Abstract
Background
Pelvic organ prolapse (pop) is a chronic disorder, often asymptomatic. There are several factors involved in the aetio-pathogenesis of POP. Perimenopausal women bear most of the burden of pop. Vaginal delivery is an established risk factor and clinical presentation may take years when women are symptomatic in menopausal age.
Method
A cross-sectional study was done for one year in a rural teaching hospital, where 150 pop women were included. Variables associated with both asymptomatic & symptomatic pop were analyzed. The mean, proportion, & simple logistic regression were used to analyze the data and p value < 0.05 was considered significant.
Results
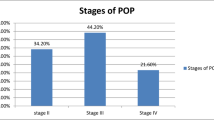
The prevalence of pop was 4.8%. Associated socio-economic & obstetrical variables were age group of 41–50 years (82.7%), housewives (84%), multiparty (93.33%), lower economic conditions (86.7%), home deliveries (74.71%), and early resumption of work after delivery (61.3%). Bulging in the vagina (p < 0.001), & difficulties in micturition (p = 0.001) were significant symptoms. Among asymptomatic & symptomatic pop, difference in BMI (p = 0.042), education level (p = 0.001), menstrual history (p = 0.001) & place of delivery (p = 0.037) were significant. Different stages of pop were significantly associated with differences in age groups (p < 0.001), menstrual history (p < 0.001) & place of delivery (p = 0.039). Differences in the proportion of constipation were significant with anterior compartment defects (p < 0.001), whereas the association of chronic lung diseases was found significant (p = 0.028) in the case of apical compartment prolapse. Simple logistic regression of co-variants shows age can predict the severity of pop stages (OR 7.25; 95% CI 1.95–26.99).
Conclusion
All stages of pop were present mostly in the age group of 41–50 years rather than in the over 50 years age group. Menopause is associated with the severity of prolapse and is mostly symptomatic. Age can predict the severity of pop.
Similar content being viewed by others
References
Sumathi N, Nandhini CC. Uterovaginal prolapse-a study in South Indian Women. Sch J Appl Med Sci. 2017;5(4F):1698–704.
Miedel A, Tegerstedt G, Maehle-Schmidt M, et al. Non obstetric risk factors for symptomatic pelvic organ prolapse. Obstet Gynecol. 2009;113(5):1089–97.
Quiroz LH, Munoz A, Shippey SH, et al. Vaginal parity and pelvic organ prolapse. J Reprod Med. 2010;55(3–4):93–8.
Shaikh Z, Pathak R. Revised Kuppuswamy and B. G. Prasad socio-economic scales for 2016. Int J Community Med Public Health. 2017;4:997–9.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet. 2004;363(9403):157–63.
Raiser J, Kumari S, Walia I, et al. Self-reported uterine prolapse in a resettlement colony of north India. J Midwifery Women’s Health. 2011;45(4):343–50.
Wu JM, Vaughan CP, Goode PS, et al. Prevalence and trends of symptomatic pelvic floor disorders in U.S. women. Obstet Gynecol. 2014;123(1):141–8.
Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24:1783–90.
Gumanga SK, Munkaila A, Malechi H. Social demographic characteristics of women with pelvic organ prolapse at the Tamale Teaching Hospital. Ghana Ghana Med J. 2014;48(4):208–13.
Dhama V, Chaudhary R, Singh S, et al. Evaluation of pelvic organ prolapse by standardized pop q system for vaginal hysterectomy. Int J Reprod Contracept Obstet Gynecol. 2017;6:2584–8.
Asresie A, Adamassu E, Setegn T. Determinants of pelvic organ prolapse among gynecologic patients in Bahir Dar, North West Ethiopia: a case-control study. Int J Womens Health. 2016;8:713–9.
Mesenga GG, Shayo BC, Rasch V. Prevalence and risk factors for pelvic organ prolapse in Kilimanjaro, Tanzania: a population based study in Tanzanian rural community. PLoS ONE. 2018;13(4):1–13.
Giri A, Hartmann KE, Hellwege JN, et al. Obesity and pelvic organ prolapse: a systematic review and meta-analysis of observational studies. Am J Obstet Gynecol. 2017;217(1):11–26.
Patil P, Patil A. Evaluation of Pelvic Organ Prolapse in Indian Females. J Evol Med Dent Sci. 2013;2(40):7612–20.
Urbankova I, Grohregin K, Hanacek J, et al. The effect of the first vaginal birth on pelvic floor anatomy and dysfunction. Int Urogynecol J. 2019;30(10):1689–96.
Peker N, Erdem B, Kaban A. Does home birth reduce the risk of pelvic organ prolapse? Ginekol Pol. 2018;89(8):432–6.
Miedel A, Tegerstedt G, Maehle-Schmidt M, et al. Symptoms and pelvic support defects in specific compartments. Obstet Gynecol. 2008;112(4):851–8.
Myers DL, Sung VW, Richter HE, et al. Prolapse symptoms in overweight and obese women before and after weight loss. Female Pelvic Med Reconstr Surg. 2012;18(1):55–9.
Glazener C, Elders A, Macarthur C, et al. Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG. 2013;120(2):161–8.
Burrows LJ, Meyn LA, Walters MD, et al. Pelvic symptoms in women with pelvic organ prolapse. Obstet Gynecol. 2004;104(5):982–8.
Gyhagen M, Bullarbo M, Nielsen TF, et al. Prevalence and risk factors for pelvic organ prolapse 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG. 2013;120(2):152–60.
Hoffman BL, Schorge JO, Schaffer JI, et al. Williams Gynecology. New York: McGraw-Hill; 2012. p. 633–58.
Swift S, Woodman P, O’Boyle A, et al. Pelvic Organ Support Study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192(3):795–806.
Akter F, Gartoulla P, Oldroyd J, et al. Prevalence of, and risk factors for, symptomatic pelvic organ prolapse in Rural Bangladesh: a cross-sectional survey study. Int Urogynecol J. 2016;27(11):1753–9.
Ellerkmann RM, Cundiff GW, Melick CF, et al. Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. 2001;185(6):1332–7 (discussion 1337–8).
Weintraub AY, Glinter H, Marcus-Braun N. Narrative review of the epidemiology, diagnosis and pathophysiology of pelvic organ prolapse. Int Braz J Urol. 2020;46(1):5–14.
Funding
No funding source.
Author information
Authors and Affiliations
Contributions
MD KA &SK-design, data collection, analysis, interpretation of data and drafting of the article. PPS: conception, design, acquisition of data, analysis and revise critically for intellectual content of the article and final approval of the version.
Corresponding author
Ethics declarations
Conflict of interest
None declared regarding financial, personal, political, intellectual, or religious interests.
Ethical Approval
This study on human participants was approved by the institutional ethics committee and has been performed in accordance with the ethical standard as laid down in the Helsinki Declaration. This article does not contain any studies with animals performed by any of the authors.
Informed Consent
Patients written, informed consent for the study was taken before enrollment.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Md. Kamaluddin Ansari, M.B.B.S, M.S, RMO is an Department of Obstetrics and Gynecology, North Bengal Medical College and Hospital, Sushrutanagar, Darjeeling, West Bengal, India; Partha Pratim Sharma, M.B.B.S, M.D, Associate Professor is an Department of Obstetrics and Gynecology, Midnapore Medical College and Hospital, Paschim Midnapore, West Bengal, 721101, India; Sharmin Khan, M.B.B.S, M.D, Senior Resident, Department of Pharmacology, MidnaporeMedical College and Hospital, Paschim Midnapore, West Bengal, India.
Rights and permissions
About this article
Cite this article
Ansari, M.K., Sharma, P.P. & Khan, S. Pelvic Organ Prolapse in Perimenopausal and Menopausal Women. J Obstet Gynecol India 72, 250–257 (2022). https://doi.org/10.1007/s13224-021-01524-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13224-021-01524-8