Abstract
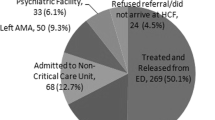
Many poisoned patients may only require a period of observation after their exposure. There are limited data describing the use of observation units for managing poisoned adult and pediatric patients. We performed a retrospective review of all patients reported to the ToxIC Case Registry between January 1, 2012 and December 31, 2013. Eligible patients included those who received a bedside consultation by a medical toxicologist and whose care was provided in an observation unit, or those who were admitted under the care of a medical toxicologist in an observation unit. A total of 15,562 poisonings were reported to the registry during the study period, of which 340 (2.2 %) involved patients who were cared for in an observation unit. Of these patients, 22.1 % were 18 years of age or younger, and the remaining 77.9 % were greater than 18 years of age. The most common reason for exposure was the intentional ingestion of a pharmaceutical agent in both adult (30.2 %) and pediatric patients (36.0 %). Alcohols (ethanol) (24.9 %), opioids (20.0 %), and sedative-hypnotics (17.7 %) were the most common agent classes involved in adult patient exposures. The most common agent classes involved in pediatric exposures were antidepressants (12.0 %), anticonvulsants (10.7 %), and envenomations (10.7 %). In adult patients, the most common signs and symptoms involved the nervous system (52.0 %), a toxidrome (17.0 %), or a major vital sign abnormality (14.7 %). In pediatric patients, the most common signs and symptoms involved the nervous system (53.3 %), a toxidrome (21.3 %), or a major vital sign abnormality (17.3 %). The results of this study demonstrate that a wide variety of poisoned patients have been cared for in an observation unit in consultation with a board-certified medical toxicologist. Patterns for the reasons for exposure, agents responsible for the exposure, and toxicological treatments will continue to evolve. Further study is needed to identify better those poisoned patients who can be appropriately managed in an observation unit.
Similar content being viewed by others
References
Mowry JB, Spyker DA, Cantilena LR, Bailey JE, Ford M. 2012 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 30th Annual Report. Clin Toxicol. 2013;51:949–1229.
Komindr A, Baugh CW, Grossman SA, Bohan SJ. Key operational characteristics in emergency department observation units: a comparative study between sites in the United States and Asia. Int J Emerg Med. 2014;7:6.
Yealy DM, De Hart DA, Ellis G, Wolfson AB. A survey of observation units in the United States. Am J Emerg Med. 1989;7(6):576–80.
Brillman J, Mathers-Dunbar L, Graff L, Joseph T, Leikin JB, Schultz C, et al. Management of observation units. Ann Emerg Med. 1995;25(6):823–30.
Ross MA, Graff 4th LG. Principles of observation medicine. Emerg Med Clin North Am. 2001;19(1):1–17.
Leikin JB. The uprooting of observational units from emergency departments: opportunity lost for emergency medicine? Am J Emerg Med. 1988;6(1):49–51.
Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 emergency department summary. Natl Health Stat Rep. 2010. Aug 6: 26; 1–31.
Ross MA, Compton S, Medado P, Fitzgerald M, Kilanowski P, O’Neil BJ. An emergency department diagnostic protocol for patients with transient ischemic attack: a randomized controlled trial. Ann Emerg Med. 2007;50(2):109–19.
Jagminas L, Partridge R. A comparison of emergency department versus inhospital chest pain observation units. Am J Emerg Med. 2005;23(2):111–3.
McDermott MF, Murphy DG, Zalenski RJ, Rydman RJ, McCarren M, Marder D, et al. A comparison between emergency diagnostic and treatment unit and inpatient care in the management of acute asthma. Arch Intern Med. 1997;157(18):2055–62.
Calello DP, Alpern ER, McDaniel-Yakscoe M, Garrett BL, Shaw KN, Osterhoudt KC. Observation unit experience for pediatric poison exposures. J Med Toxicol. 2009;5(1):15–9.
Dribben W, Welch J, Dunn D, Kirk M. The utilization of emergency department observation units for the poisoned patient. Clin Toxicol. 1999;37(5):583–675.
Gummin DD, Butler JR, Roberts RR, Erickson TB. Utilization of an emergency department observation unit for acute intoxications. Clin Toxicol. 1999;37(5):583–675.
Plumb J, Dudley NC, Herman BE, Kadish HA. Utilization of a pediatric observation unit for toxicologic ingestions. Pediatr Emerg Care. 2012;28(11):1169–72.
Wax PM, Kleinschmidt KC, Brent J. The Toxicology Investigators Consortium (ToxIC) Registry. J Med Toxicol. 2011;7:259–65.
Lemke T, Wang R. Emergency department observation for toxicologic exposures. Emerg Observation Med. 2001;19(1):155–67.
Zebrack M, Katish H, Nelson D. The pediatric hybrid observation unit: an analysis of 6477 consecutive patient encounters. Pediatr. 2005. doi:10.1542/peds.2004-0391.
Mace SE, Graff L, Mikhail M, Ross M. A national survey of observation units in the United States. Am J Emerg Med. 2003;21(7):529–33.
Baugh CW, Venkatesh AK, Hilton JA, Samuel PA, Schuur JD, Bohan JS. Making greater use of dedicated hospital observation units for many short-stay patients could save $3.1 billion a year. Health Aff. 2012;31(10):2314–23.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Judge, B.S., Ouellette, L.M., VandenBerg, M. et al. Utilization of Observation Units for the Care of Poisoned Patients: Trends from the Toxicology Investigators Consortium Case Registry. J. Med. Toxicol. 12, 111–120 (2016). https://doi.org/10.1007/s13181-015-0498-4
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13181-015-0498-4