Abstract
Background
Programmed cell death-1 (PD-1)/programmed cell death ligand-1 (PD-L1) immune checkpoint inhibitors (ICIs) significantly affect outcomes in non-small cell lung cancer (NSCLC) patients. However, differences in reactions toward PD-1/PD-L1 ICI among patients impose inefficient treatment. Therefore, developing a reliable biomarker to predict PD-1/PD-L1 ICI reaction is highly necessary for predictive, preventive, and personalized (3P) medicine.
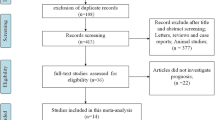
Materials and methods
We recruited 63 patients from the National Cancer Center (NCC) and classified them into the training and validation sets. Next, 99 patients were recruited for inclusion into the external validation set at the Samsung Medical Center (SMC). Proteomic analysis enabled us to identify plasma C7 levels, which were significantly different among groups classified by their overall response to the RECIST V 1.1–based assessment. Analytical performance was evaluated to predict the PD-1/PD-L1 ICI response for each type of immunotherapy, and NSCLC histology was evaluated by determining the C7 levels via ELISA.
Results
Plasma C7 levels were significantly different between patients with and without clinical benefits (PFS ≥ 6 months). Among the groups sorted by histology and PD-1/PD-L1 immunotherapy type, only the predicted accuracy for pembrolizumab-treated patients from both NCC and SMC was greater than 73%. In patients treated with pembrolizumab, C7 levels were superior to those of the companion diagnostics 22C3 (70.3%) and SP263 (62.1%). Moreover, for pembrolizumab-treated patients for whom the PD-L1 tumor proportion score (TPS) was < 50%, the predictive accuracy of C7 was nearly 20% higher than that of 22C3 and SP263.
Conclusion
Evaluation of plasma C7 levels shows an accurate prediction of NSCLC patient reactions on pembrolizumab. It demonstrates plasma C7 is an alternative and supportive biomarker to overcome the predictive limitation of previous 22C3 and SP263. Thus, it is clear that clinical use of plasma C7 allows predictive diagnosis on lung cancer patients who have not been successfully treated with current CDx and targeted prevention on metastatic diseases in secondary care caused by a misdiagnosis of current CDx. Reduction of patients’ financial burden and increased efficacy of cancer treatment would also enable prediction, prevention, and personalization of medical service on NSCLC patients. In other words, plasma C7 provides efficient medical service and an optimized medical economy followed which finally promotes the prosperity of 3P medicine.




Similar content being viewed by others
Availability of data and material
All raw data and materials are available from the corresponding authors upon reasonable request.
Code availability
Not applicable
Abbreviations
- 3P medicine:
-
Predictive, preventive, and personalized medicine
- C7:
-
Complement component 7
- PD-1:
-
Programmed cell death protein 1
- PD-L1:
-
Programmed cell death ligand 1
- ICI:
-
Immune checkpoint inhibitor
- CDx:
-
Companion diagnostics
- NSCLC:
-
Non-small cell lung cancer
- NCC:
-
National Cancer Center
- SMC:
-
Samsung Medical Center
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- TMB:
-
Tumor mutation burden
- MS:
-
Mass spectroscopy
- AGC:
-
Automatic gain control
- HCD:
-
Higher-energy collisional dissociation
- IACUC:
-
Institutional Animal Care and Use Committee
- NCCI:
-
National Cancer Center Institute
- TDLN:
-
Tumor-draining lymph node
- ECL:
-
Enhanced chemiluminescence
- AUC:
-
Area under the curve
- ACC:
-
Accuracy
- ROC:
-
Receiver operating characteristics
- N:
-
Number
- CR:
-
Complete responder
- PR:
-
Partial responder
- SD:
-
Stable disease
- PD:
-
Progressive disease
- responder:
-
Responder with clinical benefit (PFS ≥ 6 months)
- Non-responder:
-
Non-responder without clinical benefit (PFS < 6 months)
- ADC:
-
Adenocarcinoma
- SqCC:
-
Squamous cell carcinoma
- Other:
-
Other types of lung cancer
- CRO:
-
Contract research organization
- CRA:
-
Clinical research associate
- SEN:
-
Sensitivity
- SPE:
-
Specificity
- PPV:
-
Positive predictive value
- NPV:
-
Negative predictive value
References
Cha E, Wallin J, Kowanetz M. PD-L1 inhibition with MPDL3280A for solid tumors. In: Semin Oncol. WB Saunders; 2015:484–87. https://doi.org/10.1053/j.seminoncol.2015.02.002.
Gettinger SN, Shepherd FA, Antonia SJ, Brahmer JR, Chow LQM, Juergens RA, et al. First-line nivolumab (anti-PD-1; BMS-936558, ONO-4538) monotherapy in advanced NSCLC: Safety, efficacy, and correlation of outcomes with PD-L1 status. J Clin Oncol. 2014;32:8024. https://doi.org/10.1200/jco.2014.32.15_suppl.8024.
Genentech. FDA approves Genentech’s Tecentriq as a first-line monotherapy for certain people with metastatic non-small cell lung cancer. May 18, 2020. Available from: https://bit.ly/2ZfNjHK
US FDA. FDA approves durvalumab for extensive-stage small cell lung cancer. March 30, 2020. Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-durvalumab-extensive-stage-small-cell-lung-cancer
US FDA. FDA expands pembrolizumab indication for first-line treatment of NSCLC (TPS ≥1%). April 11, 2019. Available from: https://www.fda.gov/drugs/fda-expands-pembrolizumab-indication-first-line-treatment-nsclc-tps-1
US FDA. FDA approves atezolizumab for first-line treatment of metastatic NSCLC with high PD-L1 expression. May 18, 2020. Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-atezolizumab-first-line-treatment-metastatic-nsclc-high-pd-l1-expression
Horn L, Spigel DR, Vokes EE, Holgado E, Ready N, Steins M, et al. Nivolumab versus docetaxel in previously treated patients with advanced non–small-cell lung cancer: two-year outcomes from two randomized, open-label, phase III trials (CheckMate 017 and CheckMate 057). J Clin Oncol. 2017;35:3924. https://doi.org/10.1200/JCO.2017.74.3062.
Herbst RS, Baas P, Kim DW, Felip E, Perez-Gracia JL, Han JY, et al. Pembrolizumab versus docetaxel for previously treated, PD-L1-positive, advanced non-small-cell lung cancer (KEYNOTE-010): a randomised controlled trial. Lancet. 2016;387:1540–50. https://doi.org/10.1016/S0140-6736(15)01281-7.
Spira AI, Park K, Mazières J, Vansteenkiste JF, Rittmeyer A, Ballinger M, et al. Efficacy, safety and predictive biomarker results from a randomized phase II study comparing MPDL3280A vs docetaxel in 2L/3L NSCLC (POPLAR). J Clin Oncol. 2015;33(15_suppl):8010. https://doi.org/10.1200/jco.2015.33.15_suppl.8010.
Rittmeyer A, Barlesi F, Waterkamp D, Park K, Ciardiello F, Von Pawel J, et al. Atezolizumab versus docetaxel in patients with previously treated non-small-cell lung cancer (OAK): a phase 3, open-label, multicentre randomised controlled trial. Lancet. 2017;389:255–65. https://doi.org/10.1016/S0140-6736(16)32517-X.
Rangachari D, VanderLaan PA, Shea M, Le X, Huberman MS, Kobayashi SS, et al. Correlation between classic driver oncogene mutations in EGFR, ALK, or ROS1 and 22C3–PD-L1≥ 50% expression in lung adenocarcinoma. J Thorac Oncol. 2017;12:878–83. https://doi.org/10.1016/j.jtho.2016.12.026.
Smith J, Robida MD, Acosta K, Vennapusa B, Mistry A, Martin G, et al. Quantitative and qualitative characterization of two PD-L1 clones: SP263 and E1L3N. Diagnostic Pathol. 2016;11:1–9. https://doi.org/10.1186/s13000-016-0494-2.
Jazieh AR, Bounedjar A, Bamefleh H, Alfayea T, Almaghraby HQ, Belarabi A, et al. Expression of immune response markers in Arab patients with lung cancer. JCO Global Oncol. 2020;6:1218–24. https://doi.org/10.1200/GO.20.00107.
Ilie M, Long-Mira E, Bence C, Butori C, Lassalle S, Bouhel L, et al. Comparative study of the PD-L1 status between surgically resected specimens and matched biopsies of NSCLC patients reveal major discordances: a potential issue for anti-PD-L1 therapeutic strategies. Ann Oncol. 2016;27:147–53. https://doi.org/10.1093/annonc/mdv489.
Munari E, Zamboni G, Marconi M, Sommaggio M, Brunelli M, Martignoni G, et al. PD-L1 expression heterogeneity in non-small cell lung cancer: evaluation of small biopsies reliability. Oncotarget. 2017;8:90123. https://doi.org/10.18632/oncotarget.21485.
Paz-Ares L, Langer CJ, Novello S, et al. Pembrolizumab (pembro) plus platinum-based chemotherapy (chemo) for metastatic NSCLC: tissue TMB (tTMB) and outcomes in KEYNOTE-021, 189, and 407. Ann Oncol. 2019;30:851–934. https://doi.org/10.1093/annonc/mdz394.078.
Torlakovic E, Lim HJ, Adam J, Barnes P, Bigras G, Chan AWH, et al. Interchangeability of PD-L1 immunohistochemistry assays: a meta-analysis of diagnostic accuracy. Mod Pathol. 2020;33:4–17. https://doi.org/10.1038/s41379-019-0327-4.
Tsimafeyeu I, Imyanitov E, Zavalishina L, Raskin G, Povilaitite P, Savelov N, et al. Agreement between PDL1 immunohistochemistry assays and polymerase chain reaction in non-small cell lung cancer: CLOVER comparison study. Sci Rep. 2020;10:1–8. https://doi.org/10.1038/s41598-020-60950-2.
Munari E, Zamboni G, Sighele G, Marconi M, Sommaggio M, Lunardi G, et al. Expression of programmed cell death ligand 1 in non–small cell lung cancer: comparison between cytologic smears, core biopsies, and whole sections using the SP263 assay. Cancer Cytopathol. 2019;127:52–61. https://doi.org/10.1002/cncy.22083.
Li J, Jie HB, Lei Y, Gildener-Leapman N, Trivedi S, Green T, et al. PD-1/SHP-2 Inhibits Tc1/Th1 phenotypic responses and the activation of T cells in the tumor microenvironment. Cancer Res. 2015;75:508–18. https://doi.org/10.1158/0008-5472.
Li B, Li F, Huangyang P, Burrows M, Guo K, Riscal R, et al. FBP1 loss disrupts liver metabolism and promotes tumorigenesis through a hepatic stellate cell senescence secretome. Nat Cell Biol. 2020;22:728–39. https://doi.org/10.1038/s41556-020-0511-2.
Sawyers CL, Zhang Z, Karthaus WR, Lee YS, Gao VR, Wu C, et al. Tumor microenvironment-derived NRG1 promotes antiandrogen resistance in prostate cancer. Cancer Cell. 2020;38:279–96. https://doi.org/10.1016/j.ccell.2020.06.005.
Gerner C, Brunmair J, Bileck A, Stimpfl T, Rabile F, Favero GD, et al. Metabo-tip: a metabolomics platform for lifestyle monitoring supporting the development of novel strategies in predictive, preventive and personalised medicine. EPMA J. 2021;1–13(12):1–20. https://doi.org/10.1007/s13167-021-00241-6.
Kucera R, Pecen L, Topolcan O, Dahal AR, Costigliola V, Giordano FA, et al. Prostate cancer management: long-term beliefs, epidemic developments in the early twenty-first century and 3PM dimensional solutions. EPMA J. 2020;11:399–418. https://doi.org/10.1007/s13167-020-00214-1.
Golubnitschaja O, Baban B, Boniolo G, Wang W, Bubnov R, Kapalla M, et al. Medicine in the early twenty-first century: paradigm and anticipation. EPMA J. 2016;7(1):23. https://doi.org/10.1186/s13167-016-0072-4.
Aydin B, Caliskan A, Arga KY. Overview of Omics biomarkers in pituitary neuroendocrine tumors to design future diagnosis and treatment strategies. EPMA J. 2021;12:383–401. https://doi.org/10.1007/s13167-021-00246-1.
Demark-Wahnefried W, Rogers LQ, Gibson JT, Harada S, Frugé AD, Oster RA, et al. Randomized trial of weight loss in primary breast cancer: impact on body composition, circulating biomarkers and tumor characteristics. Int J Cancer. 2020;146:2784–96. https://doi.org/10.1002/ijc.32637.
Huizar CC, Raphael I, Forsthuber TG. Genomic, proteomic, and systems biology approaches in biomarker discovery for multiple sclerosis. Cell Immunol. 2020;358:104219. https://doi.org/10.1016/j.cellimm.2020.104219.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47. https://doi.org/10.1016/j.ejca.2008.10.026.
Smits N. A note on Youden’s J and its cost ratio. BMC Med Res Methodol. 2010;10:1–4. https://doi.org/10.1186/1471-2288-10-89.
Würzner R. Modulation of complement membrane attack by local C7 synthesis. Clin Exp Immunol. 2000;121:8. https://doi.org/10.1046/j.1365-2249.2000.01263.x.
Naughton MA, Walport MJ, Würzner R, Carter J, Alexander GJ, Goldman JM, et al. Organ-specific contribution to circulating C7 levels by the bone marrow and liver in humans. Eur J Immunol. 1996;26:2108–12. https://doi.org/10.1002/eji.1830260922.
Colten HR, Strunk RC. Synthesis of complement components in liver and at extrahepatic sites. Complement in health and disease. Dordrecht: Springer; 1993. p. 127–58. https://doi.org/10.1007/978-94-011-2214-6_4.
Morgan BP, Gasque P. Extrahepatic complement biosynthesis: where, when, and why? Clin Exp Immunol. 1997;107:1. https://doi.org/10.1046/j.1365-2249.1997.d01-890.x.
Funding
This study was funded by research grants from the National Cancer Center, Republic of Korea (NCC-2010161, and NCC-2110480-1), and InnoBation Bio Co., Ltd. (202000380001).
Author information
Authors and Affiliations
Contributions
This study was designed by JG Park, BK Choi, YJ Lee, SH Lee, and BC Yoo. Study material provision and patient recruitment were performed by YJ Lee and SH Lee. The data were collected and assembled by JG Park, BK Choi, YJ Lee, EJ Jang, SH Lee, and BC Yoo. All authors contributed to data analysis and interpretation. This manuscript was written by JG Park, BK Choi, YJ Lee, SH Lee, and BC Yoo. All authors contributed to the review and approved the final version of the manuscript. All authors had full access to all data and approved the submission of this manuscript for publication.
Corresponding authors
Ethics declarations
Ethics approval
This study was approved by the National Cancer Center Institutional Review Board (NCC-2017-0257) and the Samsung Medical Center Institutional Review Board (SMC-2018-04-048). All animal experiments were performed in accordance with the animal experimental guidelines and were approved by the Ethics Committee of the National Cancer Center, Republic of Korea.
Consent to participate
Written informed consent was obtained for each volunteer to participate in the study.
Consent for publication
Written informed consent was obtained from each volunteer for publishing the data.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jae Gwang Park, Beom Kyu Choi and Youngjoo Lee are co-first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Park, J.G., Choi, B.K., Lee, Y. et al. Plasma complement C7 as a target in non-small cell lung cancer patients to implement 3P medicine strategies. EPMA Journal 12, 629–645 (2021). https://doi.org/10.1007/s13167-021-00266-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13167-021-00266-x