Abstract
Purpose
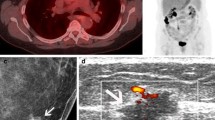
To compare the performance of fluorine-18 fluorodeoxyglucose positron emission tomography and computed tomography (FDG PET/CT) with conventional imaging methods (CIM), including computed tomography (CT), magnetic resonance imaging (MRI), and mammography (MMG) in cancer of unknown primary (CUP).
Methods
A total of 36 patients with CUP, who referred to our clinic for a FDG PET/CT scan, were enrolled in this study. Thirty of the patients were also examined through either diagnostic CT/MRI and/or MMG. The diagnostic performance of both methods for the primary cancer location was analyzed. The results of FDG PET/CT and CIM were compared based on the standard reference of the histopathology and/or clinical and laboratory follow-up.
Results
The primary cancer locations were detected in 24 patients (66.6%, 24/36) by FDG PET/CT, whereas CIM identified the locations in 16 patients (53.3%, 16/30). Sensitivity, specificity, PPV, NPV, and accuracy rates of the detection of the primary tumor localizations were as follows: 83, 70, 89, 58, and 79% for FDG PET/CT; 70, 62, 84, 42, and 68% for CIM, respectively. There was no statistical significance between modalities regarding any of the categories in 30 patients.
Conclusion
FDG PET/CT detected the primary tumors of the patients with CUP more than CIM did. However, the difference between them was not found to be statistically significant. It may be considered that FDG PET/CT scan can be performed as a first-line tool in the initial diagnosis of the patients with CUP and to add radiodiagnostic imaging in selective cases. We conclude that if the first-line examination of a CUP patient has been already performed by a CIM and the result was negative or inconclusive, FDG PET/CT can be considered to avoid unnecessary imaging procedures.

Similar content being viewed by others
References
Pavlidis N, Fizazi K. Carcinoma of unknown primary (CUP). Crit Rev Oncol Hematol. 2009;69:271–8.
Antoch G, Vogt FM, Freudenberg LS, Nazaradeh F, Goehde SC, Barkhauden J, et al. Whole-body dual-modality PET/CT and whole-body MRI for tumor staging in oncology. JAMA. 2003;290:3199–206.
Nam EJ, Yun MJ, Oh YT, Kim JW, Kim JH, Kim S, et al. Diagnosis and staging of primary ovarian cancer: correlation between PET/CT, Doppler US, and CT or MRI. Gynecol Oncol. 2010;116:389–94.
Shim SS, Lee KS, Kim BT, Chung MJ, Lee EJ, Han J, et al. Non-small cell lung cancer: prospective comparison of integrated FDG PET/CT and CT alone for preoperative staging. Radiology. 2005;236:1011–9.
Johansen J, Petersen H, Godballe C, Loft A, Grau C. FDG-PET/CT for detection of the unknown primary head and neck tumor. Q J Nucl Med Mol Imaging. 2011;55:500–8.
National Comprehensive Cancer Network. Occult Primary (Version 1.2018). https://www.nccn.org/professionals/physician_gls/pdf/occult.pdf. Accessed January 15, 2018.
Agrawal A, Rangarajan V. Appropriateness criteria of FDG PET/CT in oncology. Indian J Radiol Imaging. 2015;25:88–101.
Kwee TC, Kwee RM. Combined FDG-PET/CT for the detection of unknown primary tumors: systematic review and meta-analysis. Eur Radiol. 2009;19:731–44.
Fencl P, Belohlavek O, Skopalova M, Jaruskova M, Kantorova I, Simonova K. Prognostic and diagnostic accuracy of [18F] FDG-PET/CT in 190 patients with carcinoma of unknown primary. Eur J Nucl Med Mol Imagıng. 2007;34:1783–92.
Elboga U, Kervancioglu S, Sahin E, Mustafa Basıbuyuk YZC, Aktolun C. Utility of F-18 fluorodeoxyglucose positron emission tomography/computed in carcinoma of unknown primary. Int J Clin Exp Pathol. 2014;7:8941–6.
Han A, Xue J, Hu M, Zheng J, Wang X. Clinical value of F18-FDG PET/CT in detecting primary tumor for patients with carcinoma of unknown primary. Cancer Epidemiol. 2012;36:470–5.
Rusthoven KE, Koshy M, Paulino AC. The role of fluorodeoxyglucose positron emission tomography in cervical lymph node metastases from an unknown primary tumor. Cancer. 2004;101:2641–9.
Pelosi E, Pennone M, Deandreis D, Douroukas A, Mancini M, Bisi G. Role of whole body positron emission tomography/computed tomography scan with 18F-fluorodeoxyglucose in patients with biopsy proven tumor metastases from unknown primary site. Q J Nucl Med Mol Imaging. 2006;50:15–22.
Kwee TC, Basu S, Cheng G, Alavi A. FDG PET/CT in carcinoma of unknown primary. Eur J Nucl Med Mol Imaging. 2010;37:635–44.
Gutzeit A, Antoch G, Kühl H, Egelhof T, Fischer M, Hauth H, et al. Unknown primary tumors: detection with dual-modality PET/CT--initial experience. Radiology. 2005;234:227–34.
Regelink G, Brouwer J, de Bree R, Pruim J, van der Laan BF, Vaalburg W, et al. Detection of unknown primary tumours and distant metastases in patients with cervical metastases: value of FDG-PET versus conventional modalities. Eur J Nucl Med. 2002;29:1024–30.
Lee JR, Kim JS, Roh JL, Lee JH, Baek JH, Cho KJ, et al. Detection of occult primary tumors in patients with cervical metastases of unknown primary tumors: comparison of (18)F FDG PET/CT with contrast-enhanced CT or CT/MR imaging-prospective study. Radiology. 2015;274:764–71.
Moller AK, Loft A, Berthelsen AK, Pedersen KD, Graff J, Christensen CB, et al. A prospective comparison of 18F-FDG PET/CT and CT as diagnostic tools to identify the primary tumor site in patients with extracervical carcinoma of unknown primary site. Oncologist. 2012;17:1146–54.
Ng SH, Chan SC, Yen TC, Chang JT, Liao CT, Ko SF, et al. Staging of untreated nasopharyngeal carcinoma with PET/CT: comparison with conventional imaging work-up. Eur J Nucl Med Mol Imaging. 2009;36:12–22.
Rosen EL, Eubank WB, Mankoff DA. FDG PET, PET/CT, and breast cancer imaging. Radiographics. 2007;27(Suppl 1):215–29.
National Comprehensive Cancer Network. Hepatobiliary Cancers (Version 4.2017). https://www.nccn.org/professionals/physician_gls/pdf/hepatobiliary.pdf. Accessed January 18, 2018.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
Neslihan Cetin Avci, Filiz Hatipoglu, Ahmet Alacacıoglu, Emine Ebru Bayar, and Gonca Gul Bural declare that they have no conflict of interest or no fundings received.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed Consent
The institutional review board of our institute approved this retrospective study, and the requirement to obtain informed consent was waived.
Rights and permissions
About this article
Cite this article
Cetin Avci, N., Hatipoglu, F., Alacacıoglu, A. et al. FDG PET/CT and Conventional Imaging Methods in Cancer of Unknown Primary: an Approach to Overscanning. Nucl Med Mol Imaging 52, 438–444 (2018). https://doi.org/10.1007/s13139-018-0544-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13139-018-0544-7