Abstract
Acetaminophen (APAP) overdose is the most common pharmaceutical poisoning. The objective of this study was to examine the management of patients admitted for treatment of APAP overdose. Factors impacting hospital length of stay (LOS) were of particular interest. This was a retrospective cohort study of patients admitted to Kaiser Permanente Northern California hospitals for APAP overdose from July 2003 through December 2007. Medical records were abstracted for patient demographic data, key factors of overdose, California Poison Control System (CPCS) contact, data regarding hospital course, transfer for liver transplantation, and death. Four hundred thirty-five patients were included. The mean hospital LOS was 66.5 h (95% CI 62.1, 71.0). Four patients (0.9%) died. Eight patients (1.8%) were transferred for liver transplantation, but all of these patients later recovered without transplant. Of 289 cases eligible for placement on the Rumack–Matthew nomogram (acute ingestion with known time of ingestion <24 h and normal liver enzymes), 161 (55.7%) had APAP levels above the “200” line and 77 (26.6%) fell below the “150” line. CPCS was contacted in 295 cases (67.8%). Mean LOS in cases with CPCS consultation was 61.9 h (95% CI 57.2, 66.5 h) versus 76.3 h (95% CI 66.6, 86.0 h) in those without. LOS in cases treated with IV NAC was 67.1 h (95% CI 57.7, 76.5 h) versus 66.4 h (95% CI 61.2, 71.5 h) in cases treated with oral NAC. Many patients admitted for APAP overdose had serum APAP levels below the minimum toxicity level. Use of IV NAC did not impact hospital LOS. CPCS consultation appeared to decrease mean hospital LOS.
Similar content being viewed by others
Introduction
Acetaminophen (APAP) overdose is the most common pharmaceutical poisoning reported to poison control centers and remains the number one cause of medication overdose mortality [1]. Unfortunately, little is known about the clinical management of APAP poisoning cases by community physicians. No studies examining the management of APAP overdose outside of academic medical centers or poison control centers currently exist.
Patients presenting with acute APAP overdose are risk stratified based on the Rumack–Matthew nomogram. The traditional treatment protocol for APAP poisoning in the USA consists of a 72-h course of oral N-acetylcysteine (NAC) [2–4]. More recently experts have recommended patient-tailored approaches to oral NAC treatment [5–12]. These protocols seek to truncate NAC therapy for patients showing evidence of recovery. Though definitive research evidence to “prove” efficacy of these protocols is lacking, many medical toxicologists have adopted these strategies based on anecdotal experiences. Most protocols depend on an undetectable serum APAP level and normal (or resolving) liver enzymes as clearance criteria. A shortened-course of oral NAC for selected cases of APAP poisoning has been recommended by practitioners from the California Poison Control System (CPCS) since before 2000 [5, 6], though no routine policy is in place.
In 2004, the US FDA approved an intravenous NAC preparation (Acetadote) giving practitioners another viable treatment option. The Acetadote package insert recommends a 21-h course of therapy [13]; however, this protocol may not be appropriate for all patients with APAP poisoning. Considerable controversy still exists within the toxicology community regarding the proper endpoints for NAC therapy regardless of the route used [14]. Treatment of patients with chronic or repeated APAP overdose present an even more complicated management problem.
This retrospective study was designed to examine the clinical management of admitted APAP poisoning patients by physicians in a community hospital setting. The aim was to describe the hospital course of patients admitted to our large, community hospital system for treatment of APAP overdose with particular focus on factors influencing hospital length of stay (LOS). It was hypothesized that LOS would be decreased by early activated charcoal (AC) use, CPCS consultation, early NAC use, and use of intravenous NAC. It was also hypothesized that hospital LOS would be markedly (>24 h) longer than the times of earliest laboratory evidence of clearance (the endpoint of most patient-tailored treatment algorithms).
Methods
This was a retrospective cohort study of all patients admitted for treatment of APAP poisoning to any hospital within our large, community-based hospital system. Kaiser Permanente Northern California (KPNC) records were searched for cases of APAP overdose admitted for antidotal therapy from July 2003 through December 2007. KPNC electronic hospital records were searched for hospital diagnoses of “acetaminophen overdose”, “drug overdose”, or “analgesic overdose” by ICD-9 codes (500911, 501231, 501623, 965.4, 965.4A, 977.9E, 977.9D, E850.4, E850.4A, E935.4, E935.4A, E950.0, E950.0A, 965.9, 965.8). Pharmacy records were then searched for patients receiving NAC therapy. Records of patients admitted for “overdose” and receiving NAC antidotal therapy were reviewed for possible study inclusion. The Kaiser Foundation Research Institute investigational review board approved this study.
Study Setting
KPNC is a large, integrated healthcare delivery system consisting of 21 medical centers throughout Northern California. These healthcare facilities provide comprehensive medical care for over 3.5 million patient members. Although three KPNC facilities have University-affiliated residency programs, these are not considered major academic centers. It is the author’s belief that the practice patterns of KPNC physicians mirror those of other community physicians (at non-academic medical centers).
No bedside toxicology consulting service existed within KPNC during the study period. Physicians within KPNC do, however, have phone access to the CPCS. The CPCS is a statewide telephone advice line providing poison and drug overdose information to healthcare providers and the lay public. Treatment decisions were ultimately at the discretion of the admitting physicians who were internal medicine physicians or pediatricians. No standardized treatment guidelines for acetaminophen overdose existed during the study period.
Commercially available intravenous N-acetylcysteine (Acetadote) has been on formulary at KPNC since 2005. Since its inclusion, this is the product available for use when IV NAC is ordered. Since the vast majority of our facilities do not have compounding pharmacies, extemporaneously prepared intravenous mucomyst is no longer available.
Inclusion/Exclusion Criteria
Any patient with hospital admission for APAP poisoning was eligible for study inclusion. Children as well as adults were included. Exclusion criteria were: primary diagnosis other than APAP poisoning (not including liver failure secondary to APAP overdose), any “significant” co-ingested drug or medication, transfers into the KPNC system where NAC therapy was initiated prior to arrival, or cases where hospital records were not available. Significant co-ingestion was defined as any co-ingestant overdose that caused alteration of mental status such that the patient could not give history in the emergency department (unless AMS was felt due to APAP-induced liver toxicity) or that required additional, specific antidotal therapy (e.g., naloxone, etc.). No attempt was made to analyze cases of APAP overdose that were evaluated and released from the emergency department.
Data Collection
KPNC uses an extensive computerized medical record system throughout its hospitals, pharmacies, and laboratories. These computerized medical records were queried to extract patient demographic data, emergency department and hospital times, activated charcoal administration, NAC antidote formulations, and pertinent laboratory results. Medical records for all cases meeting inclusion criteria were reviewed by a single reviewer (SRO) to determine the reported time of APAP ingestion, any co-ingested medications, timing of ingestion (acute vs. chronic), type of ingestion (intentional vs. accidental), presence of known pre-existing liver or renal disease, times of psychiatry consultation, notation of poison control center call, transfer for liver transplantation, and death. When multiple entries for time of ingestion occurred, the time recorded in the admitting physician’s note was entered for study purposes. No attempt was made to determine APAP dosage, therapeutic medications lists, or NAC stop times. Unfortunately, NAC stop times were unreliably recorded in the medical records. Cases of acute overdose receiving APAP levels between 4 and 24 h of ingestion were evaluated for Rumack–Matthew nomogram placement using formulas derived by Rumack and White [15]. Cases presenting with liver enzyme elevation (AST > 60 IU/L, ALT > 60 IU/L) and/or INR elevation (>1.3) were not considered eligible for Rumack–Matthew nomogram placement. All data were entered into a standardized data collection instrument.
CPCS computerized records were also queried for cases of APAP overdose originating from any Kaiser Permanente Northern California healthcare facility. Patient names on this list were compared with the study patient list to determine whether the CPCS had been contacted for information regarding the case. Cases where no call was found within the CPCS records but notation was made of a discussion with a poison control center, were considered to have been managed in consultation with the CPCS.
The KPNC mortality database was reviewed to capture possible cases of APAP overdose resulting in death not captured during the initial review. This database tracks mortality data, including date of death, for Kaiser members and is used primarily for research purposes.
In order to estimate potential times to completion of NAC therapy using patient-tailored protocols [5, 6, 10], a theoretical model for predicting when patients might have been cleared from antidotal therapy was developed. The “earliest laboratory evidence of clearance time” was defined as the time when available labs demonstrated that the APAP level was undetectable (less than 10 μg/mL) and the patient’s liver transaminases were normal (AST < 60 IU/L, ALT < 60 IU/L). In the event that liver enzymes were elevated at any point during the hospitalization, lab evidence of clearance was considered to have occurred when the serum APAP level was undetectable (<10 μg/mL) and liver enzymes were decreasing and less than 1,000 IU/L.
Data Analysis
All data were entered directly into a Microsoft Excel spreadsheet developed a priori for study data entry. Rumack–Matthew nomogram placement was determined using formulas derived and published by White and Rumack [15]. Statistical analysis was performed with STATA statistical software (Stata Corp., Version 11.0, College Station, TX). Data were described using simple, descriptive statistics. 95% confidence intervals (CI) are provided where appropriate. Comparison of means was performed with Student’s t test. Relationships between certain continuous variables were described using correlation coefficients.
Results
Six hundred and nineteen cases of APAP overdose were admitted to KPNC hospitals during the study period. In 25 cases (4.0%), no hospital chart was available for review. Seventy-one cases (11.5%) were transfers from outside hospitals and therefore excluded. Eighty-eight cases (14.2%) were excluded due to significant co-ingestants. The study dataset therefore consisted of 435 cases (70.3%). Description of study cases is in Table 1. One hundred and thirteen patients (26.0%) were admitted to intensive care units, 11 (2.5%) to transitional (intermediate) care units, 308 (70.8%) to ward beds, and three (0.69%) patients were admitted by the hospital medicine service but never left the emergency department.
There were seven cases with pre-existing liver disease on hospital admission. These consisted of 4 cases of hepatitis C with mild liver enzymes elevations, two cases of alcoholic hepatitis without liver enzyme elevation, and one case of hepatitis B without liver enzyme elevation. All seven of these cases received CPCS consultation. All seven were treated with oral NAC. None died or were transferred for liver transplantation.
There were two cases with known pre-existing renal disease. One was a patient with documented renal insufficiency and creatinine of 1.6 mg/dL. The other was a patient with renal failure and on hemodialysis. This patient received CPCS consultation and received intravenous NAC therapy. Both of these patients recovered and neither were transferred for liver transplantation.
There were four deaths during the study period. (See Table 2) eight patients were transferred out of our hospital system for consideration of liver transplant. All eight patients eventually recovered without transplantation.
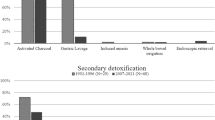
One hundred and sixty-one patients (37%) received AC in the ED. Fifty-five of these cases (34.2%) were associated with co-ingestant ingestions. Time from ingestion to AC administration (mean 5.8 h; 95% CI = 4.9, 6.7) was mildly correlated with hospital LOS (r = 0.22; p = 0.0057). Of patients receiving AC, those treated within 4 h of ingestion had a mean hospital LOS of 56.0 h (95% CI = 50.1, 61.9) versus 60.1 h (95% CI = 53.1, 67.1) in those who were not. (Difference in means = 4.1 h; 95% CI = −4.9, 13.1)
Two hundred and eighty patients (64.3%) had a documented CPCS phone consultation. In 15 cases (3.5%) no documentation of CPCS consultation was found, but a discussion with poison control was documented in the medical record. Therefore 295 patients (67.8%) were managed with CPCS consultation by telephone. Patients receiving CPCS consultation were similar to those who did not in baseline characteristics (Table 3). There was one death (0.3%; 95% CI = −0.3, 1.0) in the group of patients receiving CPCS consultation versus three deaths (2.1%; 95% CI = −0.2, 4.5) in the group that did not. Mean hospital LOS was significantly shorter among patients who received CPCS consultation (difference in means = 14.4 h; 95% CI = 5.0, 23.9 h).
There was a higher percentage of cases with serum APAP levels falling below the “150” line of the Rumack–Matthew nomogram in the group of patients who received CPCS consultation (30.5% vs 18.5%). When those cases with levels falling below the “150” line were removed from the LOS analysis, CPCS consultation was still associated with shorter hospital LOS (66.1 h versus 79.9 h; difference in means = 13.8 h; 95% CI = 3.0, 24.7).
Time from ingestion to NAC administration was correlated with hospital LOS (r = 0.16; p = 0.0033). Patients receiving NAC within 8 h of ingestion had a mean hospital LOS of 56.2 h (95% CI = 51.5, 60.9) versus 66.8 h (95% CI = 60.5, 73.1) for those who did not. (Difference in means = 10.6 h; 95% CI = 2.6, 18.6)
One hundred and three patients (23.7%) were treated with IV NAC and 325 (74.7%) treated with oral NAC (Table 4). In seven cases (1.6%) the exact NAC formulation could not be determined. We observed a steady increase in IV NAC use throughout the study period with no cases in 2003 to 53 cases (49%) in 2007 (see Table 5). We found no difference in hospital LOS for patients treated with IV NAC (mean 67.1 h; 95% CI = 57.65, 76.5) versus those treated with oral NAC (mean, 66.4 h; 95% CI = 61.2, 71.5) (difference in means = 0.7 h; 95% CI = −9.8, 11.3 h). All four deaths occurred in the oral NAC group.
The mean ED LOS was 5.8 h (95% CI = 5.4, 6.3 h). The mean hospital LOS for all cases throughout the study period was 66.5 h (95% CI = 62.1, 71.0 h). Annual mean hospital LOS is shown in Table 5. Mean time from presentation to the earliest laboratory evidence of clearance was 30.3 h (95% CI = 27.8, 32.8 h). The mean time from earliest laboratory evidence of clearance to discharge was 35.0 h (95% CI = 31.8, 38.2 h).
Limitations
Our study is subject to the limitations inherent to chart review data including recording bias. The most important areas of concern are the actual product taken in overdose and the exact time of ingestion. These data points are of particular concern as they are collected from third party information (patient to clinician to medical record) and might directly affect our findings. We do, however, feel that that the recorded times of ingestion are likely to accurately reflect clinician estimates used to make treatment decisions. Data on reported dose of acetaminophen ingested was not collected, as this information was inconsistently and unreliably recorded in the medical record.
Administration of NAC was used as a search criterion to identify eligible patients, therefore any cases of APAP overdose that were managed without NAC therapy would have been missed. As NAC is widely available and the well-known antidote for APAP overdose, it is likely that very few cases (if any) would be managed without ever receiving NAC.
Decisions to obtain CPCS consultation were made by treating clinicians. Therefore it is possible that cases where CPCS consultation was sought could have been inherently different. It is logical that consultation would be more likely in cases that were complicated or higher acuity. Therefore, observed differences in CPCS case outcomes should be evaluated with this limitation in mind.
We made an attempt to estimate when patients might have been cleared from NAC therapy based on patient-tailored protocols by calculating the time of “earliest laboratory evidence of clearance”. This was compared with actual hospital LOS to estimate where efficiency improvements might be made. Unfortunately this estimation is dependent on laboratory tests ordered by clinicians at the time of treatment. We had no control over the timing of available lab draws. It is likely that more accurate estimates could be possible were scheduled labs available.
Discussion
This study examined a large cohort of patients admitted to KPNC hospitals for treatment of uncomplicated APAP poisoning. This is the first study to describe the clinical management of APAP overdose within a community (non-academic) hospital system.
Death due to APAP overdose was rare, occurring in only four patients (0.9%). This mortality rate is consistent with previous studies of patients treated for APAP overdose [14, 16, 17]. Although several patients were transferred for possible liver transplantation, no patients actually received transplant.
A large number of acute overdose patients (approximately 27%) were admitted for treatment despite serum APAP levels below the “150” treatment line on the Rumack–Matthew nomogram. While some cases may have been properly treated due to historical nuances, many of these likely represent patients who required neither NAC nor hospital admission [3]. These patients were hospitalized for an average of 2 days. While this study was not designed to explore the reasons for admission in these cases, it is unlikely that psychiatric evaluation was a significant factor as this is not the usual practice in our facilities. Desire for extra caution or a lack of familiarity with treatment guidelines by clinicians may account for some of these admissions. It is possible that improved toxicological evaluation would decrease the number of hospital admission days in this cohort.
Patients were hospitalized, on average, for nearly 3 days. While this average LOS is somewhat shorter than would be expected with the 72-h NAC treatment protocol previously advocated, patients appear to stay in the hospital much longer than would be predicted using patient-tailored NAC treatment protocols. The average time from earliest laboratory evidence of clearance to hospital discharge was 35 h. This calculation was performed in an attempt to measure the potential impact of routine use of patient-tailored NAC treatment protocols. [5, 6, 10] The maximum potential impact in this cohort was 157 hospital admission days per year (Total earliest laboratory clearance to DC hours/24 h/3.5 years). While it is clear that patients could never be discharged immediately upon laboratory clearance, this represents an area where meaningful efficiency improvements could be made in the management of APAP overdose patients.
Little literature exists examining the effects of poison control center telephone contact and/or medical toxicology consultation on the hospital course of overdose patients. Current data suggests that availability of poison control center telephone consultation decreases healthcare resource utilization mostly by decreasing ED presentations and hospital admissions after toxicological exposures [18–20]. Studies evaluating the impact of poison control center contact on hospital LOS, however, are mixed. Data from a statewide database of hospital admissions demonstrated a 3-day shorter hospital LOS for overdose patients who received poison center consultations versus those who did not [21]. Another, recent study comparing poison center call volumes and hospital LOS was unable to identify any such correlation [22]. Two past studies examine the effects of hospital medical toxicology services on resource utilization. Both involved evaluation of toxicology patients admitted before and after availability of toxicology consultation services. One study found a significant decrease in hospital LOS among patients receiving consultation [23]. The other study examined the management of TCA overdose and did not find any difference in LOS [24]. This study did, however, identify a decrease in general resource utilization. It should be noted that none of these studies examined APAP overdose admissions specifically (the most common cause of medication overdose). Within our system clinical toxicology consultation was not available during the study period, but two thirds of patients were managed with CPCS consultation by telephone. When compared with patients managed without CPCS, these patients had a significantly shorter hospital length of stay. Our findings support the conclusion that toxicology consultation by CPCS does impact hospital LOS.
There was a significant increase in the use of IV NAC antidote during the study period. IV NAC was used in no cases in 2003 then steadily increased to half of cases in 2007 (see Table 5) This increase in parenteral antidote use corresponds to US FDA approval of IV NAC (Acetadote®) in 2004, the subsequent marketing that followed, and inclusion into the KPNC formulary in 2005. Interestingly, this study did not demonstrate a decrease in LOS for admitted APAP poisoning patients despite this increase in IV NAC use.
All four deaths occurred in patients treated with oral NAC and prior to 2006. Unfortunately these numbers are too small to formulate any concrete conclusions. There were no deaths in the IV NAC group. Rates of allergic reactions related to IV NAC use were not collected.
It is generally accepted that both oral and IV NAC are equally effective for the treatment of APAP overdose [4, 14, 25]. Though one recent study suggested that IV NAC may slightly decrease the risk of hepatotoxicity in patients starting treatment early [26], most toxicologists consider either formulation to provide adequate hepatic protection. Debate, however, exists over which formulation is preferable from a resource utilization standpoint. While the FDA approved IV NAC formulation (Acetadote®) is more expensive, it is considered to be easier to use and better tolerated by patients. Despite its higher price, some authors have suggested that Acetadote® is actually more cost effective than oral NAC [16, 26–29]. The basis for this assertion is Acetadote’s 20-h treatment regimen and a presumed decrease in hospitalization time. Our data did not support the conclusion that IV NAC use decreases hospital LOS. While strict adherence to recommended IV 21-h protocols might have changed this result, it is not clear that Acetadote® dosing, as outlined in the package insert, is appropriate in all cases of APAP poisoning. This study cannot explain why IV NAC had no effect on hospital LOS but possible reasons include the use of longer courses of IV NAC, a desire to observe patients after completion of the course of therapy, and/or disposition issues that delayed discharge (e.g., psychiatric consultation and/or placement).
Areas for future research might include the evaluation of hospital management after institution of routine APAP overdose management protocols within community hospital systems and/or evaluation of patient care before and after availability of a clinical toxicology consultation service.
Conclusions
In this cohort of patients admitted for treatment of APAP overdose, patients appeared to be managed safely. A large percentage of acute overdose patients were admitted with APAP levels falling below the Rumack–Matthew treatment line, perhaps unnecessarily. The time from lab evidence of clearance to hospital discharge may represent an area that could be improved in managing these patients. Hospital LOS was significantly shorter in patients who received CPCS telephone consultation. There was no decrease in LOS associated with IV NAC use.
References
Bronstein AC, Spyker DA, Cantilena LR, Green JL, Rumack BH, Heard SE (2008) 2007 Annual report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 25th Annual Report. Clin Toxicol 46(10):927–1057
Rumack BH, Matthew H (1975) Acetaminophen poisoning and toxicity. Pediatrics 55:871–876
Rumack BH (2002) Acetaminophen hepatotoxicity: The first 35 years. J Toxicol Clin Toxicol 40:3–20
Prescott L (2005) Oral or intravenous N-acetylcysteine for acetaminophen poisoning? Ann Emerg Med 45:409–413
Woo OF, Mueller PD, Olson KR, Anderson IB, Kim SY (2000) Shorter duration of oral N-acetylcysteine therapy for acute acetaminophen overdose. Ann Emerg Med 35(4):363–368
Betten DP, Cantrell FL, Thomas SC, Williams SR, Clark RF (2007) A prospective evaluation of shortened course oral N-acetylcysteine for the treatment of acute acetaminophen poisoning. Ann Emerg Med 50(3):272–279
Dart RC, Rumack BH (2007) Patient-tailored acetylcysteine administration. Ann Emerg Med 50(3):280–281
Yip L, Dart RC (2003) A 20-hour treatment for acetaminophen overdose. N Engl J Med 348(24):2471–2472
Tsai CL, Fang CC, Walson PD (2008) Key features of the patient-tailored N-acetylcysteine protocol. Ann Emerg Med 51(4):451–452
Tsai CL, Chang WT, Weng TI, Fang CC, Walson PD (2005) A patient-tailored N-acetylcysteine protocol for acute acetaminophen intoxication. Clin Ther 27(3):336–341
Kociancic T, Reed MD (2003) Acetaminophen intoxication and length of treatment: how long is long enough? Pharmacotherapy 23(8):1052–1059
Smilkstein MJ, Bronstein AC, Linden C, Augenstein KKW, Rumack BH (1991) Acetaminophen overdose: 48-hour intravenous N-acetylcysteine treatment protocol. Ann Emerg Med 20(10):1058–1063
Cumberland Pharmaceuticals. Acetadote website. Prescribing information. Available at: http://www.acetadote.net/locator/index.php. Accessed 12 July 2010
Heard KJ (2008) Acetylcysteine for acetaminophen poisoning. N Engl J Med 359(3):285–292
White SJ, Rumack BH (2005) The acetaminophen toxicity equations: “Solutions” for acetaminophen toxicity based on the Rumack–Matthew nomogram. Ann Emerg Med 45(5):563–564
Buckley NA, Whyte IM, O'Connell DL, Dawson AH (1999) Oral or intravenous N-acetylcysteine: which is the treatment of choice for acetaminophen (paracetamol) poisoning? J Toxicol Clin Toxicol 37(6):759–767
Prescott LF, Illingworth RN, Critchley JA, Stewart MJ, Adam RD, Proudfoot AT (1979) Intravenous N-acetylcystine: the treatment of choice for paracetamol poisoning. Br Med J 2(6198):1097–1100
Zaloshnja E, Miller T, Jones P, Litovitz T, Coben J, Steiner C et al (2006) The potential impact of poison centers on rural hospitalization rates for poisoning. Pediatrics 118(5):2094–2100
Miller TR, Lestina DC (1997) Costs of poisoning in the United States and savings from poison control centers: a cost-benefit analysis. Ann Emerg Med 29(2):239–245
Polivka BJ, Elliott MB, Wolowich WR (2002) Comparison of poison center exposure data: NHIS and TESS data. J Toxicol Clin Toxicol 40(7):839–845
Vassilev ZP, Marcus SM (2007) The impact of a poison control center on the length of hospital stay for patients with poisoning. J Toxicol Environ Health 70:107–110
Albertson TE, Tharratt RS, Marquardt K, Alsop J, Ninomiya JK, Foulke GE (2008) Poisoning hospitalization correlates with poison center call frequency. J Med Toxicol 4(3):151–156
Lee V, Kerr JF, Braitberg G, Louis WJ, O'Callaghan CJ, Frauman AG et al (2001) Impact of a toxicology service on a metropolitan teaching hospital. Emerg Med (Fremantle) 13(1):37–42
Clark RF, Williams SR, Nordt SP, Pearigen PD, Deutsch R (1998) Resource-use analysis of a medical toxicology consultation service. Ann Emerg Med 31(6):705–709
Hendrickson RG, Bizovi KE (2006) Acetaminophen. In: Flomenbaum N, Goldfrank L, Hoffman R, Howland M, Lewin N, Nelson L (eds) Goldfrank’s toxicologic emergencies, 8th edn. McGraw-Hill, New York, pp 523–543
Yarema MC, Johnson DW, Berlin RJ, Sivilotti ML, Nettel-Aguirre A, Brant RF et al (2009) Comparison of the 20-hour intravenous and 72-hour oral acetylcysteine protocols for the treatment of acute acetaminophen poisoning. Ann Emerg Med 54(4):606–614
Culley CM, Krenzelok EP (2005) A clinical and pharmacoeconomic justification for intravenous acetylcysteine: a US perspective. Toxicol Rev 24(2):131–143
Martello JL, Pummer TL, Krenzelok EP (2010) Cost minimization analysis comparing enteral N-acetylcysteine to intravenous acetylcysteine in the management of acute acetaminophen toxicity. Clin Toxicol (Phila) 48(1):79–83
Marchetti A, Rossiter R (2009) Managing acute acetaminophen poisoning with oral versus intravenous N-acetylcysteine: a provider-perspective cost analysis. J Med Econ 12(4):384–391
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding source
Kaiser Permanente Northern California Community Benefits Research Program Grant 2008
Rights and permissions
About this article
Cite this article
Offerman, S.R. The Clinical Management of Acetaminophen Poisoning in a Community Hospital System: Factors Associated with Hospital Length of Stay. J. Med. Toxicol. 7, 4–11 (2011). https://doi.org/10.1007/s13181-010-0115-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13181-010-0115-5