E. Thompson. Oilfield Processing of Petroleum: Crude Oil. Tulsa: PennWell, 1995.
Mizuno, T., R. D. Weisel, and R. K. Li. Reloading the heart: a new animal model of LVAD removal. J. Thorac. Cardovasc. Surg. 130:99–106, 2005.
Morley, D., K. Litwak, P. Spence, et al. Hemodynamic effects of partial ventricular support in chronic heart failure: results of simulation validated with in vivo data. J. Thorac. Cardiovasc. Surg. 133:21–28, 2007.
Morshuis, M., M. Schoenbrodt, C. Nojiri, et al. DuraHeart magnetically levitated centrifugal LVAS for advanced heart failure patients. Expert Rev. Med. Devices 7:173–183, 2010.
Nose, Y. Is a pulsatile cardiac prosthesis a dying dinosaur? Artif. Organs 16:233–234, 1992.
Potapov, E. V., A. Koster, M. Loebe, et al. The MicroMed DeBakey VAD—Part I: the pump and the blood flow. JECT 35:274–283, 2003.
Salamonsen, R. F., D. G. Mason, and P. J. Ayre. Response of rotary blood pumps to changes in preload and afterload at a fixed speed setting are unphysiological when compared with the natural heart. Artif. Organs 35:E47–E53, 2011.
Saxton, Jr, G. A., and C. B. Andrews. An ideal heart pump with hydrodynamic characteristics analogous to the mammalian heart. ASAIO Trans. 6:288–291, 1960.
Smith, W. A., P. Allaire, J. Antaki, et al. Collected nondimensional performance of rotary dynamic blood pumps. ASAIO J. 50:25–32, 2004.
Stepanoff, A. J. Centrifugal and Axial Flow Pumps, 2nd ed. New York: Wiley, 2011.
Tansley, G., S. Vidakovic, and J. Reizes. Fluid dynamic characteristics of the VentrAssist rotary blood pump. Artif. Organs 24:483–487, 2000.
Vollkron, M., P. Voitl, J. Ta, G. Wieselthaler, and H. Schima. Suction events during left ventricular support and ventricular arrhythmias. J. Heart Lung Transpl. 26:819–825, 2007.
Acknowledgment
This work was funded in part by the National Institute of Health R01HL089592 (CHS). Dr. Stanfield reports being a former employee of World Heart, Inc. No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Keefe B. Manning oversaw the review of this article.
Rights and permissions
About this article
Cite this article
Stanfield, J.R., Selzman, C.H. Pressure Sensitivity of Axial-Flow and Centrifugal-Flow Left Ventricular Assist Devices. Cardiovasc Eng Tech 3, 413–423 (2012). https://doi.org/10.1007/s13239-012-0110-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-012-0110-x