Abstract
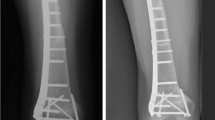
The purpose of this study was to discuss the epiphysis salvage reconstruction procedure outcomes and complications in skeletally immature patients. The study included 12 patients with pediatric malignant tumors (osteosarcoma, Ewing’s sarcoma) located close to the epiphysis, who underwent epiphyseal-preservation surgery with vascularized fibula in the plastic surgery and orthopedics and traumatology clinic between January 2008 and November 2018. The study was designed retrospectively. Neoadjuvant and adjuvant chemotherapy was administered to all patients. None of the patients received radiotherapy. Functional evaluation was assessed using the Musculoskeletal Tumor Society (MSTS) scoring system. The patients were followed up for a mean period of 51 (21‑115) months. The mean age of patients was 10.4 (range, 5 to 15) years. Union times in the target region (epiphyseal region) and diaphyseal region were reported separately. Accordingly, the mean total union time in the target region of all patients was 7.9 months (5‑11), and the mean total union time in the diaphyseal region was 6.5 months (5‑9). According to the MSTS grading system, the mean score of the patients was 27.50 (range, 21‑30). The mean operative time was 480 (390‑540) min, the mean intraoperative blood loss was 790 (580‑1100) cc, and the mean length of hospital stay was 6 (4‑17) days. Six patients had shortness, 5 patients had delayed union, 3 patients had angular deformity, and 2 patients had infection. Epiphyseal-preservation surgery may be an alternative to other techniques used for malignant tumors located close to the growth line in skeletally immature patients. Despite the fact that this technique has plenty of complications, many of them can be successfully treated with secondary operations without leaving sequelae.



Similar content being viewed by others
Data Availability
Not applicable.
References
Kim S-Y, Kim Y-G, Hwang J-K (2005) Cementless calcar-replacement hemiarthroplasty compared with intramedullary fixation of unstable intertrochanteric fractures: a prospective, randomized study. JBJS. 87(10):2186–2192
Racano A, Pazionis T, Farrokhyar F, Deheshi B, Ghert M (2013) High infection rate outcomes in long-bone tumor surgery with endoprosthetic reconstruction in adults: a systematic review. Clin Orthop Relat Res 471(6):2017–2027
Shehadeh A, Noveau J, Malawer M, Henshaw R (2010) Late complications and survival of endoprosthetic reconstruction after resection of bone tumors. Clin Orthop Relat Res 468(11):2885–2895
Kawai A, Lin PP, Boland PJ, Athanasian EA, Healey JH (1999) Relationship between magnitude of resection, complication, and prosthetic survival after prosthetic knee reconstructions for distal femoral tumors. J Surg Oncol 70(2):109–115
Gupta A, Meswania J, Pollock R et al (2006) Non-invasive distal femoral expandable endoprosthesis for limb-salvage surgery in paediatric tumours. J Bone Joint Surg Brit Vol 88(5):649–654
Ruggieri P, Mavrogenis AF, Pala E, Romantini M, Manfrini M, Mercuri M (2013) Outcome of expandable prostheses in children. J Pediatr Orthop 33(3):244–253
Saghieh S, Abboud MR, Muwakkit SA, Saab R, Rao B, Haidar R (2010) Seven-year experience of using Repiphysis® expandable prosthesis in children with bone tumors. Pediatr Blood Cancer 55(3):457–463
Staals EL, Colangeli M, Ali N, Casanova JM, Donati DM, Manfrini M (2015) Are complications associated with the Repiphysis® expandable distal femoral prosthesis acceptable for its continued use? Clin Orthop Relat Res 473(9):3003–3013
Picardo N, Blunn G, Shekkeris A et al (2012) The medium-term results of the Stanmore non-invasive extendible endoprosthesis in the treatment of paediatric bone tumours. J Bone Joint Surg Brit Vol 94(3):425–430
Khattak MJ, Umer M, Umar M (2006) Autoclaved tumor bone for reconstruction: an alternative in developing countries. Clin Orthop Relat Res 447:138–144
Pollock R, Stalley P, Lee K, Pennington D (2005) Free vascularized fibula grafts in limb-salvage surgery. J Reconstr Microsurg 21(02):79–84
Muscolo DL, Ayerza MA, Aponte-Tinao L, Ranalletta M, Abalo E (2004) Intercalary femur and tibia segmental allografts provide an acceptable alternative in reconstructing tumor resections. Clin Orthop Relat Res 426:97–102
Chang DW, Weber KL (2005) Use of a vascularized fibula bone flap and intercalary allograft for diaphyseal reconstruction after resection of primary extremity bone sarcomas. Plast Reconstr Surg 116(7):1918–1925
Berrey BH Jr, Lord CF, Gebhardt M, Mankin HJ (1990) Fractures of allografts. Frequency, treatment, and end-results. JBJS. 72(6):825–833
Cara JA, Lacleriga A, Cañadell J (1994) Intercalary bone allografts: 23 tumor cases followed for 3 years. Acta Orthop Scand 65(1):42–46
Muscolo DL, Ayerza MA, Aponte-Tinao LA, Ranalletta M (2004) Partial epiphyseal preservation and intercalary allograft reconstruction in high-grade metaphyseal osteosarcoma of the knee. JBJS. 86(12):2686–2693
Aponte-Tinao L, Ayerza MA, Muscolo DL, Farfalli GL (2015) Survival, recurrence, and function after epiphyseal preservation and allograft reconstruction in osteosarcoma of the knee. Clin Orthop Relat Res 473(5):1789–1796
Li J, Wang Z, Ji C, Chen G, Liu D, Zhu H (2017) What are the oncologic and functional outcomes after joint salvage resections for juxtaarticular osteosarcoma about the knee? Clin Orthop Relat Res 475(8):2095–2104
Enneking W, Dunham W, Gebhardt M, Malawar M, Pritchard D A system for the functional evaluation of reconstructive procedures after surgical treatment of tumors of the musculoskeletal system. Clin Orthop Relat Res 1993(286):241
Kapukaya A, Suba M, Kandiya E, Özate M, Yilmaz F (2000) Limb reconstruction with the callus distraction method after bone tumor resection. Arch Orthop Trauma Surg 120(3-4):215–218
Kapukaya A, Subasi M, Arslan H, Tuzuner T, Selek S (2006) Technique and complications of callus distraction in the treatment of bone tumors. Arch Orthop Trauma Surg 126(3):157–163
Hsu R-W, Wood MB, Sim FH, Chao EY (1997) Free vascularised fibular grafting for reconstruction after tumour resection. J Bone Joint Surg Brit Vol 79(1):36–42
Moran SL, Shin AY, Bishop AT (2006) The use of massive bone allograft with intramedullary free fibular flap for limb salvage in a pediatric and adolescent population. Plast Reconstr Surg 118(2):413–419
Weitao Y, Qiqing C, Songtao G, Jiaqiang W (2012) Epiphysis preserving operations for the treatment of lower limb malignant bone tumors. Eur J Surg Oncol (EJSO) 38(12):1165–1170
Kiss S, Terebessy T, Szöke G, Kiss J, Antal I, Szendröi M (2013) Epiphysis preserving resection of malignant proximal tibial tumours. Int Orthop 37(1):99–104
Takeuchi A, Yamamoto N, Hayashi K et al (2018) Growth of epiphysis after epiphyseal-preservation surgery for childhood osteosarcoma around the knee joint. BMC Musculoskelet Disord 19
Li J, Shi L, Chen G-j (2014) Image navigation assisted joint-saving surgery for treatment of bone sarcoma around knee in skeletally immature patients. Surg Oncol 23(3):132–139
Author information
Authors and Affiliations
Contributions
Study concepts: Rana Kapukaya, Evren Karaali, Osman Çiloğlu
Study design: Rana Kapukaya, Evren Karaali, Hasan Ulaş Oğur
Data acquisition: Rana Kapukaya, Mehmet Baydar, Hasan Ulaş Oğur
Quality control of data and algorithms: Rana Kapukaya, Hasan Ulaş Oğur, Mehmet Baydar
Data analysis and interpretation: Rana Kapukaya, Evren Karaali, Mehmet Baydar
Statistical analysis: Rana Kapukaya, Osman Çiloğlu, Hasan Ulaş Oğur
Manuscript preparation: Rana Kapukaya, Evren Karaali, Osman Çiloğlu
Manuscript editing: Rana Kapukaya, Evren Karaali, Mehmet Baydar
Manuscript review: Rana Kapukaya, Evren Karaali, Kahraman Öztürk
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Code Availability
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kapukaya, R., Karaali, E., Çiloğlu, O. et al. Epiphysis Salvage Reconstruction and Associated Complications Following Tumor Resections in Skeletally Immature Patients. Indian J Surg Oncol 12, 164–171 (2021). https://doi.org/10.1007/s13193-020-01275-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13193-020-01275-4