Abstract
Background
Miscarriage is defined as an adverse and unexpected termination of pregnancy; it is the most frequent pregnancy complication. Here, we aimed to identify the factors predisposing to miscarriage in pregnant women in Eastern Algeria and the effect of the combination of several factors, including maternal Body Mass Index (BMI), maternal age, concomitant pathologies, and nutrients, and to predict the occurrence of miscarriage.
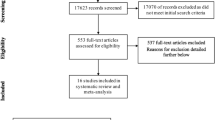
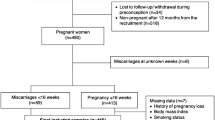
Methods
A total of 786 pregnant women from Eastern Algeria were interviewed between 2011 and 2015. Association between miscarriage exposure and identified risk factors was assessed using a Generalized Linear Model (GLM), ANOVA test, Multiple Correspondence Analysis (MCA), and Hierarchical Clustering Analysis (HCA). Throughout this study, we sought to find answers, discuss this association, and predict the occurrence of miscarriage.
Results
We developed a predictive model for miscarriage, and we found that miscarriage was significantly higher for pregnant women aged over 35 years (1.75; 95% CI: 0.75–4.37; p = 0.208), with a high BMI (> 25 kg/m2), (1.88; 95% CI:1.28–2.78; p = 0.001). We have highlighted that miscarriage is strongly associated with hypertension (1.67; 95% CI: 1.16–2.39; p = 0.006), diet rich in meat (0.60; 95% CI: 0.33–1.04; p = 0.075), and moderate in fish (2.32; 95% CI: 1.18–4.58; p = 0.015).
Conclusion
Our study proved that knowing these risk factors helps to establish predictive models and strategies to prevent tragic pregnancy outcomes and highlights the link between miscarriage and several risk factors; and thus, will allow protecting mother and fetus health.






Similar content being viewed by others
References
Martin CE, Scialli A, Terplan M. Addiction and depression: unmet treatment needs among reproductive age women. Matern Child Health J [Internet]. 2020;24:660–7. https://doi.org/10.1007/s10995-020-02904-8.
Delabaere A, Huchon C, Deffieux X, et al. Épidémiologie Des Pertes De Grossesse. J Gynecol Obstet Biol la Reprod. 2014;43:764–75.
McClure JH, Cooper GM, Clutton-Brock TH. Saving mothers’ lives: reviewing maternal deaths to make motherhood safer: 20068: a review. Br J Anaesth. 2011;107:127–32.
Banno C, Sugiura-Ogasawara M, Ebara T, et al. Attitude and perceptions toward miscarriage: a survey of a general population in Japan. J Hum Genet [Internet]. 2020;65:155–64. https://doi.org/10.1038/s10038-019-0694-1.
Qu F, Wu Y, Zhu YH, et al. The association between psychological stress and miscarriage: a systematic review and meta-analysis. Sci Rep [Internet]. 2017;7:1–8. https://doi.org/10.1038/s41598-017-01792-3.
Kicia M, Skurzak A, Wiktor K, et al. Anxiety and stress in miscarriage. Polish J Public Heal. 2018;125:162–5.
Brezina PR. Genetic screening and early recurrent pregnancy loss. Curr Obstet Gynecol Rep. 2017;6:163–8.
Addati L, Cassirer N, Gilchrist K. Maternity and paternity at work : law and practice across the world [Internet]. ILO. International Labour Office, editor. Geneva; 2014. Available from: www.ilo.org/publns.
Maconochie N, Doyle P, Prior S, et al. Risk factors for first-trimester miscarriage - results from a UK-population-based case-control study. BJOG An Int J Obstet Gynaecol. 2007;114:170–86.
El Sanharawi M, Naudet F. Comprendre la régression logistique. J Fr Ophtalmol [Internet]. 2013;36:710–5. https://doi.org/10.1016/j.jfo.2013.05.008.
Haoud K, Mellali S, Gouas L, et al. Prevalence of aneuploidies in products of spontaneous abortion: interest of FISH and MLPA. Morphologie [Internet]. 2014;98:40–6. https://doi.org/10.1016/j.morpho.2014.02.001.
Mellali S, Haoud K, Gouas L, et al. Prenatal BoBsTM in the cytogenetic analysis of products of spontaneous miscarriage. South African Med J. 2015;105:870–3.
Fuchs F, Monet B, Ducruet T, et al. Effect of maternal age on the risk of preterm birth: a large cohort study. Obstet Gynecol Surv. 2018;73:340–2.
Ben-David A, Glasser S, Schiff E, et al. Pregnancy and birth outcomes among primiparae at very advanced maternal age: at what price? Matern Child Health J. 2016;20:833–42.
Tabrizi JS, Asghari A, Pourali F, et al. Effects of food supplementation during pregnancy on maternal weight gain, hemoglobin levels and pregnancy outcomes in Iran. Matern Child Health J [Internet]. 2019;23:258–64. https://doi.org/10.1007/s10995-018-2648-1.
Johansson S, Villamor E, Altman M, et al. Maternal overweight and obesity in early pregnancy and risk of infant mortality: a Population based cohort study in Sweden. BMJ [Internet]. 2014;349:1–12. https://doi.org/10.1136/bmj.g6572.
Reynolds RM, Allan KM, Raja EA, et al. Maternal obesity during pregnancy and premature mortality from cardiovascular event in adult offspring: follow-up of 1 323 275 person years. BMJ [Internet]. 2013;347:1–10. https://doi.org/10.1136/bmj.f4539.
Ju AC, Heyman MB, Garber AK, et al. Maternal obesity and risk of preterm birth and low birthweight in Hawaii PRAMS, 2000–2011. Matern Child Health J [Internet]. 2018;22:893–902. https://doi.org/10.1007/s10995-018-2464-7.
Turner MJ, Fattah C, O’Connor N, et al. Body mass index and spontaneous miscarriage. Eur J Obstet Gynecol Reprod Biol [Internet]. 2010;151:168–70. https://doi.org/10.1016/j.ejogrb.2010.04.021.
Heude B, Thiébaugeorges O, Goua V, et al. Pre-pregnancy body mass index and weight gain during pregnancy: relations with gestational diabetes and hypertension, and birth outcomes. Matern Child Health J. 2012;16:355–63.
Pan ML, Chen LR, Tsao HM, et al. Prepregnancy endocrine, autoimmune disorders and the risks of gestational hypertension-preeclampsia in primiparas: A nationwide population-based study in Taiwan. Int J Environ Res Public Health. 2020;17.
Behrens I, Basit S, Lykke JA, et al. Association between hypertensive disorders of pregnancy and later risk of cardiomyopathy. JAMA - J Am Med Assoc. 2016;315:1026–33.
Kharazmi E, Fallah M, Luoto R. Miscarriage and risk of cardiovascular disease. Acta Obstet Gynecol Scand. 2010;89:284–8.
Razak A, Florendo-Chin A, Banfield L, et al. Pregnancy-induced hypertension and neonatal outcomes: a systematic review and meta-analysis. J Perinatol. 2018;38:46–53.
Nelson DB, Grisso JA, Joffe MM, et al. Does stress influence early pregnancy loss? Ann Epidemiol. 2003;13:223–9.
Golbasi Z, Kelleci M, Kisacik G, et al. Prevalence and correlates of depression in pregnancy among Turkish women. Matern Child Health J. 2010;14:485–91.
Lynch CD, Sundaram R, Buck Louis GM. Biomarkers of preconception stress and the incidence of pregnancy loss. Hum Reprod. 2018;33:728–35.
Lee A, Belski R, Radcliffe J, et al. What do pregnant women know about the healthy eating guidelines for pregnancy? A web-based questionnaire. Matern Child Health J. 2016;20:2179–88.
Duke CH, Williamson JA, Snook KR, et al. Association between fruit and vegetable consumption and sleep quantity in pregnant women. Matern Child Health J. 2017;21:966–73.
Laurenzi C, Field S, Honikman S. Food insecurity, maternal mental health, and domestic violence: a call for a syndemic approach to research and interventions. Matern Child Health J [Internet]. 2020;24:401–4. https://doi.org/10.1007/s10995-019-02872-8.
WHO. Enquête nationale sur la mesure du poids des facteurs de risque des Maladies Non Transmissibles selon l’approche STEPwise de l’OMS Principaux résultats [Internet]. Algérie; 2017. Available from: https://www.afro.who.
Cheurfa T, Kaïd Tlilane N. L’insuffisance renale chronique terminale en Algerie: Aspects epidemiologiques et économiques. Les Cah. Du Cread. 2015.
Jitraknatee J, Ruengorn C, Nochaiwong S. Prevalence and risk factors of chronic kidney disease among type 2 diabetes patients: a cross-sectional study in primary care practice. Sci Rep. 2020;10:1–10.
Nelson DB, Hanlon AL, Wu G, et al. First trimester levels of BV-associated bacteria and risk of miscarriage among women early in pregnancy. Matern Child Health J. 2015;19:2682–7.
Acknowledgments
This paper and the research behind it would not have been possible without the exceptional support of my supervisor Pr. Mouloud Yahia (RIP). I would like to express my sincere appreciation to my colleagues at Batna University for their technical assistance, provided insight and expertise that greatly assisted the research. I wish to extend my special thanks and greet everyone who has supported the creation of this work. Great thanks to The DGRSDT (General Directorate of Scientific Research and Technological Development in Algeria), Departments of Health in hospitals of Mother and Child, especially The Head of the Department of Health in Batna, and Dr. Benakcha.
Funding
No funds, grants, or other support were received.
Author information
Authors and Affiliations
Contributions
Adel Kalla led the study by being involved in data collection, performing the statistical analysis, interpreting the results, conceiving, and designing this article, and providing intellectual content revisions and suggestions for clarity and precision on the subject matter. Mouloud Yahia has initiated the study as a physio-pathologist and the head of the laboratory. Lotfi Loucif has been part of the study as the new head of the laboratory. All authors read and approved the final review manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Ethical Approval
Anonymous data are obtained from the Department of Health of Batna, who determined that Ethics approval is complying with the specific requirements of Algeria Law. The approval of a research ethics committee is not necessary in Algeria for an observational study since no intervention on patients took place in this study. Nonetheless, the study received clearance from the Internal Review Board of the University of Batna 2, Batna, Algeria.
Consent to Participate
Patients were not involved in the design, or conduct, or reporting, or dissemination plans of our research. However, informed written consent was obtained from all individual participants included in the study before conducting the interviews.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Adel KALLA is an assistant professor at the Faculty of Natural and Life Sciences at the University of Batna 2, Algeria.
Rights and permissions
About this article
Cite this article
Kalla, A., Loucif, L. & Yahia, M. Miscarriage Risk Factors for Pregnant Women: A Cohort Study in Eastern Algeria’s Population. J Obstet Gynecol India 72 (Suppl 1), 109–120 (2022). https://doi.org/10.1007/s13224-021-01564-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-021-01564-0