Abstract
Background
Excimer laser is used to treat coronary artery disease, especially in case of lesions with thrombus and in-stent restenosis (ISR). However, there are no in vivo preclinical studies that have evaluated the pathological reactions of the vessel wall after excimer laser ablation.
Methods
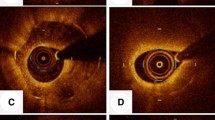
Bare-metal stents were placed in the external iliac arteries of six healthy rabbits. Twenty-eight days later, excimer laser ablation was performed with low-power (45 (fluency)/25 (rate)) in one side, and high-power (60/40) in the opposite side, followed by optical coherence tomography (OCT) evaluation. Rabbits were sacrificed 15 min after the procedure, and histological assessment was performed.
Results
Morphometry analysis of OCT showed similar stent and lumen size between low-power and high-power group. Histological evaluation suggested endothelial cell loss, fibrin deposition, and tissue loss. The low-power group showed significantly less pathological changes compared with the high-power group: angle of endothelial cell loss, 32.4° vs. 191.7° (interquartile range, 8.8°–131.7° vs. 125.7°–279.5°; p < 0.01); fibrin deposition, 1.1° vs. 59.6° (0.0°–70.4° vs. 31.4°–178.4°; p = 0.03); and tissue loss 0.0° vs. 18.2° (0.0°–8.7° vs. 0.0°–42.7°; p = 0.03).
Conclusions
The pathological changes in neointima were more prominent after high-power excimer laser ablation than after low-power excimer laser. To improve safety in clinical practice, understanding the pathological changes of tissues after excimer laser in lesions with ISR is essential.





Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, [ST], upon reasonable request.
References
Cook SL, Eigler NL, Shefer A, Goldenberg T, Forrester JS, Litvack F. Percutaneous excimer laser coronary angioplasty of lesions not ideal for balloon angioplasty. Circulation. 1991;84:632–43.
Rawlins J, Din JN, Talwar S, O’Kane P. Coronary intervention with the excimer laser: review of the technology and outcome data. Interv Cardiol. 2016;11:27–32.
Tsutsui RS, Sammour Y, Kalra A, et al. Excimer laser atherectomy in percutaneous coronary intervention: a contemporary review. Cardiovasc Revasc Med. 2021;25:75–85.
Dahm JB, Topaz O, Woenckhaus C, et al. Laser-facilitated thrombectomy: a new therapeutic option for treatment of thrombus-laden coronary lesions. Catheter Cardiovasc Interv. 2002;56:365–72.
Topaz O, Bernardo NL, Shah R, et al. Effectiveness of excimer laser coronary angioplasty in acute myocardial infarction or in unstable angina pectoris. Am J Cardiol. 2001;87:849–55.
Baumbach A, Bittl JA, Fleck E, et al. Acute complications of excimer laser coronary angioplasty: a detailed analysis of multicenter results. Coinvestigators of the U.S. and European Percutaneous Excimer Laser Coronary Angioplasty (PELCA) Registries. J Am Coll Cardiol. 1994;23:1305–13. https://pubmed.ncbi.nlm.nih.gov/8176087/.
Sintek M, Coverstone E, Bach R, et al. Excimer laser coronary angioplasty in coronary lesions: use and safety from the NCDR/CATH PCI registry. Circ Cardiovasc Interv. 2021;14:e010061.
Nakazawa G, Torii S, Ijichi T et al. Comparison of vascular responses following new-generation biodegradable and durable polymer-based drug-eluting stent implantation in an atherosclerotic rabbit iliac artery model. J Ame Heart Assoc 2016;5.
Fujihara M, Kurata N, Yazu Y, et al. Clinical expert consensus document on standards for lower extremity artery disease of imaging modality from the Japan Endovascular Treatment Conference. Cardiovasc Interv Ther. 2022;37:597–612.
Fujii K, Kubo T, Otake H, et al. Expert consensus statement for quantitative measurement and morphological assessment of optical coherence tomography: update 2022. Cardiovasc Interv Ther. 2022;37:248–54.
Torii S, Nakazawa G, Ijichi T, Yoshikawa A, Ohno Y, Ikari Y. Comparison of the endothelial coverage in everolimus and zotarolimus-eluting stents in normal, atherosclerotic, and bifurcation rabbit iliac arteries. Cardiovasc Interv Ther. 2018;33:55–61.
Torii S, Yahagi K, Mori H, et al. Biologic drug effect and particulate embolization of drug-eluting stents versus drug-coated balloons in healthy swine femoropopliteal arteries. J Vasc Interv Radiol. 2018;29:1041-1049.e3.
Torii S, Yahagi K, Mori H, et al. Safety of zilver PTX drug-eluting stent implantation following drug-coated balloon dilation in a healthy swine model. J Endovasc Ther. 2018;25:118–26.
Torii S, Jinnouchi H, Sakamoto A, et al. Drug-eluting coronary stents: insights from preclinical and pathology studies. Nat Rev Cardiol. 2020;17:37–51.
Giacoppo D, Alfonso F, Xu B, et al. Drug-coated balloon angioplasty versus drug-eluting stent implantation in patients with coronary stent restenosis. J Am Coll Cardiol. 2020;75:2664–78.
Topaz O, Ebersole D, Das T, et al. Excimer laser angioplasty in acute myocardial infarction (the CARMEL multicenter trial). Am J Cardiol. 2004;93:694–701.
Nishino M, Mori N, Takiuchi S, et al. Indications and outcomes of excimer laser coronary atherectomy: efficacy and safety for thrombotic lesions—the ULTRAMAN registry. J Cardiol. 2017;69:314–9.
Acknowledgements
We thank Ayako Yoshikawa (CV-Hills, Tokai University) and Shunji Amano (the Support Center for Medical Research and Education, Tokai University) for their valuable technical assistance.
Funding
This study is sponsored by Philips (Amsterdam, Netherlands). Sho Torii received research grants from Abbot Vascular Japan, Boston Scientific Japan, Medtronic, Philips Japan, and received honoraria from Philips Japan. Gaku Nakazawa is a consultant for Boston Scientific, Abbott Vascular, Terumo Corp., and Japan Medical Device Technology Co., Ltd, and received research grants from Boston Scientific, Abbott Vascular, Terumo Corp., and Japan Medical Device Technology Co., Ltd. Yuji Ikari received honoraria from Philips Japan.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nagamatsu, H., Torii, S., Aihara, K. et al. Histological evaluation of vascular changes after excimer laser angioplasty for neointimal formation after bare-metal stent implantation in rabbit iliac arteries. Cardiovasc Interv and Ther 38, 223–230 (2023). https://doi.org/10.1007/s12928-022-00905-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12928-022-00905-8