Abstract
Introduction
Sepsis is the dysregulated response of the body to the infection. Obstetric sepsis carries significantly greater morbidity and mortality as the condition is also augmented by the physiological adaptation of body during pregnancy. We conducted this study to determine the various epidemiological and clinical determinants of severity of sepsis which can help in prediction of survival in case of obstetric sepsis.
Materials and Methods
This retrospective study was conducted in a tertiary care center and all cases admitted with the diagnosis of obstetric sepsis as per the defined criteria between January 1, 2016 and December 31, 2020 were included in the study. Patients were evaluated for their clinical presentation, SOFA score, biochemical and microbiological parameters and the treatment given during their course of stay. Variables were compared among survivor and non-survivor group using appropriate statistical tests. Parameters which have significant association were further taken for binary logistic regression analysis.
Result
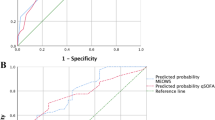
A total 46 patients of obstetric sepsis were admitted under defined criteria. Twelve out of 46 patients did not survive (26.09%). On statistical analysis, mean SOFA score (p = 0.005) as well as patients with SOFA score > 6 (p = 0.029), presence of multi organ failure (0.04) and septic shock (p = 0.012) were found to be significantly associated with mortality.
Conclusion
The study suggests that these determinants of survival should always be evaluated while catering to a patient of obstetric sepsis in order to guide the treatment, prognostication and improving outcome of the patients.



Similar content being viewed by others
References
van Dillen J, Zwart J, Schutte J, van Roosmalen J. Maternal sepsis: epidemiology, etiology and outcome. Curr Opin Infect Dis. 2010;23(3):249–54.
Shrestha GS, Kwizera A, Lundeg G, Baelani JI, Azevedo LCP, Pattnaik R, et al. International Surviving Sepsis Campaign guidelines 2016: the perspective from low-income and middle-income countries. Lancet Infect Dis. 2017;17(9):893–5.
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315(8):801–10.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
Acosta CD, Kurinczuk JJ, Lucas DN, Tuffnell DJ, Sellers S, Knight M. Severe maternal sepsis in the UK, 2011–2012: a national case-control study. PLoS Med. 2014;11(7):e1001672.
Acosta CD, Harrison DA, Rowan K, Lucas DN, Kurinczuk JJ, Knight M. Maternal morbidity and mortality from severe sepsis: a national cohort study. BMJ Open. 2016;6(8):e012323.
Knowles SJ, Osullivan NP, Meenan AM, Hanniffy R, Robson M. Maternal sepsis incidence, aetiology and outcome for mother and fetus: a prospective study. BJOG Int J Obstet Gynaecol. 2015;122(5):663–71.
Surgers L, Bleibtreu A, Burdet C, Clermont O, Laouénan C, Lefort A, et al. Escherichia coli bacteraemia in pregnant women is life-threatening for foetuses. Clin Microbiol Infect. 2014;20(12):O1035–41.
Jones AE, Trzeciak S, Kline JA. The Sequential Organ Failure Assessment score for predicting outcome in patients with severe sepsis and evidence of hypoperfusion at the time of emergency department presentation. Crit Care Med. 2009;37(5):1649–54.
Al-Ostad G, Kezouh A, Spence AR, Abenhaim HA. Incidence and risk factors of sepsis mortality in labor, delivery and after birth: population-based study in the USA. J Obstet Gynaecol Res. 2015;41(8):1201–6.
Vaught AJ. Maternal sepsis. Semin Perinatol. 2018;42(1):9–12.
Oud L, Watkins P. Evolving trends in the epidemiology, resource utilization, and outcomes of pregnancy-associated severe sepsis: a population-based cohort study. J Clin Med Res. 2015;7(6):400–16.
Song JE, Kim MH, Jeong WY, Jung IY, Oh DH, Kim YC, et al. Mortality risk factors for patients with septic shock after implementation of the surviving sepsis campaign bundles. Infect Chemother. 2016;48(3):199–208.
Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(9):840–51.
Holanda AMC, de Amorim MMR, Bezerra SMB, Aschoff LMS, Katz L. Risk factors for death in patients with sepsis admitted to an obstetric intensive care unit. Medicine (Baltimore). 2020;99(50):e23566.
Arnold RC, Sherwin R, Shapiro NI, O’Connor JL, Glaspey L, Singh S, et al. Multicenter observational study of the development of progressive organ dysfunction and therapeutic interventions in normotensive` sepsis patients in the emergency department. Acad Emerg Med. 2013;20(5):433–40.
Javed A, Guirgis FW, Sterling SA, Puskarich MA, Bowman J, Robinson T, et al. Clinical predictors of early death from sepsis. J Crit Care. 2017;42:30–4.
Levy MM, Evans LE, Rhodes A. The surviving sepsis campaign bundle: 2018 update. Intensive Care Med. 2018;44(6):925–8.
Ling RR, Ramanathan K, Poon WH, et al. Venoarterial extracorporeal membrane oxygenation as mechanical circulatory support in adult septic shock: a systematic review and meta-analysis with individual participant data meta-regression analysis. Crit Care. 2021;25:246. https://doi.org/10.1186/s13054-021-03668-5.
Ko RE, Chung CR, Yang JH, et al. Use of extracorporeal membrane oxygenation in postpartum patients with refractory shock or respiratory failure. Sci Rep. 2021;11:887. https://doi.org/10.1038/s41598-020-80423-w.
Weill D, Benden C, Corris PA, Dark JH, Davis RD, Keshavjee S, Lederer DJ, Mulligan MJ, Patterson GA, Singer LG, Snell GI, Verleden GM, Zamora MR, Glanville AR. A consensus document for the selection of lung transplant candidates: 2014—an update from the Pulmonary Transplantation Council of the International Society for Heart and Lung Transplantation. J Heart Lung Transplant. 2015;34(1):1.
Funding
No funding is received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors have no conflict of interest.
Ethical approval
The study was approved by Institute’s Ethics Committee via letter no. AIIMS/ Pat/IEC/2020/725 and individual patient’s consent was waived off as the study involves only secondary data analysis and there was no risk involved for the participants, and identity of the participants was not revealed at any point of time.
Human and animal rights
No patient is harmed in conducting this research and all rights of human participants keep protected, while conducting this research.
Informed consent
As this is a retrospective study involving secondary data analysis of available data of already treated patients, individual patient’s consent is waived off by the Institute’s Ethics Committee, and identity of any patient was not revealed at any point of time.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Agarwal, M., Bhushan, D., Singh, S. et al. Determinants of Survival in obstetric Sepsis: Retrospective Observational Study. J Obstet Gynecol India 72 (Suppl 1), 159–165 (2022). https://doi.org/10.1007/s13224-021-01611-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-021-01611-w