Abstract
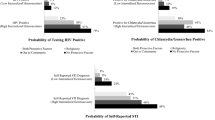
The present study sought to identify patterns and predictors of disclosure of sexual orientation to healthcare providers among lesbian, gay, and bisexual (LGB) adults. Respondents were 396 self-identified LGB individuals ages 18–59, recruited from diverse community venues in New York City, with equal numbers of men and women and Whites, Blacks, and Latinos. Respondents were interviewed at baseline and 1-year follow-up. We assessed the relationships among disclosure of sexual orientation, demographic characteristics, health, and minority stress. Rates of nondisclosure to healthcare providers were significantly higher among bisexual men (39.3 %) and bisexual women (32.6 %) compared with gay men (10 %) and lesbians (12.9 %). Bivariate and multivariate logistic regression models predicting disclosure of sexual orientation indicated that patient age, level of education, immigration status, medical history, level of internalized homophobia, and degree of connectedness to the LGBT community were significant factors, along with sexual identity. Nondisclosure of sexual orientation was related to poorer psychological well-being at 1 year follow-up. Our findings suggest that interventions targeting sexual minorities ought to carefully tailor messages to subpopulations. In particular, interventionists and clinicians ought to be mindful of differences between bisexually and gay/lesbian-identified individuals.
Similar content being viewed by others
References
American Association for Public Opinion Research. (2005). Standard definitions: Final dispositions of case codes and outcome rates for surveys. Deerfield, IL: Author. Retrieved from http://www.aapor.org/pdfs/standarddefs_3.1.pdf.
Barbara, A. M., Quandt, S. A., & Anderson, R. T. (2001). Experiences of lesbians in the health care environment. Women & Health, 34, 45–62.
Bernstein, K. T., Liu, K., Begier, E. M., Koblin, B., Karpati, A., & Murrill, C. (2008). Same-sex attraction disclosure to health care providers among New York City men who have sex with men: Implications for HIV testing approaches. Archives of Internal Medicine, 168, 1458–1464.
Boehmer, U., & Case, P. (2004). Physicians don’t ask, sometimes patients tell: Disclosure of sexual orientation among women with breast carcinoma. Cancer, 101, 1882–1889.
Conger, R. D., Wallace, L. E., Sun, Y., Simmons, R. L., McLoyd, V. C., & Brody, G. H. (2002). Economic pressure in African American families: a replication and extension of the family stress model. Developmental Psychology, 38, 179–193.
Conron, K. J., Mimiaga, M. J., & Landers, S. J. (2010). A population-based study of sexual orientation identity and gender differences in adult health. American Journal of Public Health, 100, 1953–1960.
Drabble, L., Keatley, J., & Marcelle, G. (2003). Progress and opportunities in lesbian, gay, bisexual, and transgender health communications. Clinical Research and Regulatory Affairs, 20, 205–227.
Eliason, M. J., & Schope, R. (2001). Does “Don’t Ask Don’t Tell” apply to health care? Lesbian, gay, and bisexual people’s disclosure to health care providers. Journal of the Gay and Lesbian Medical Association, 5, 125–134.
Fredriksen-Goldsen, K. I., Kim, H., Barkan, S. E., Balsam, K. F., & Mincer, S. L. (2011). Disparities in health-related quality of life: a comparison of lesbians and bisexual women. American Journal of Public Health, 100, 2255–2261.
Frost, D. M., & Meyer, I. H. (2012). Measuring community connectedness among diverse sexual minority populations. Journal of Sex Research, 49, 36–49.
Frost, D. M., Lehavot, K., & Meyer, I. H. (2011, August). Minority stress and physical health among sexual minorities. Poster presented at the 119th Annual Convention of the American Psychological Association, Washington, DC
Gates, G. J. (2011). How many people are lesbian, gay, bisexual, and transgender? Retrieved from The Williams Institute website: http://williamsinstitute.law.ucla.edu/wp-content/uploads/Gates-How-Many-People-LGBT-Apr-2011.pdf. Accessed 26 July 2012.
Heck, J. E., Sell, R. L., & Gorin, S. S. (2006). Health care access among individuals involved in same-sex relationships. American Journal of Public Health, 96, 1111–1118.
Herek, G. M., & Garnets, L. D. (2007). Sexual orientation and mental health. Annual Review of Clinical Psychology, 3, 353–375.
Herek, G. M., & Glunt, E. K. (1995). Identity and community among gay and bisexual men in the AIDS era: Preliminary findings from the Sacramento Men’s Health Study. In G. M. Herek & B. Greene (Eds.), AIDS, identity, and community: The HIV epidemic and lesbians and gay men (pp. 55–84). Thousand Oaks, CA: Sage.
Institute of Medicine. (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. Washington, DC: The National Academies Press.
King, M., Semlyen, J., See Tai, S., Killaspy, H., Osborn, D., Popelyuk, D., & Nazareth, I. (2008). A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry, 18, 70–87.
Klitzman, R. L., & Greenberg, J. D. (2002). Patterns of communication between gay and lesbian patients and their health care providers. Journal of Homosexuality, 42, 65–75.
Labig, C. E., Jr., & Peterson, T. O. (2006). Sexual minorities and selection of a primary care physician in a Midwestern U.S. city. Journal of Homosexuality, 51, 1–5.
Lease, S. H., Horne, S. G., & Noffsinger-Frazier, N. (2005). Affirming faith experiences and psychological health for Caucasian lesbian, gay, and bisexual individuals. Journal of Counseling Psychology, 52, 378–388.
Lindley, L. L., Walsemann, K. M., & Carter, J. W. (2011). The association of sexual orientation measures with young adults’ health-related outcomes. American Journal of Public Health, 102, 1177–1185.
Link, B. G. (1987). Understanding labeling effects in the area of mental disorders: an assessment of the effects of expectations of rejection. American Sociological Review, 52, 96–112.
Martin, J. L., & Dean, L. (1987). Summary of measures: mental health effects of AIDS on at-risk homosexual men. Unpublished manuscript.
Meyer, I. H. (1995). Minority stress and mental health in gay men. Journal of Health and Social Behavior, 36, 38–56.
Meyer, I. H. (2003). Prejudice, social stress and mental health in lesbian, gay, and bisexual populations: conceptual issues and research evidence. Psychological Bulletin, 129, 674–697.
Meyer, I. H., Rossano, L., Ellis, J. M., & Bradford, J. (2002). A brief telephone interview to identify lesbian and bisexual women in random digit dialing sampling. Journal of Sex Research, 39, 139–144.
Pachankis, J. E. (2007). The psychological implications of concealing a stigma: a cognitive-affective-behavioral model. Psychological Bulletin, 133, 328–345.
Petroll, A. E., & Mosack, K. E. (2011). Physician awareness of sexual orientation and preventive health recommendations to men who have sex with men. Sexually Transmitted Diseases, 38, 63–67.
Riggle, E. D. B., Rostosky, S. S., & Danner, F. (2009). LGB identity and eudaimonic well being in midlife. Journal of Homosexuality, 56, 786–798.
Ryff, C. D. (1989). Happiness is everything, or is it? Explorations of the meaning of psychological well-being. Journal of Personality and Social Psychology, 57, 1069–1081.
Ryff, C. D., & Keyes, C. L. M. (1995). The structure of psychological well-being revisited. Journal of Personality and Social Psychology, 69, 719–727.
St. Pierre, M. (2012). Under what conditions do lesbians disclose their sexual orientation to healthcare providers? A review of the literature. Journal of Lesbian Studies, 16, 199–219.
Stein, G. L., & Bonuck, K. A. (2001). Physician–patient relationships among the lesbian and gay community. Journal of the Gay and Lesbian Medical Association, 5, 87–93.
The Fenway Institute (2012). How to gather data about sexual orientation and gender identity in clinical settings. Retrieved from The Fenway Institute website: http://www.fenwayhealth.org/site/DocServer/Policy_Brief_HowtoGather..._v3_01.09.12.pdf?docID=9142
The Joint Commission (2011). Advancing effective communication, cultural competence, and patient- and family- centered care for the lesbian, gay, bisexual, and transgender (LGBT) community: a field guide. Oak Brook, IL.
U.S. Department of Health and Human Services, Health Resources and Services Administration. (2011). Women’s health USA 2011. Rockville, Maryland: U.S. Department of Health and Human Services.
van Dam, M. A., Koh, A. S., & Dibble, S. L. (2001). Lesbian disclosure to health care providers and delay of care. Journal of the Gay and Lesbian Medical Association, 5, 11–19.
Ware, J. E., Kosinski, M., Turner-Bowker, D. M., & Gandek, B. (2002). Introduction. In How to score version 2 of the SF-12 Health Survey; pp. 3-8. Lincoln, RI, & Boston, MA: QualityMetric Inc., & Health Assessment Lab.
Williams, D. R., Spencer, M. S., & Jackson, J. S. (1999). Race, stress, and physical health. In R. J. Contrada & R. D. Ashmore (Eds.), Self, social identity, and physical health (pp. 71–100). NY: Oxford University Press.
Acknowledgments
This research was supported by the National Institute of Mental Health grant R01-MH066058 to Ilan H. Meyer, Principal Investigator. The authors report no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Durso, L.E., Meyer, I.H. Patterns and Predictors of Disclosure of Sexual Orientation to Healthcare Providers Among Lesbians, Gay Men, and Bisexuals. Sex Res Soc Policy 10, 35–42 (2013). https://doi.org/10.1007/s13178-012-0105-2
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13178-012-0105-2