Abstract
Purpose
To investigate the predictors of contralateral hypertrophy in patients treated with unilobar transarterial radioembolization (TARE) with yttrium-90-loaded resin microspheres due to unresectable right-liver tumors.
Methods
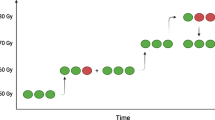
Patients who underwent right unilobar TARE with resin microspheres between May 2019 and September 2021 were screened retrospectively. Contralateral hypertrophy was evaluated by calculating the kinetic growth rate (KGR) in 8–10 weeks after TARE. The predictors of increased KGR were determined with linear regression analysis.
Results
A total of 24 patients (16 with primary and 8 with metastatic liver tumors) were included in the study. After right unilobar TARE, mean volume of the left lobe increased from 368.26 to 436.16 mL, while the mean volume of the right lobe decreased from 1576.22 to 1477.89 mL. The median KGR of the left lobe was 0.28% per week. The radiation dose absorbed by the healthy parenchyma of the right lobe was significantly higher in patients with increased KGR (31.62 vs. 18.78 Gy, p = 0.037). Linear regression analysis showed that the dose absorbed by healthy parenchyma was significantly associated with increased KGR (b = 0.014, p = 0.043).
Conclusion
Patients who received right unilobar TARE for liver malignancies could develop a substantial contralateral hypertrophy, and the radiation dose absorbed by the healthy parenchyma of the right lobe was significantly associated with increased KGR in the left lobe. TARE could have a role for inducing contralateral hypertrophy as it offers the advantage of concurrent local tumor control along with its hypertrophic effect.




Similar content being viewed by others
Data Availability
Contact the corresponding author for data requests.
References
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R, et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149:713–24.
Khan AS, Garcia-Aroz S, Ansari MA, Atiq SM, Senter-Zapata M, Fowler K, et al. Assessment and optimization of liver volume before major hepatic resection: current guidelines and a narrative review. Int J Surg. 2018;52:74–81.
Abdalla EK, Barnett CC, Doherty D, Curley SA, Vauthey JN. Extended hepatectomy in patients with hepatobiliary malignancies with and without preoperative portal vein embolization. Arch Surg 2022;137:675–80; discussion 80–1.
Hemming AW, Reed AI, Howard RJ, Fujita S, Hochwald SN, Caridi JG et al. Preoperative portal vein embolization for extended hepatectomy. Ann Surg 2003;237:686–91; discussion 91–3.
Isfordink CJ, Samim M, Braat M, Almalki AM, Hagendoorn J, Borel Rinkes IHM, et al. Portal vein ligation versus portal vein embolization for induction of hypertrophy of the future liver remnant: a systematic review and meta-analysis. Surg Oncol. 2017;26:257–67.
Aloia TA. Associating liver partition and portal vein ligation for staged hepatectomy: portal vein embolization should remain the gold standard. JAMA Surg. 2015;150:927–8.
Simoneau E, Hassanain M, Shaheen M, Aljiffry M, Molla N, Chaudhury P, et al. Portal vein embolization and its effect on tumour progression for colorectal cancer liver metastases. Br J Surg. 2015;102:1240–9.
Schadde E, Ardiles V, Robles-Campos R, Malago M, Machado M, Hernandez-Alejandro R, et al. Early survival and safety of ALPPS: first report of the International ALPPS Registry. Annals of Surgery. 2014;260:829–38.
Jakobs TF, Hoffmann R-T, Dehm K, Trumm C, Stemmler H-J, Tatsch K, et al. Hepatic yttrium-90 radioembolization of chemotherapy-refractory colorectal cancer liver metastases. J Vasc Interv Radiol. 2008;19:1187–95.
Shindoh J, Truty MJ, Aloia TA, Curley SA, Zimmitti G, Huang SY, et al. Kinetic growth rate after portal vein embolization predicts posthepatectomy outcomes: toward zero liver-related mortality in patients with colorectal liver metastases and small future liver remnant. J Am Coll Surg. 2013;216:201–9.
Kambakamba P, Stocker D, Reiner CS, Nguyen-Kim TD, Linecker M, Eshmuminov D, et al. Liver kinetic growth rate predicts postoperative liver failure after ALPPS. HPB (Oxford). 2016;18:800–5.
Giammarile F, Bodei L, Chiesa C, Flux G, Forrer F, Kraeber-Bodere F, et al. EANM procedure guideline for the treatment of liver cancer and liver metastases with intra-arterial radioactive compounds. Eur J Nucl Med Mol Imaging. 2011;38:1393–406.
Rayar M, Sulpice L, Edeline J, Garin E, Levi Sandri GB, Meunier B, et al. Intra-arterial yttrium-90 radioembolization combined with systemic chemotherapy is a promising method for downstaging unresectable huge intrahepatic cholangiocarcinoma to surgical treatment. Ann Surg Oncol. 2015;22:3102–8.
Gaba RC, Lewandowski RJ, Kulik LM, Riaz A, Ibrahim SM, Mulcahy MF, et al. Radiation lobectomy: preliminary findings of hepatic volumetric response to lobar yttrium-90 radioembolization. Ann Surg Oncol. 2009;16:1587–96.
Jakobs TF, Saleem S, Atassi B, Reda E, Lewandowski RJ, Yaghmai V, et al. Fibrosis, portal hypertension, and hepatic volume changes induced by intra-arterial radiotherapy with 90yttrium microspheres. Dig Dis Sci. 2008;53:2556–63.
Teo JY, Goh BK, Cheah FK, Allen JC, Lo RH, Ng DC, et al. Underlying liver disease influences volumetric changes in the spared hemiliver after selective internal radiation therapy with 90Y in patients with hepatocellular carcinoma. J Dig Dis. 2014;15:444–50.
Teo JY, Goh BK. Contra-lateral liver lobe hypertrophy after unilobar Y90 radioembolization: an alternative to portal vein embolization? World J Gastroenterol. 2015;21:3170–3.
Kulik LM, Carr BI, Mulcahy MF, Lewandowski RJ, Atassi B, Ryu RK, et al. Safety and efficacy of 90Y radiotherapy for hepatocellular carcinoma with and without portal vein thrombosis. Hepatology. 2008;47:71–81.
Salem R, Lewandowski RJ, Mulcahy MF, Riaz A, Ryu RK, Ibrahim S, et al. Radioembolization for hepatocellular carcinoma using yttrium-90 microspheres: a comprehensive report of long-term outcomes. Gastroenterology. 2010;138:52–64.
Khor AY-K, Toh Y, Allen JC, Ng DC-E, Kao Y-H, Zhu G, et al. Survival and pattern of tumor progression with yttrium-90 microsphere radioembolization in predominantly hepatitis B Asian patients with hepatocellular carcinoma. Hepatol Int. 2014;8:395–404.
Nalesnik MA, Federle M, Buck D, Fontes P, Carr BI. Hepatobiliary effects of 90yttrium microsphere therapy for unresectable hepatocellular carcinoma. Hum Pathol. 2009;40:125–34.
Carpizo DR, Gensure RH, Yu X, Gendel VM, Greene SJ, Moore DF, et al. Pilot study of angiogenic response to yttrium-90 radioembolization with resin microspheres. J Vasc Interv Radiol. 2014;25:297–306.e1.
Fernandez-Ros N, Inarrairaegui M, Paramo JA, Berasain C, Avila MA, Chopitea A, et al. Radioembolization of hepatocellular carcinoma activates liver regeneration, induces inflammation and endothelial stress and activates coagulation. Liver Int. 2015;35:1590–6.
Lewandowski RJ, Andreoli JM, Hickey R, Kallini JR, Gabr A, Baker T, et al. Angiogenic response following radioembolization: results from a randomized pilot study of yttrium-90 with or without sorafenib. J Vasc Interv Radiol. 2016;27:1329–36.
Birgin E, Rasbach E, Seyfried S, Rathmann N, Diehl SJ, Schoenberg SO, et al. Contralateral liver hypertrophy and oncological outcome following radioembolization with (90)Y-microspheres: a systematic review. Cancers (Basel). 2020;12:294.
Palard X, Edeline J, Rolland Y, Le Sourd S, Pracht M, Laffont S, et al. Dosimetric parameters predicting contralateral liver hypertrophy after unilobar radioembolization of hepatocellular carcinoma. Eur J Nucl Med Mol Imaging. 2018;45:392–401.
Acknowledgements
We thank all staffs in the departments of Nuclear Medicine and Interventional Radiology for their hard work in radioembolization procedures.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by Aslihan Yildirim, Nazim Coskun, and Alptug Ozer Yuksel. The first draft of the manuscript was written by Nazim Coskun and all authors commented on the previous versions of the manuscript. The study was supervised by Elif Ozdemir and Murat Canyigit. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
The study was approved by the institutional review board of Ankara City Hospital (approval no: E2-22-1684), and informed consent was obtained from all individual participants included in the study (or the requirement for written consent was waived by the institutional review board). All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration as revised in 2013 and its later amendments.
Consent for Publication
The participants signed consent regarding publishing their data (and/or photographs).
Competing Interests
Nazim Coskun, Aslihan Yildirim, Alptug Ozer Yuksel, Murat Canyigit, and Elif Ozdemir declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Coskun, N., Yildirim, A., Yuksel, A.O. et al. The Radiation Dose Absorbed by Healthy Parenchyma Is a Predictor for the Rate of Contralateral Hypertrophy After Unilobar Radioembolization of the Right Liver. Nucl Med Mol Imaging 56, 291–298 (2022). https://doi.org/10.1007/s13139-022-00770-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-022-00770-6