Abstract
Objectives
Mindfulness is a multifaceted concept which might be best captured by person-centered profiles rather than by variable-centered assessment of its subcomponents. Patients with different mindfulness profiles may vary in mental health status and might experience differential clinical outcomes of Mindfulness-Based Cognitive Therapy (MBCT). We therefore aimed to assess the relationship between mindfulness profiles and mental health in patients with major depressive disorder (MDD) and to examine whether mindfulness profiles are predictive for MBCT-induced changes in mental health.
Method
Latent profile analysis (LPA), a method used to identify hidden subgroups of individuals within a population, was performed on pre-MBCT subscale scores of the Five Facet Mindfulness Questionnaire in patients with current or remitted MDD (n=754). Equality of means of pre-MBCT, post-MBCT, and residualized change scores of several mental health measures across the latent profiles was tested.
Results
LPA identified four distinct mindfulness profiles. Three profiles were similar to previously identified profiles in another MDD sample (“very low mindfulness,” “high mindfulness,” “non-judgmentally aware”) and one profile was similar to that identified in non-clinical populations (“judgmentally observing”). The “high mindfulness” subgroup scored best, the “very low mindfulness” worst, and the other subgroups intermediate on mental health in terms of depressive symptoms, worry, overall functional impairment, and self-compassion. Mindfulness profiles were not predictive of MBCT-induced changes in mental health.
Conclusions
Mindfulness profiles were differentially related to mental health, but were not predictive of treatment outcome. Future research would benefit from longitudinal assessment of latent mindfulness profiles to examine whether a patient’s profile changes after MBCT and whether hypothesized change in profile would be related to treatment outcome.
Preregistration
This study was not preregistered.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Mindfulness has been described as the awareness that arises through paying attention in the present moment, on purpose, in an open, accepting, and non-judgmental way (Kabat-Zinn, 2009). To better understand the construct of mindfulness and its relation to mental health, it is important to be able to adequately measure trait mindfulness.
One of the most widely used questionnaires to measure trait mindfulness is the Five Facet Mindfulness Questionnaire (FFMQ) consisting of 5 subscales: observing, describing, acting with awareness, non-judging of inner experience, and non-reactivity to inner experience (Baer et al., 2006; Baer et al., 2008). However, the observing subscale loads negatively on an overall latent construct of mindfulness (Baer et al., 2006; Pearson et al., 2015) and expected relations between the observing subscale with measures of mental health are inconsistent for populations with and without meditation experience (Baer et al., 2006; Baer et al., 2008; Brown et al., 2015; Fernandez et al., 2010; Gu et al., 2016).
Given the inconsistent findings regarding the observing subscale in different samples and the multi-faceted nature of trait mindfulness, it seems conceptually more appropriate to focus on the individual facets of the FFMQ rather than the total score. Moreover, it is also important to consider the relationship between the individual facets and the extent to which they interact with each other to contribute to mental health. This can be achieved by either examining the predictive value of the individual FFMQ subscales and their interactions in relation to external indicators of mental health within a given population (variable-centered), or by the identification of person-centered mindfulness profiles. By identifying (unobserved) subgroups of people based on their similarities (response profiles) on a set of variables (e.g., mindfulness subscales), one could examine how those subgroups relate to measures of mental health. Such a person-centered approach allows for a more fine-grained evaluation of the relationship between mindfulness facets and how they together interact and relate to mental health, and may therefore be a good addition to the traditionally used variable-centered methods (Howard & Hoffman, 2018).
Latent profile analysis (LPA) is such a person-centered statistical method that aims to identify latent subgroups based on a certain set of variables, such as scores on the FFMQ subscales. Pearson et al. (2015) were the first to identify subgroups based on individuals’ response profiles on mindfulness facets of the FFMQ in college students. They identified four subgroups: a “high mindfulness,” “low mindfulness”, “judgmentally observing,” and “non-judgmentally aware” subgroup. The subgroups “low mindfulness” and “high mindfulness” were characterized by relatively low and high scores on the FFMQ subscales respectively. “Judgmentally observing” was characterized by very low scores on non-judging and acting with awareness, and relatively high on observing, whereas “non-judgmentally aware” was characterized by relatively low scores on observing and high scores on non-judging and acting with awareness. Subsequently, the same four subgroups were identified in a sample of college students with and without meditation experience (Bravo et al., 2016), young adults in romantic relationships (Kimmes et al., 2017), another college student sample (Bravo et al., 2018), and adults (Ford et al., 2020; Sahdra et al., 2017; Zhu et al., 2020). In addition, three similar subgroups were found in a military sample (combined “low mindfulness” and “judgmentally observing” (Bravo et al., 2018)), adolescents (moderate mindfulness instead of “high” and “low mindfulness” (Calvete et al., 2020)) and college students (absence of “low mindfulness” (Bronchain et al., 2021)). The subgroups were remarkably similar in those studies, in which the “high mindfulness” and “non-judgmentally aware” subgroups were associated with better mental health, i.e., better cross-sectional scores on several symptom domains (depressive and anxiety symptoms, worry, rumination, affective lability, and distress intolerance) and psychological well-being outcomes. Some studies in non-clinical samples found slightly different mindfulness profiles showing overlap but also some distinctions in profile structure and associations with other measures (De Souza Marcovski & Miller, 2022; Gómez-Odriozola & Calvete, 2021; Lecuona et al., 2022; Stanmyre et al., 2022; Zhang et al., 2019).
As a result of these studies in non-clinical samples, Gu et al. (2020) investigated whether these same four latent profiles would also be observed in people with a history of depression, and whether the “low mindfulness,” and “judgmentally observing” profiles would be associated (cross-sectionally) with poorer mental health. Gu et al. (2020) performed LPA on two subsamples of adults with a history of recurrent depression (≥ 3 episodes) in full or partial remission who participated in one of two RCTs that examined the effectiveness of Mindfulness-Based Cognitive Therapy (MBCT) at reducing relapse (Kuyken et al., 2015; Williams et al., 2014). In both the test (n = 343) and validation sample (n = 340), they identified a 4-profile solution of which 2 profiles mapped broadly on the “high mindfulness” and “non-judgmentally aware” profiles previously identified in non-clinical samples (Gu et al., 2020). In addition, they found a “moderate mindfulness” and “very low mindfulness” profile. The majority of this clinical population was classified into the “very low mindfulness” (23.0%) or the “moderate mindfulness” (58.1%) subgroup. Those classified into the “high mindfulness” (12.2%) and “non-judgmentally aware” (6.7%) subgroups had lower levels of depressive symptoms and higher levels of self-compassion (Gu et al., 2020).
To our best knowledge, no study to date assessed the predictive value of mindfulness profiles for mindfulness-based interventions (MBIs) such as MBCT. MBCT is an evidence-based treatment for major depressive disorder (MDD) that combines elements of cognitive behavioral therapy and meditative practices and is both effective in reducing relapse rates (Kuyken et al., 2016) and (residual) depressive symptoms (Goldberg et al., 2019). Based on a compensation model (Cheavens et al., 2012), it could be argued that in particular individuals with lower levels of mindfulness skills at baseline will profit from MBIs such as MBCT because an existent deficiency is targeted. Based on a capitalization model, on the other hand, it could be argued that in particular individuals with higher baseline levels of mindfulness skills will profit because more mindful people may find the mindfulness practice easier or more comfortable, and may persist longer at practicing (Shapiro et al., 2011). Studies using variable-centered methods to investigate whether baseline levels of mindfulness skills are predictive for or moderate MBI-induced treatment response are scarce and showed inconsistent results: While some studies found baseline (facets of) mindfulness to significantly predict (Gawrysiak et al., 2018) or moderate (Kuyken et al., 2016; Nyklíček et al., 2016) MBI-treatment effects, others did not find significant moderation effects (Cladder-Micus et al., 2018; Greeson et al., 2015; Van Aalderen et al., 2012). Thus, more research into the predictive value of mindfulness skills before an MBI, preferably by assessing the individual facets of mindfulness separately, instead of a total score, is required. Moreover, to our best knowledge, no studies to date assessed whether a person-centered approach would reveal differential relationships between mindfulness profiles and treatment outcome.
The current study has two main objectives. First, we aimed to assess whether we can replicate the 4-profile solution found by Gu et al. (2020) in a large naturalistic cohort of patients with past or present MDD. As part of the replication, we aim to validate those profiles by assessing the associations of the most optimal profile solution in this sample with a broader range of mental health measures: depressive symptoms (BDI-II), worry (PSWQ), overall functional impairment (OQ-45), and self-compassion (SCS). We define the combination of those measures as indicators of “mental health” rather than “psychological functioning” (as defined by Gu et al., 2020) because mental health encompasses emotional, psychological, and social well-being and therefore this term is more appropriate in the present study. Second, we aim to assess whether profile membership at baseline is predictive of treatment outcomes following MBCT. Because we are not aware of any existing prior information on the predictive value of mindfulness profiles, we aim to provide a most comprehensive picture of the prospective value of those profiles and therefore include depressive symptoms (BDI-II) as primary outcome and the other measures (PSWQ, OQ-45, SCS) as secondary outcomes.
Method
Participants
The sample consisted of a naturalistic uncontrolled cohort of patients with past or present MDD who received MBCT at the Radboud University Medical Centre for Mindfulness in Nijmegen, the Netherlands, between July 2012 and April 2018. Demographic and clinical variables were derived from the electronic patient health records. Those patients with at least one episode of MDD were selected for the latent profile analysis. The current sample thus consisted of patients with different recurrence (recurrent versus single) and remission (current versus remitted) status of MDD; see Table 1.
Procedure
Patients were referred to the center for mindfulness by their general practitioner or attending psychologist or psychiatrist. All referred patients were clinically assessed before taking part in the MBCT by means of a semi-structured psychiatric interview (see measures). The multi-disciplinary team consisting of the attending psychiatrist, psychologists, and mindfulness trainers evaluated whether MBCT was suitable or whether other evidence-based treatments were preferable for the patient. This was usually the case if patients met one or more of the following criteria: current substance dependency, acute suicidality, acute psychotic symptoms. In addition, motivation and practical barriers for participation in the MBCT were discussed. Patients were offered MBCT if they were willing to participate in a group setting, adhere to homework assignments, and able to attend at least six out of eight sessions and the silent day. Before the start of the MBCT and after the final session of the MBCT, patients were asked to complete a set of self-report questionnaires (see measures) as part of routine outcome monitoring (ROM). All patients who completed the baseline questionnaires were included in the current study. This same dataset (n = 765) was previously used in a study investigating the effectiveness of MBCT for MDD in routine clinical practice (Geurts et al., 2020). In the current study, patients who had missing data on all subscales of the FFMQ at baseline were excluded from analyses (n = 11), resulting in 754 patients for the LPA. All procedures were in accordance with the 1964 Helsinki Declaration and later amendments. The medical ethical committee waived the need for approval (CMO dossier: 2020–7226) per the Dutch Medical Research Involving Human Subjects Act, since participants were not subject to additional procedures or required to follow rules of behavior.
MBCT was provided in accordance with the original protocol (Segal et al., 2002) and consisted of eight weekly sessions of 2.5 hr, a 6-hr silent day in between Sessions 6 and 7, and daily home practice (30–45 min). The MBCT sessions were given in groups of 8–12 participants and consisted of psychoeducation and meditation exercises as well as dialogue and inquiry about those exercises. MBCT was taught by teachers meeting the advanced criteria of the Association of Mindfulness-Based Teachers in the Netherlands and Flanders, which are in concordance with the Good Practice guidelines of the UK Network of Mindfulness-Based Teacher Trainers (Crane et al., 2012).
Measures
Demographic and Clinical Variables
The Mini International Neuropsychiatric Interview Plus (MINI-Plus; Sheehan et al., 1998) was used to determine psychiatric disorders. The MINI-Plus is a semi-structured psychiatric diagnostic interview developed to assess patients for psychiatric diagnosis according to DSM-IV-TR criteria and has good psychometric properties. It was conducted by trained psychiatrists (in training) or psychologists. Apart from MDD, several other comorbid psychiatric disorders were assessed, e.g., dysthymia, bipolar, anxiety, somatization, ADHD, addiction, and eating disorders (Geurts et al., 2021). Personality disorders and autism spectrum disorders were classified, either when diagnosed in the patient history and the psychiatric review was in accordance with these classifications or when suspected, additional diagnostic interviews were conducted, i.e., the structured clinical interview for DSM-IV personality disorders (SCID-II, First et al., 1997) and the Dutch Interview for diagnosing autism spectrum disorders (NIDA, Vuijk, 2016), respectively.
Five Facet Mindfulness Questionnaire-Short Form
Mindfulness skills were measured with the Dutch version of the Five Facet Mindfulness Questionnaire-Short Form (FFMQ-SF; Bohlmeijer et al., 2011). This questionnaire consists of 24 items that measure levels of mindfulness on a 5-point Likert scale across the five facets “observing,” “describing,” “acting with awareness,” “non-judgment of inner experience,” and “non-reactivity to inner experience” (Baer et al., 2006). The facets’ scores were calculated by determining the mean of corresponding item scores, which is in accordance with relevant previous literature (Bravo et al., 2016; Bravo et al., 2018; Gu et al., 2020; Pearson et al., 2015). Negatively phrased items were reversed scored before computing the mean scores of the facets. Cronbach’s alpha/McDonald’s omega for the individual facets were 0.78/0.78 (observing), 0.87/0.88 (describing), 0.83/0.84 (acting with awareness), 0.78/0.78 (non-judgment of inner experience), and 0.76/0.77 (non-reactivity of inner experience).
Beck Depression Inventory-Second edition
Severity of depressive symptoms was assessed with the Beck Depression Inventory (BDI-II: Beck et al., 1996, Dutch version: Van der Does, 2002). The questionnaire contains 21 items which are scored on a 4-point Likert scale ranging from 0 to 3. Total scores of 0–13 indicate minimal, 14–19 mild, 20–28 moderate, and 29–63 severe depression. Individual items were summed to calculate a total score. Cronbach’s alpha/McDonald’s omega in the current sample was 0.91/0.91.
Penn State Worry Questionnaire
The Penn State Worry Questionnaire (PSWQ) contains 16 items and was used to assess worry propensity on a 5-point Likert scale ranging from 1 to 5 (Meyer et al., 1990, Dutch version: van Rijsoort et al., 1999). Cronbach’s alpha/McDonald’s omega in the current sample was 0.92/0.92. Total scores of 16–28 indicate very low, 29–38 low, 39–48 average, 49–59 high, and 59–80 very high (clinical range) level of worrying (van der Heiden et al., 2009).
Outcome Questionnaire-45
The Outcome Questionnaire-45 (OQ45; Lambert et al., 1996) is a measure of psychological and general functioning consisting of 45 items which are scored on a 5-point Likert scale (0–4). The total score of the Dutch OQ-45 (ranging from 0 to 180) was used as a measure of overall functional impairment (de Jong & Spinhoven, 2008). Higher scores indicate poorer overall functioning. For the Dutch OQ45, the normative (cutoff) score is 55, meaning that a person scoring ≥ 55 belongs to the dysfunctional (clinical) range (de Jong & Spinhoven, 2008). Cronbach’s alpha/McDonald’s omega in the current sample was 0.92/0.92.
Self-Compassion Scale
The Self-Compassion Scale (SCS) is a measure of self-compassion, consisting of six subscales: self-kindness, self-judgment, common humanity, isolation, mindfulness, and overidentification (Neff, 2003). The Dutch version of the SCS was used, which is highly similar to the original but uses a 7-point response scale (instead of 5) and includes only 24 instead of 26 items (Neff & Vonk, 2009). Subscale scores were computed by calculating the mean of the relevant item scores (range 0–7). The total score was calculated by summing the subscale (mean) scores. There are no clinical norms or scores which indicate that an individual is high or low in self-compassion. Negatively phrased items were reverse-scored prior to calculation of the subscales and total score. Cronbach’s alpha/McDonald’s omega for the total score was 0.91/0.92, and for the individual subscales 0.76/0.76 (self-kindness), 0.81/0.82 (self-judgment), 0.68/0.68 (common humanity), 0.79/0.79 (isolation), 0.76/0.76 (mindfulness), and 0.71/0.71 (overidentification).
Data Analyses
Data curation and visualization was carried out in the open-source statistical software program R (RStudio 2019). Differences in baseline demographic and clinical characteristics of patients with a full dataset and patients with missing data post-MBCT were tested with χ2 or ANOVA statistics whereas pre- to post-changes in outcome measures and FFMQ subscales for patients with a full data set were tested with paired samples t-tests. Within-group Cohen’s d effect sizes were calculated by dividing the pre- to post-MBCT mean difference in outcomes by the standard deviation of the differences.
Confirmatory factor analyses (CFAs) were run on the FFMQ-SF at baseline and post-MBCT to confirm whether the FFMQ-SF in the current sample can be reduced to five facets at both time points. In line with the original validation studies of the 39-item FFMQ (Baer et al., 2006; Baer et al., 2008) and the validation study of the 24-item FFMQ-SF in a Dutch depression sample (Bohlmeijer et al., 2011), a single-factor model, correlated 5-factor model, and a second-order hierarchical model were tested in Mplus. Following Bohlmeijer et al. (2011), in those models, items were constrained to load on 1 factor only, error terms were not allowed to correlate, and the variances of the factors were fixed to 1. The root mean square error of approximation (RMSEA), comparative fit index (CFI), Tucker-Lewis Index, and standardized root mean square residual (SRMR) were used to evaluate absolute model fit. The following values were considered to represent adequate or good fit, respectively, RMSEA/SRMR ≤ 0.08 and ≤ 0.06 and CFI/TLI ≥ 0.90 and 0.95 (Browne & Cudeck, 1992; Hu & Bentler, 1999). The Akaike information criterion (AIC) and Bayesian information criterion (BIC) were used as measures of comparative fit. A smaller AIC or BIC indicates a better model fit. The results regarding the factor structure of the FFMQ-SF in the current sample are reported in the supplementary material (see Supplementary Material and Supplementary Table S1-S2).
Latent profile analyses (LPAs), a statistical approach to uncover latent subgroups within a population based on a set of indicator variables, were conducted in Mplus version 8.6 (Muthén & Muthén, 1998). Mplus code for the performed analyses can be found in the supplementary material. Maximum likelihood estimation with robust standard errors (MLR) were used to fit latent profile models from one up to eight latent profiles to the data. To determine the optimal number of profiles based on the 5 FFMQ-subscales, we followed Nylund et al. (2007) and Tein et al. (2013) and used the BIC, sample-size adjusted BIC (SABIC), and bootstrap likelihood ratio test (BLRT) as superior indicators of the correct number of latent profiles (Nylund et al., 2007; Tein et al., 2013). A smaller BIC or SABIC value indicates a better model fit. The BLRT is used to determine whether a k profile model fits the data significantly better compared to a k-1 profile model. In addition to the BIC and BLRT, we inspected and compared the average latent profile probabilities for the most likely latent profile membership by latent profile (posterior classification probabilities) for competing models. Posterior classification probabilities with higher diagonal values would indicate greater certainty of assignment to the right profile. Because model selection is not always straightforward, we followed recommendations of other researchers to also include profile size (profiles with <1% of total sample or <25 individuals should not be considered meaningful and should be rejected) and previous research and theory upon deciding on the number of profiles (Lubke & Neale, 2006; Spurk et al., 2020). As suggested by Weller et al. (2020), we additionally report the Entropy as a statistic that indicates how accurately the model defines the classes, but do not rely on the value to determine the number of profiles. There is no agreed cutoff criterion for entropy, but higher entropy values indicate a more accurate model. To be consistent with previous studies (Bravo et al., 2016; Bravo et al., 2018; Gu et al., 2020; Pearson et al., 2015), FFMQ subscale means were standardized in order to facilitate labeling and comparison between profiles. In addition, we chose to run LPA’s with both standardized scores and unstandardized scores, and report and visualize those accordingly. By visualizing the same profiles with standardized and unstandardized scores, interpretation and labeling of the profiles may (slightly) differ. We used both standardized and unstandardized scores to determine correct labels for the profiles. The reported final profile counts (n) are based on the estimated model.
The auxiliary variable function in Mplus was used to determine the relationship between the identified profiles and mental health measures at baseline. This function makes use of the Bakk and Vermunt “BCH” approach (Bakk & Vermunt, 2016) that uses a Wald chi-square test to test the equality of the means of the mental health measures across the latent profiles. This function allows to examine the relationship between profiles and mental health measures without directly including those variables in the model. The BCH methods take into account the classification errors of the assigned profile membership and use weights reflecting this measurement error of the latent class variable. The BCH method is the most robust and recommended method for this type of analysis (Bakk & Vermunt, 2016). To investigate whether mindfulness profiles at baseline are also related to post-treatment levels of mental health (uncorrected for baseline) and MBCT-induced changes in mental health, we used the same auxiliary variable function in Mplus to test the equality of the means of post-treatment and residualized change scores of mental health measures across the latent profiles.
Robustness of results was assessed by a sensitivity analysis in which the means of mental health measures were estimated across the latent profiles in 10 datasets for which missing values were imputed. Mplus’ multiple imputation procedure with the Markov Chain Monte Carlo (MCMC) method and Bayesian estimation was used to impute missing values in indicators and mental health measures at baseline and post-treatment, and residualized change scores were recalculated. Ten datasets were deemed sufficient as 5–20 imputations are recommended under moderate missingness and in our dataset only five participants had missing data on indicators and about a 0.3 fraction of the data was missing at post-treatment (Van Buuren, 2018). During the imputation process, (demographic) variables that may be related to the missingness were included in the model for a more accurate imputation of missing values (i.e., work status, educational level, number of MBCT sessions attended, comorbid disorders, age at start study). Because the type = IMPUTATION feature in Mplus does not allow for the automatic BCH method, the manual BCH method was used to estimate the means of baseline, post-MBCT, and residualized change scores across the profiles.
Results
Study population
From the 754 patients who completed the ROM at baseline, a post-MBCT measurement was available for 500 patients (Table 1). Patients without a post-MBCT measurement were slightly younger, had more comorbid developmental and personality disorders, and attended less MBCT sessions than patients with a full data set. In addition, they reported slightly lower levels of worry and slightly higher levels of some of the subscales of both the FFMQ and SCS at baseline (Table 1). Those with a post-MBCT measurement improved on all outcomes from pre- to post-MBCT (Table 1); also see Geurts et al. (2020).
Latent profile analyses
The BIC, BLRT, and entropy for the latent profile models containing 2 to 8 profiles are presented in Table 2. The BIC value is lowest for the 4-profile-solution while the SABIC is lowest for the 7-profile solution. The BLRT is significant up to the 7-profile solution. In addition, the posterior classification probabilities (Supplementary Table S3) were highest in the 4-profile solution (4-profile; ≥ 0.71, 5-profile; ≥ 0.68, 6-profile; ≥ 0.65). Thus, based upon the BIC and posterior classification probabilities, a model consisting of 4 latent profiles fits the data best, whereas based on the SABIC and BLRT, a 7-profile solution would fit best. However, the 7-profile solution contains one profile with only 14 patients, which is considerably lower than the minimum of 25 as proposed by Lubke and Neale (2006) and was therefore rejected. In addition, when visually inspecting the 5-profile and 6-profile solution, it could be concluded that no “new” distinguished profile emerged (when compared to the other 4 profiles). Thus, when taking into account the profile solution found by Gu et al. (2020), other previous studies in non-clinical samples (Bravo et al., 2016; Bravo et al., 2018; Calvete et al., 2020; Ford et al., 2020; Kimmes et al., 2017; Lecuona et al., 2022; Pearson et al., 2015; Sahdra et al., 2017; Stanmyre et al., 2022; Zhang et al., 2019) and our fit indices, we settled for the 4-profile solution.
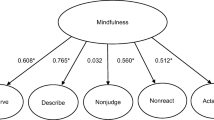
Standardized and unstandardized mean scores on the mindfulness subscales across the latent profiles based on the estimated four-profile model are presented in Table 3 and visualized in Fig. 1. Profile 1 contains 13.3% of the sample (n = 100) and had relatively high standardized mean scores on the “non-judging” subscale (z = 0.88 and low scores on the “observing” subscale (z = −0.97), which is comparable to both test and validation sample of the “non-judgmentally aware” subgroup identified by Gu et al. (2020). In addition, standardized scores on the “acting with awareness” subscale were slightly above the mean (z = 0.013), which is comparable to the validation sample in Gu et al. (2020). Therefore, Profile 1 was labeled as “non-judgmentally aware.” Profile 2 contains 24.4% of the sample (n = 184) and was labeled “very low mindfulness” because patients had relatively low standardized scores on all FFMQ subscales (all z-scores ranging from −0.50 to −0.93), comparable to those reported by Gu et al. (2020). Profile 3 contains the majority of the sample (48.5%, n = 366) and was most difficult to label. When examining the standardized scores, it can be appreciated that on all subscales standardized scores of patients are close to the mean (z-scores between −0.24 and 0.43), with the highest mean score for “observing” and the lowest mean score for “non-judging.” In addition, Fig. 1 B shows that patients in Profile 3 have high unstandardized scores on the “observing” (3.76) and “describing” (3.48) subscale and low scores on “non-reactivity” (2.52) and “non-judging” (2.63). This profile structure comes closest to the “judgmentally observing” profile previously described in extant literature (Bravo et al., 2016; Bravo et al., 2018; Kimmes et al., 2017; Pearson et al., 2015), and we therefore decided to label Profile 3 as such. Profile 4 contains 13.8% of the sample (n = 104). We labeled this profile “high mindfulness” because patients had relatively high standardized scores on all FFMQ subscales (z-scores ranging from 0.49 to 1.22).
Relation between mindfulness profiles and baseline measures of mental health
Mean scores for depressive symptoms (BDI-II), worry (PSWQ), overall functional impairment (OQ-45), and (subscales of) self-compassion (SCS) across the different profiles were evaluated and compared with one another. Profile-specific unstandardized means for the mental health measures are presented in Table 4. A significant overall chi-square test indicates that the means of the four profiles were significantly different for that mental health measure (Table 4). Subsequently, pair-wise comparisons were made to compare the individual profiles with one another. Chi-square test-statistics for pairwise comparison between profiles are presented in Supplementary Table S4.
The “very low mindfulness” profile had higher scores for depressive symptoms (BDI-II) compared to all other profiles, whereas the “high mindfulness” profile had lower scores compared to all other profiles. Depressive symptoms in the “non-judgmentally aware” and “judgmentally observing” profiles did not differ from another but were higher compared to the “high mindfulness” profile and lower compared to the “very low mindfulness” profile.
Scores for worry (PSWQ) were different between all profiles, with highest levels in the “very low mindfulness” profile, and gradually diminishing levels in “judgmentally observing,” “non-judgmentally aware,” and “high mindfulness.”
For overall, functional impairment (OQ-45) scores were highest in the “very low mindfulness” profile and lowest in the “high mindfulness” profile and intermediate scores were found for the “non-judgmentally aware” and “judgmentally observing” profiles. This pattern across the different profiles was the same as compared to depressive symptoms.
For self-compassion, the “high mindfulness” profile had higher total scores on the SCS compared to other profiles, whereas the “very low mindfulness” profile had lower scores. The “non-judgmentally aware” and “judgmentally observing” profiles had intermediate scores. A similar pattern emerged for the subscales of the SCS, though per subscale slight differences were found.
Predictive value of mindfulness profiles
First, we assessed whether the mindfulness profiles were predictive for post-treatment levels of the mental health outcomes. Post-treatment scores on the measures of mental health for the different profiles are presented in Table 5, together with the overall chi-square test statistics. Specific pair-wise comparisons between profiles can be found in Supplementary Table S5.
In line with relations found with the pre-treatment measures, post-treatment mean scores for depressive symptoms, worry, and overall functional impairment were lowest in the “high mindfulness” profile and highest in the “very low mindfulness” profile whereas scores for (subscales of) self-compassion were highest in the “high mindfulness” profile and lowest in the “very low mindfulness” profile. More specifically, while all the mental health measures at baseline significantly differed between the “high mindfulness profile” and all other profiles and between the “very low mindfulness” profile and all other profiles (except for “common humanity”), this distinction became a little bit less pronounced for post-treatment scores. These results show that mindfulness profiles at baseline are related to severity of depression and secondary outcomes measured before MBCT, but also after participation in MBCT.
However, this does not answer the question whether the rate of improvement is comparable over the profiles after accounting for the effect of baseline severity of the dependent variables. Therefore, the means of residualized change scores for depressive symptoms (BDI-II), worry (PSWQ), overall functional impairment (OQ-45), and (subscales of) self-compassion (SCS) were evaluated across the different profiles (Table 6). The overall chi-square tests were non-significant for both the depressive symptoms and all other measures. This suggests that based on the Wald chi-square test, the profiles do not differ in relation to treatment response in terms of residualized change scores on those outcomes. Because those analyses are explorative in nature, we chose to report the chi-square test statistics for pair-wise comparisons between the different profiles in Supplementary Table S6.
Sensitivity analyses: LPAs in imputed datasets
Out of 754 participants, only 5 had one or more missing indicator variables (FFMQ subscales) in the original dataset. As a result, the fit criteria for latent profile analyses containing 2 to 8 profiles, which were based on the 10 imputed datasets (Supplementary Table S7), were very similar to those reported in Table 2. In addition, mean scores of mindfulness facets across the latent profiles were very much alike (Table 3, Supplementary Table S8).
The (average) means of baseline, post-treatment, and residualized change scores of mental health measures across the profiles were very similar within the 10 imputed datasets compared to the original dataset that contained missing values at those distal outcomes (Tables 4–6, Supplementary Table S9-S11). In other words, when considering those 10 imputed datasets, profile membership was (still) related to baseline and post-treatment measures of mental health and not related to residualized change in those measures. Moreover, when examining the pair-wise comparisons, results were almost identical (Tables 4–6, Supplementary Table S9-S11).
Discussion
The current study aimed to replicate and extend the latent profile analysis previously performed by Gu et al. (2020) in a clinical sample with a history of recurrent depression based on the response profiles on the FFMQ subscales. Gu et al. (2020) identified four subgroups: a “high mindfulness,” “non-judgmentally aware,” “moderate mindfulness,” and “very low mindfulness” subgroup. We replicated three of those profiles, the “high mindfulness” (13.8%), “very low mindfulness” (24.4%), and the “non-judgmentally aware” (13.3%) profile. We additionally identified a profile which we labeled “judgmentally observing” (48.5%) because it is structurally similar to that profile previously identified in non-clinical samples (Bravo et al., 2016; Bravo et al., 2018; Bronchain et al., 2021; Calvete et al., 2020; Ford et al., 2020; Pearson et al., 2015; Sahdra et al., 2017). Furthermore, we evaluated the association between the identified profiles and a variety of mental health measures which indicates that the “high mindfulness” profile scored best and the “very low mindfulness” profile scored worst on mental health in terms of depressive symptoms, worry, overall functional impairment, and self-compassion. This is in accordance with previously reported findings in people with recurrent depression (Gu et al., 2020). In addition, we explored the predictive value for treatment outcome of these mindfulness profiles. Our results show that baseline mindfulness profiles are related to baseline and post-treatment measures of mental health in a similar fashion. Patients belonging to the “high mindfulness” subgroup have the lowest severity of depression while patients belonging to the “very low mindfulness” subgroup highest, also after MBCT. But, the rate of improvement in terms of residualized change in depressive symptoms and secondary outcomes seems to be equal between all profiles.
We found profiles that were largely similar to the profiles found by Gu et al. (2020). In terms of profile structure and associations with measures of mental health, “high mindfulness” and “very low mindfulness” were almost identical when comparing both studies. The other two profiles we found had relatively moderate scores on all FFMQ subscales and bear structural resemblances with profiles previously described in literature: “non-judgmentally aware” and “judgmentally observing.” In the test sample of Gu et al. (2020) and in most previous studies in non-clinical samples (Bravo et al., 2016; Bravo et al., 2018; Calvete et al., 2020; Kimmes et al., 2017; Pearson et al., 2015; Sahdra et al., 2017), both the “high mindfulness” and “non-judgmentally aware” profile have been shown to score best in terms of mental health. Our “non-judgmentally aware” profile is more similar to the “non-judgmentally aware” profile in the validation sample of Gu et al. (2020). Those profiles have a somewhat lower score on the “acting with awareness” subscale compared to test sample of Gu et al. (2020) and to similar profiles previously identified in non-clinical samples. Being less able to “act with awareness” may have caused patients in our “non-judgmentally aware” profile to score less well in terms of mental health compared to people from “non-judgmentally aware” profiles from previous studies, and more similar to patients from the “judgmentally observing” profile. The “judgmentally observing” profile was the largest profile identified in our sample (48.5%). We settled for “judgmentally observing” because the profile structure was not entirely flat and looks similar to previously reported profiles (highest standardized scores for observing, lowest for non-judgment), though less pronounced. When we compare our “judgmentally observing” profile to the study of Gu et al. (2020), it is most similar to their “moderate mindfulness” profile. They both contain the majority of the sample and score intermediate in terms of mental health. In contrast, the more pronounced “judgmentally observing” profile in non-clinical samples much more resembles the “low mindfulness” profiles in terms of mental health.
The most well-pronounced uneven profile was “non-judgmentally aware” and comprised a bit more than 10% of the sample, which is in accordance with previous findings in patients with a history of depression (Gu et al., 2020). Although the unevenness of our “judgmentally observing” profile is less pronounced, this profile may be of particular interest because those are the patients that seem to be able to describe and observe their experiences quite well but have difficulties in being non-judgmental and non-responsive to those experiences. From our experience, this combination of close observation coupled with critical judgment is frequently encountered in clinical practice and fits well within view of the self-critical personality trait that is linked to depressive symptoms (Werner et al., 2019). Because the “non-judgmentally aware” and “judgmentally observing” profiles have moderate scores on the FFMQ subscales on average but differ considerably in terms of observing and non-judgment, we were interested in whether those subgroups differed in terms of mental health. One may expect from most extant literature (Bravo et al., 2016; Bravo et al., 2018; Kimmes et al., 2017; Pearson et al., 2015) that the “judgmentally observing” subgroup would score worse in terms of measures of depressive symptoms and overall functional impairment compared to the “non-judgmentally aware” subgroup. However, our findings do not support this presupposition, and some other studies also found less clear distinctions between the two profiles in terms of mental health (Ford et al., 2020; Lecuona et al., 2022; Sahdra et al., 2017). Yet in terms of worry and several subscales of the SCS (i.e., self-judgment, isolation, and overidentification), the “judgmentally observing” profile does score worse compared to the “non-judgmentally aware” profile. Of interest, SCS self-judgment scores were indeed lower in the “judgmentally observing” subgroup, which is in line with the hypothesized self-critical attitude of those patients.
Our sample consisted of patients with both current and remitted MDD with one or more (previous) episodes while the sample of Gu et al. consisted of people with recurrent MDD (≥ 3 episodes) in remission. Still, we identified largely similar profiles compared with Gu et al. (2020), which illustrates that the identified four-profile solution is quite robust and that those findings may generalize to a more heterogeneous group of people with MDD. However, although we and Gu et al. (2020) identified nearly the same profiles, we cannot deduce whether those profiles would also be identified in other clinical groups not suffering from MDD. In addition, the slight structural differences between the “judgmentally observing” (our study) versus “moderate mindfulness” (Gu et al., 2020) may have been caused by the differences between the study samples, e.g., depression status, or differences in demographic variables. Until now, only two other studies aimed to identify mindfulness profiles in other clinical samples: four almost identical profiles (“high mindfulness,” “low or average mindfulness,” “judgmentally observing,” and “non-judgmentally aware” were identified in cancer patients with similar relationships with mental health variables (Lam et al., 2018; Wang et al., 2022). Future research should examine whether those 4 profiles are indeed more generalizable to other (clinical) samples and whether those findings are replicated in demographically different (e.g., in terms of education or culture) MDD populations.
Previously, we showed in the same study population that MBCT was effective in reducing depressive symptoms and also resulted in improvements in worry, mindfulness skills, and self-compassion (Geurts et al., 2020). Baseline total FFMQ scores did not significantly predict residualized change in depressive symptoms in this study population (Geurts et al., 2020). In the current study, we used the same longitudinal data to assess the predictive value of mindfulness profiles. Because baseline severity of depressive symptoms strongly predicted change in depressive symptoms in the previous study and because reductions in depressive symptoms were related to improvements in mindfulness skills on the group level (Geurts et al., 2020), one may expect that profiles that score worst in terms of baseline depression (i.e., “very low mindfulness”) would be related to better treatment outcome (compensation model). On the other hand, one may also argue that patients that are more mindful before MBCT might be better equipped and more likely to further expand and improve their mindfulness skills (capitalization model). Mindfulness profiles proved to be related to post-treatment scores of the mental health outcomes in a similar pattern as observed for the baseline scores. However, when correcting for baseline severity scores on the dependent variables, profiles before MBCT were not significantly related to improvements in depressive symptoms after MBCT, nor to improvements of any of the secondary outcomes. Thus, each profile seems to improve to an equal extent in terms of both the primary and secondary outcomes. This is in line with the variable-centered prediction in our previous study (Geurts et al., 2020). As these analyses were explorative in nature, more research (replication) is required to further assess the predictive value of mindfulness profiles.
Although we did not find mindfulness profiles at baseline to be predictive of the clinical effects of regular MBCT, this might have been different when therapy would have been specifically tailored to the needs of individuals. In general, it would be an asset to the clinical field when one would find that MBI’s specifically tailored to the needs of individuals would improve effectiveness compared to the currently uniformly administered MBI’s. For example, for the judgmentally observing group, an MBCT that focuses more on non-judgment and self-compassion (i.e., on the skills this group scores relatively low) may result in better clinical outcomes. This might be especially relevant for MDD patients, as our study indicates that about half of those patients belong to the “judgmentally observing” group before treatment. Moreover, if patients would have difficulties in being non-judgmental and less self-critical, even after MBCT, offering a mindfulness-based compassionate living (MBCL) (Van den Brink & Koster, 2015) training directly after the MBCT might help those patients in order to develop exactly those skills and to develop more self-compassion.
Limitations and Future Research
Major strengths of this study are the large naturalistic sample in routine clinical practice, inclusion being based on clinical interview of both current and remitted patients, and the use of additional measures (OQ-45, PSWQ) to validate the identified profiles. This study also has several limitations. First, mindfulness profiles could have been more accurately estimated using latent transition analysis (LTA). LTA, in addition to between person variability, also accounts for within-person variability by incorporating post-treatment FFMQ scores. However, with respect to previous research, we aimed to replicate Gu et al. (2020) and to answer the clinical question whether profiles established before training are predictive of outcome; we constrained our profile analysis for this report to baseline FFMQ. LTA results will be reported elsewhere. Second, the fit indices did not consistently point to a four-profile solution. While the BIC and posterior classification probabilities indeed favored the 4-profile solution, the BLRT and SABIC favored a 7-profile solution. Because the 7-profile solution contained one profile with only 14 individuals and because a 5- or 6-profile solution would not result in new clearly “distinguishable” profiles, we decided to select the more parsimonious 4-profile solution. Future studies with larger samples may benefit from exploring the fit of >4 profiles (such as a 7-profile solution), but, at the same time, should be cautious for overfitting. Third, the entropy value of 0.62 is relatively low. Entropy values range from 0 to 1, with higher entropy values indicating a more accurate identification of the latent profiles. While a good value of entropy is considered to be 0.80 or higher, a bad or cutoff value for entropy is hard to specify (Weller et al., 2020). In addition, entropy values can be a poor tool for model selection (Collins & Lanza, 2009) and we therefore followed (Weller et al., 2020) to report but not rely on the entropy for selecting the number of profiles. Fourth, we used the 24-item FFMQ-SF to measure the facets of mindfulness, whereas previous studies used the 39-item FFMQ (Gu et al., 2020). Although the 5-factor structure of the FFMQ-SF has now been validated in the current sample and by Bohlmeijer et al. (2011) who additionally showed that the 5-factor structure was highly similar to the long version (high correlations between SF and long version; similar internal consistency in terms of Cronbach’s alpha (Bohlmeijer et al., 2011)), slight differences between the instruments could have resulted in differences in the observed latent profiles. Fifth, a considerable number of patients (34%) did not complete the questionnaires post-MBCT. Within the main analyses, the identification and evaluation of mindfulness profiles before MBCT was based on all available baseline data whereas the residualized change scores could only be calculated for patients with a full data set. Consequently, evaluating the means of post-MBCT and residualized change scores over those profiles could only be done for patients with a full data set. Although patients with a full data set hardly differed from patients without a post-treatment measurement, those differences may have slightly influenced the analyses and reduce generalizability to the whole (n = 754) sample. In addition, for a considerable number of patients, due to change in the clinical questionnaire set, a pre (112 out of 754) and post score (86 out of 500) on the OQ-45 was missing, which may have influenced reliability of estimation of OQ-45 scores across the different profiles. Therefore, we performed sensitivity analyses with ten imputed datasets and included variables that may have been related to missingness within the imputation process. The results of these analyses were almost identical to the original results, which strengthens the robustness of the findings. Of note, the number of imputed datasets as well as the number and selection of predictors within the sensitivity imputation models were chosen arbitrary, which introduces risk for systemic bias. However, despite this limitation, the results obtained from both the main analysis and the sensitivity analysis were nearly identical, suggesting that this issue may have minimal impact on the overall findings.
In conclusion, LPA is a person-centered method that in addition to traditionally used variable centered methods could help to better understand the overall construct of mindfulness and the relations between its individual facets. For future research, it is important to continue to assess whether mindfulness profiles are consistently identified in non-clinical and clinical samples, how they relate to measures of mental health, and whether mindfulness profiles in clinical samples differ from those in non-clinical samples. Furthermore, future research will benefit from studies that use a longitudinal design in which the predictive value of baseline profiles for treatment outcome can be further evaluated. In addition, studies aimed to assess whether MBCT specifically adapted to the needs of individuals (e.g., patients with a self-critical judgmental attitude) improve effectiveness of MBCT may be of particular interest. Moreover, the current study and the study of Gu et al. (2020) only identified the latent profile structure at a specific point in time. This prevents conclusions on whether a patient’s mindfulness profile changes in time (e.g., after a MBI), and whether those hypothesized changes in profile are related to changes in outcome. Latent transition analysis (LTA) could fill this gap. By means of LTA, it could be elucidated whether hypothesized improvement in mindfulness skills after an MBI (e.g., change of a “very low mindfulness” profile to a profile considered to be related to good scores on mental health measures) would go hand in hand with improvement in measures of mental health.
Data Availability
The data and the Mplus code used for the performed analyses used in this study are openly available in the Radboud Data Repository at 10.34973/n6r0-8547.
References
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., & Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment, 13(1), 27–45. https://doi.org/10.1177/1073191105283504
Baer, R. A., Smith, G. T., Lykins, E., Button, D., Krietemeyer, J., Sauer, S., Walsh, E., Duggan, D., & Williams, J. M. G. (2008). Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment, 15(3), 329–342. https://doi.org/10.1177/1073191107313003
Bakk, Z., & Vermunt, J. K. (2016). Robustness of stepwise latent class modeling with continuous distal outcomes. Structural Equation Modeling, 23(1), 20–31. https://doi.org/10.1080/10705511.2014.955104
Beck, A. T., Steer, R. A., & Brown, G. K. (1996). Beck depression inventory (BDI-II). The Psychological Corporation.
Bohlmeijer, E., Ten Klooster, P. M., Fledderus, M., Veehof, M., & Baer, R. (2011). Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment, 18(3), 308–320. https://doi.org/10.1177/1073191111408231
Bravo, A. J., Boothe, L. G., & Pearson, M. R. (2016). Getting personal with mindfulness: A latent profile analysis of mindfulness and psychological outcomes. Mindfulness, 7(2), 420–432. https://doi.org/10.1007/s12671-015-0459-7
Bravo, A. J., Pearson, M. R., & Kelley, M. L. (2018). Mindfulness and psychological health outcomes: A latent profile analysis among military personnel and college students. Mindfulness, 9(1), 258–270. https://doi.org/10.1007/s12671-017-0771-5
Bronchain, J., Raynal, P., & Chabrol, H. (2021). Dispositional mindfulness profiles and cannabis use in young adults. Journal of Rational-Emotive & Cognitive-Behavior Therapy, 39(4), 509–521. https://doi.org/10.1007/s10942-020-00382-z
Brown, D. B., Bravo, A. J., Roos, C. R., & Pearson, M. R. (2015). Five facets of mindfulness and psychological health: Evaluating a psychological model of the mechanisms of mindfulness. Mindfulness, 6(5), 1021–1032. https://doi.org/10.1007/s12671-014-0349-4
Browne, M. W., & Cudeck, R. (1992). Alternative ways of assessing model fit. Sociological Methods & Research, 21, 230–258. https://doi.org/10.1177/0049124192021002005
Calvete, E., Fernández-González, L., Echezarraga, A., & Orue, I. (2020). Dispositional mindfulness profiles in adolescents and their associations with psychological functioning and hypothalamic–pituitary–adrenal axis hormones. Journal of Youth and Adolescence, 49(7), 1406–1419. https://doi.org/10.1007/s10964-019-01128-6
Cheavens, J. S., Strunk, D. R., Lazarus, S. A., & Goldstein, L. A. (2012). The compensation and capitalization models: A test of two approaches to individualizing the treatment of depression. Behaviour Research and Therapy, 50(11), 699–706. https://doi.org/10.1016/j.brat.2012.08.002
Cladder-Micus, M. B., Speckens, A. E., Vrijsen, J. N., Donders, T., Becker, E. S., & Spijker, J. (2018). Mindfulness-based cognitive therapy for patients with chronic, treatment-resistant depression: A pragmatic randomized controlled trial. Depression and Anxiety, 35(10), 914–924. https://doi.org/10.1002/da.22788
Collins, L. M., & Lanza, S. T. (2009). Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences (Vol. 718). John Wiley & Sons.
Crane, R. S., Kuyken, W., Williams, J. M. G., Hastings, R. P., Cooper, L., & Fennell, M. J. (2012). Competence in teaching mindfulness-based courses: concepts, development and assessment. Mindfulness, 3(1), 76–84. https://doi.org/10.1007/s12671-011-0073-2
de Jong, K., & Spinhoven, P. (2008). De Nederlandse versie van de Outcome Questionnaire (OQ-45): een crossculturele validatie. Psychologie en Gezondheid, 36(1), 35–45. https://doi.org/10.1007/BF03077465
De Souza Marcovski, F. C., & Miller, L. J. (2022). A latent profile analysis of the five facets of mindfulness in a US adult sample: Spiritual and psychological differences among four profiles. Current Psychology, 42, 14223–14236. https://doi.org/10.1007/s12144-021-02546-1
Fernandez, A. C., Wood, M. D., Stein, L., & Rossi, J. S. (2010). Measuring mindfulness and examining its relationship with alcohol use and negative consequences. Psychology of Addictive Behaviors, 24(4), 608. https://doi.org/10.1037/a0021742
First, M. B., Gibbon, M., Spitzer, R. L., Williams, J. B., & Benjamin, L. S. (1997). Structured clinical interview for DSM-IV® axis ii personality disorders SCID-II. American Psychiatric Pub.
Ford, C. G., Wilson, J. M., Altman, N., Strough, J., & Shook, N. J. (2020). Profiles of mindfulness across adulthood. Mindfulness, 11(6), 1557–1569. https://doi.org/10.1007/s12671-020-01372-z
Gawrysiak, M. J., Grassetti, S. N., Greeson, J. M., Shorey, R. C., Pohlig, R., & Baime, M. J. (2018). The many facets of mindfulness and the prediction of change following Mindfulness-Based Stress Reduction (MBSR). Journal of Clinical Psychology, 74(4), 523–535. https://doi.org/10.1002/jclp.22521
Geurts, D. E., Compen, F. R., Van Beek, M. H., & Speckens, A. E. (2020). The effectiveness of mindfulness-based cognitive therapy for major depressive disorder: Evidence from routine outcome monitoring data. BJPsych Open, 6, e144. https://doi.org/10.1192/bjo.2020.118
Geurts, D. E., Haegens, N. M., Van Beek, M. H., Schroevers, M. J., Compen, F. R., & Speckens, A. E. (2021). Putting mindfulness-based cognitive therapy to the test in routine clinical practice: A transdiagnostic panacea or a disorder specific intervention? Journal of Psychiatric Research, 142, 144–152. https://doi.org/10.1016/j.jpsychires.2021.07.043
Goldberg, S. B., Tucker, R. P., Greene, P. A., Davidson, R. J., Kearney, D. J., & Simpson, T. L. (2019). Mindfulness-based cognitive therapy for the treatment of current depressive symptoms: A meta-analysis. Cognitive Behaviour Therapy, 48(6), 445–462. https://doi.org/10.1080/16506073.2018.1556330
Gómez-Odriozola, J., & Calvete, E. (2021). The role of dispositional mindfulness profiles as predictors of sleep problems through rumination in adolescents over time. Personality and Individual Differences, 180, 110966. https://doi.org/10.1016/j.paid.2021.110966
Greeson, J. M., Smoski, M. J., Suarez, E. C., Brantley, J. G., Ekblad, A. G., Lynch, T. R., & Wolever, R. Q. (2015). Decreased symptoms of depression after mindfulness-based stress reduction: Potential moderating effects of religiosity, spirituality, trait mindfulness, sex, and age. The Journal of Alternative and Complementary Medicine, 21(3), 166–174. https://doi.org/10.1089/acm.2014.0285
Gu, J., Karl, A., Baer, R., Strauss, C., Barnhofer, T., & Crane, C. (2020). Latent profile analysis of the Five Facet Mindfulness Questionnaire in a sample with a history of recurrent depression. Assessment, 27(1), 149–163. https://doi.org/10.1177/1073191117715114
Gu, J., Strauss, C., Crane, C., Barnhofer, T., Karl, A., Cavanagh, K., & Kuyken, W. (2016). Examining the factor structure of the 39-item and 15-item versions of the Five Facet Mindfulness Questionnaire before and after mindfulness-based cognitive therapy for people with recurrent depression. Psychological Assessment, 28(7), 791–802. https://doi.org/10.1037/pas0000263
Howard, M. C., & Hoffman, M. E. (2018). Variable-centered, person-centered, and person-specific approaches: Where theory meets the method. Organizational Research Methods, 21(4), 846–876. https://doi.org/10.1177/1094428117744021
Hu, L. T., & Bentler, P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6(1), 1–55. https://doi.org/10.1080/10705519909540118
Kabat-Zinn, J. (2009). Wherever you go, there you are: Mindfulness meditation in everyday life. Hachette Books.
Kimmes, J. G., Durtschi, J. A., & Fincham, F. D. (2017). Perception in romantic relationships: A latent profile analysis of trait mindfulness in relation to attachment and attributions. Mindfulness, 8(5), 1328–1338. https://doi.org/10.1007/s12671-017-0708-z
Kuyken, W., Hayes, R., Barrett, B., Byng, R., Dalgleish, T., Kessler, D., Lewis, G., Watkins, E., Brejcha, C., & Cardy, J. (2015). Effectiveness and cost-effectiveness of mindfulness-based cognitive therapy compared with maintenance antidepressant treatment in the prevention of depressive relapse or recurrence (PREVENT): A randomised controlled trial. The Lancet, 386(9988), 63–73. https://doi.org/10.1016/S0140-6736(14)62222-4
Kuyken, W., Warren, F. C., Taylor, R. S., Whalley, B., Crane, C., Bondolfi, G., Hayes, R., Huijbers, M., Ma, H., & Schweizer, S. (2016). Efficacy of mindfulness-based cognitive therapy in prevention of depressive relapse: An individual patient data meta-analysis from randomized trials. JAMA Psychiatry, 73(6), 565–574. https://doi.org/10.1001/jamapsychiatry.2016.0076
Lam, K. F., Lim, H. A., Kua, E. H., Griva, K., & Mahendran, R. (2018). Mindfulness and cancer patients’ emotional states: A latent profile analysis among newly diagnosed cancer patients. Mindfulness, 9(2), 521–533. https://doi.org/10.1007/s12671-017-0794-y
Lambert, M. J., Burlingame, G. M., Umphress, V., Hansen, N. B., Vermeersch, D. A., Clouse, G. C., & Yanchar, S. C. (1996). The reliability and validity of the Outcome Questionnaire. Clinical Psychology & Psychotherapy, 3(4), 249–258. https://doi.org/10.1002/(SICI)1099-0879(199612)3:4<249::AID-CPP106>3.0.CO;2-S
Lecuona, O., García-Rubio, C., de Rivas, S., Moreno-Jiménez, J. E., & Rodríguez-Carvajal, R. (2022). Unraveling heterogeneities in mindfulness profiles: A review and latent profile analysis of the Five Facet Mindfulness Questionnaire Short-Form (FFMQ-SF) in the Spanish Population. Mindfulness, 13(8), 2031–2046. https://doi.org/10.1007/s12671-022-01939-y
Lubke, G., & Neale, M. C. (2006). Distinguishing between latent classes and continuous factors: Resolution by maximum likelihood? Multivariate Behavioral Research, 41(4), 499–532. https://doi.org/10.1207/s15327906mbr4104_4
Meyer, T. J., Miller, M. L., Metzger, R. L., & Borkovec, T. D. (1990). Development and validation of the penn state worry questionnaire. Behaviour Research and Therapy, 28(6), 487–495. https://doi.org/10.1016/0005-7967(90)90135-6
Muthén, L. K., & Muthén, B. O. (1998). Mplus user's guide (8th ed.). Muthén & Muthén.
Neff, K. (2003). Self-compassion: An alternative conceptualization of a healthy attitude toward oneself. Self and identity, 2(2), 85–101. https://doi.org/10.1080/15298860309032
Neff, K., & Vonk, R. (2009). Self-compassion versus global self-esteem: Two different ways of relating to oneself. Journal of Personality, 77(1), 23–50. https://doi.org/10.1111/j.1467-6494.2008.00537.x
Nyklíček, I., van Son, J., Pop, V. J., Denollet, J., & Pouwer, F. (2016). Does Mindfulness-Based Cognitive Therapy benefit all people with diabetes and comorbid emotional complaints equally? Moderators in the DiaMind trial. Journal of Psychosomatic Research, 91, 40–47. https://doi.org/10.1016/j.jpsychores.2016.10.009
Nylund, K. L., Asparouhov, T., & Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A Monte Carlo simulation study. Structural Equation Modeling, 14(4), 535–569. https://doi.org/10.1080/10705510701575396
Pearson, M. R., Lawless, A. K., Brown, D. B., & Bravo, A. J. (2015). Mindfulness and emotional outcomes: Identifying subgroups of college students using latent profile analysis. Personality and Individual Differences, 76, 33–38. https://doi.org/10.1016/j.paid.2014.11.009
RStudio Team. (2019). RStudio: Integrated development for R. RStudio, PBC, Boston, MA. http://www.rstudio.com/
Sahdra, B. K., Ciarrochi, J., Parker, P. D., Basarkod, G., Bradshaw, E. L., & Baer, R. (2017). Are people mindful in different ways? Disentangling the quantity and quality of mindfulness in latent profiles and exploring their links to mental health and life effectiveness. European Journal of Personality, 31(4), 347–365. https://doi.org/10.1002/per.2108
Segal, Z. V., Williams, J. M. G., & Teasdale, J. D. (2002). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. Guilford Press.
Shapiro, S. L., Brown, K. W., Thoresen, C., & Plante, T. G. (2011). The moderation of mindfulness‐based stress reduction effects by trait mindfulness: results from a randomized controlled trial. Journal of Clinical Psychology, 67(3), 267–277. https://doi.org/10.1002/jclp.20761
Sheehan, D. V., Lecrubier, Y., Sheehan, K. H., Amorim, P., Janavs, J., Weiller, E., Hergueta, T., Baker, R., & Dunbar, G. C. (1998). The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry, 59(20), 22–33.
Spurk, D., Hirschi, A., Wang, M., Valero, D., & Kauffeld, S. (2020). Latent profile analysis: A review and “how to” guide of its application within vocational behavior research. Journal of Vocational Behavior, 120, 103445. https://doi.org/10.1016/j.jvb.2020.103445
Stanmyre, J. F., Mills, D. J., Anthony, W. L., & Nower, L. (2022). Mindfulness profiles among gamblers: Exploring differences in gambling behaviors, motivations, cognitions, and mental health. Mindfulness, 13(2), 339–350. https://doi.org/10.1007/s12671-021-01791-6
Tein, J.-Y., Coxe, S., & Cham, H. (2013). Statistical power to detect the correct number of classes in latent profile analysis. Structural Equation Modeling, 20(4), 640–657. https://doi.org/10.1080/10705511.2013.824781
Van Aalderen, J., Donders, A., Giommi, F., Spinhoven, P., Barendregt, H., & Speckens, A. (2012). The efficacy of mindfulness-based cognitive therapy in recurrent depressed patients with and without a current depressive episode: A randomized controlled trial. Psychological Medicine, 42(5), 989–1001. https://doi.org/10.1017/S0033291711002054
Van Buuren, S. (2018). Flexible imputation of missing data. CRC press.
Van den Brink, E., & Koster, F. (2015). Mindfulness-based compassionate living. Routledge.
Van der Does, A. (2002). BDI-II-NL. Handleiding. De Nederlandse versie van de Beck depression inventory. Harcourt Test Publishers.
van der Heiden, C., Muris, P., Bos, A. E., van der Molen, H., & Oostra, M. (2009). Normative data for the Dutch version of the Penn State Worry Questionnaire. Netherlands Journal of Psychology, 65, 69–75. https://doi.org/10.1007/BF03080129
van Rijsoort, S., Emmelkamp, P., & Vervaeke, G. (1999). The Penn State Worry Questionnaire and the Worry Domains Questionnaire: Structure, reliability and validity. Clinical Psychology & Psychotherapy, 6(4), 297–307. https://doi.org/10.1002/(SICI)1099-0879(199910)6:4<297::AID-CPP206>3.0.CO;2-E
Vuijk, R. (2023). Nederlands Interview voor Diagnostiek Autismespectrumstoornis bij volwassenen (NIDA) - Handleiding en Interview (derde, geheel herziene druk) [Dutch Interview for Diagnostic assessment Autism spectrum disorder in adults (NIDA) - Manual and Interview (third, fully revised edition)]. AutismeSpectrumNederland and Sarr Autisme Rotterdam. http://www.autismespectrumnederland.nl/wp-content/uploads/2016-Vuijk-NIDA.pdf
Wang, J., Wei, L., Zhu, L., & Schroevers, M. J. (2022). Profiles of mindfulness in cancer patients and associations with psychological outcomes and coping strategies: A person-centered approach. Journal of Clinical Psychology. https://doi.org/10.1002/jclp.23346
Weller, B. E., Bowen, N. K., & Faubert, S. J. (2020). Latent class analysis: A guide to best practice. Journal of Black Psychology, 46(4), 287–311. https://doi.org/10.1177/0095798420930932
Werner, A. M., Tibubos, A. N., Rohrmann, S., & Reiss, N. (2019). The clinical trait self-criticism and its relation to psychopathology: A systematic review–Update. Journal of Affective Disorders, 246, 530–547. https://doi.org/10.1016/j.jad.2018.12.069
Williams, J. M. G., Crane, C., Barnhofer, T., Brennan, K., Duggan, D. S., Fennell, M. J., Hackmann, A., Krusche, A., Muse, K., & Von Rohr, I. R. (2014). Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: A randomized dismantling trial. Journal of Consulting and Clinical Psychology, 82(2), 275–286. https://doi.org/10.1037/a0035036
Zhang, J., Deng, X., Huang, L., Zeng, H., Wang, L., & Wen, P. (2019). Profile of trait mindfulness and its association with emotional regulation for early adolescents. Personality and Individual Differences, 147, 12–17. https://doi.org/10.1016/j.paid.2019.04.008
Zhu, L., Wang, J., & Schroevers, M. J. (2020). Looking beyond the value of individual facets of mindfulness: A person-centered examination of mindfulness. Mindfulness, 11(10), 2349–2359. https://doi.org/10.1007/s12671-020-01452-0
Acknowledgements
The authors would like to thank all MBCT teachers and therapists who taught the MBCT, Irma Veliscek-van Maren, for organizing the MBCT interventions and collecting the routine outcome monitoring (ROM) assessments. We thank Geert Schattenberg (datamanager) for importing the ROM data and thank Alexander van Daele, Isa van Dord, Lorraine Hagemeijer, Iris van Oostrom, and Anna Kirschberger for assisting with data important. The authors express their sincere gratitude to the reviewers for their invaluable feedback on the statistical approach employed in this study. The reviewers’ insightful comments and suggestions have significantly enhanced the quality and rigor of the current study.
Artificial Intelligence
Artificial intelligence was used to improve English language of the manuscript.
Author information
Authors and Affiliations
Contributions
All authors contributed to this manuscript. Anne Speckens: conceptualization, supervision, supervision of clinical assessments and MBCT courses, writing—review and editing. Jelle Lubbers: methodology, data curation, formal analysis, visualization, writing—original draft. Dirk Geurts: investigation, data curation, conceptualization, supervision, writing—review and editing. Philip Spinhoven: methodology, investigation, formal analysis, conceptualization, supervision, writing—review and editing. Jan Spijker: conceptualization, supervision, writing—review and editing. Mira Cladder-Micus: conceptualization, writing—review and editing.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Ethics Statement
All procedures were in accordance with the 1964 Helsinki Declaration and later amendments. Informed consent was obtained by means of an opt-out system, meaning that patients were informed that their anonymized outcome data could be utilized for scientific research purposes. The medical ethical committee (“Medisch Etische Toetsingscommissie Oost-Nederland”) waived the need for approval (CMO dossier: 2020–7226) per the Dutch Medical Research Involving Human Subjects Act, since participants were not subject to additional procedures or required to follow rules of behavior.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lubbers, J., Spinhoven, P., Cladder-Micus, M.B. et al. Latent Profile Analysis of the Five Facet Mindfulness Questionnaire (FFMQ) Subscales in a Naturalistic Sample of Patients with Past or Present Major Depression: A Replication and Extension Study. Mindfulness 15, 403–420 (2024). https://doi.org/10.1007/s12671-023-02298-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-023-02298-y