Abstract
Objectives
During the pandemic, establishing effective interventions to mitigate burnout is essential to ensure the provision of stable healthcare. This study examined the efficacy of a 4-week online mindfulness program on healthcare workers’ burnout to explore whether brief online programs can influence healthcare workers’ wellbeing by decreasing signs and symptoms of burnout.
Methods
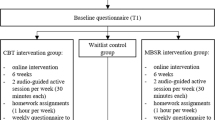
We examined differences between healthcare workers’ burnout (emotional exhaustion, depersonalization, and personal accomplishment) at three time points (baseline, post-intervention, and follow-up survey) using linear regression analyses accounting and without accounting for covariates. Covariates included demographic (age, sex), work-related (year of work experience, mode of care), resiliency (the ability to bounce back from hardship), and mindfulness-related factors (number of practices per week, prior experience of mindfulness, number of sessions attended). A total of n = 130 healthcare workers in Ontario, Canada, participated in the study (October 2020 to March 2021).
Results
Without accounting for the covariates, the two components of burnout, emotional exhaustion (feelings of being emotionally overextended and exhausted by one’s work) and depersonalization (an unfeeling and impersonal response toward recipients of one’s service, care, treatment, or instruction) levels, were significantly lower after the 4-week mindfulness program compared to the baseline and remained lower after 4 weeks. However, the personal accomplishment level (feelings of competence and achievement in one’s work) remained unchanged after the mindfulness program. Resiliency significantly contributed to reducing emotional exhaustion. Number of mindfulness practices contributed to reducing emotional exhaustion, depersonalization, and enhancing personal accomplishment.
Conclusions
The findings provide a basis for healthcare organizational development decision-makers to consider employee-facing mindfulness programs. It also informs curriculum designers of mindfulness education and training programs to create online programs for maximum efficacy.
Similar content being viewed by others
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Aguayo-Estremera, R., Cañadas, G. R., Ortega-Campos, E., Ariza, T., & De la Fuente-Solana, E. I. (2023). Validity Evidence for the Internal Structure of the Maslach Burnout Inventory-Student Survey: A Comparison between Classical CFA Model and the ESEM and the Bifactor Models. Mathematics, 11(6), 1515. https://doi.org/10.3390/math11061515
Ali, P., & Younas, A. (2021). Understanding and interpreting regression analysis. Evidence Based Nursing, 24(4), 116–118. https://doi.org/10.1136/ebnurs-2021-103425
Alsubaie, M., et al. (2017). Mechanisms of action in mindfulness-based cognitive therapy (MBCT) and mindfulness-based stress reduction (MBSR) in people with physical and/or psychological conditions: A systematic review. Clinical Psychology Review, 55, 74–91.
Amanullah, S., & Ramesh Shankar, R. (2020). The impact of COVID-19 on physician burnout globally: A review. Healthcare, 8(4), 421. https://doi.org/10.3390/healthcare8040421
Ballinger, G. A. (2004). Using generalized estimating equations for longitudinal data analysis. Organizational Research Methods, 7(2), 127–150. https://doi.org/10.3390/healthcare8040421
Behan, C. (2020). The benefits of Meditation and Mindfulness practices during times of crisis such as Covid-19. Irish Journal of Psychological Medicine, 37(4), 256–258. https://doi.org/10.1017/ipm.2020.38
Bodini, L., Bonetto, C., Cheli, S., Del Piccolo, L., Rimondini, M., Rossi, A., Carta, A., Porru, S., Amaddeo, F., & Lasalvia, A. (2022). Effectiveness of a Mindful Compassion Care Program in reducing burnout and psychological distress amongst frontline hospital nurses during the COVID-19 pandemic: A study protocol for a randomized controlled trial. Trials, 23(1), 1–11. https://doi.org/10.1186/s13063-022-06666-2
Brackett, M. (2019). Permission to feel: Unlocking the power of emotions to help our kids, ourselves, and our society thrive. Celadon Books.
Brady, S., O’Connor, N., Burgermeister, D., & Hanson, P. (2012). The impact of mindfulness meditation in promoting a culture of safety on an acute psychiatric unit. Perspectives in Psychiatric Care, 48(3), 129–137. https://doi.org/10.1111/j.1744-6163.2011.00315.x
Chen, K.-Y., Yang, C.-M., Lien, C.-H., Chiou, H.-Y., Lin, M.-R., Chang, H.-R., & Chiu, W.-T. (2013). Burnout, job satisfaction, and medical malpractice among physicians. International Journal of Medical Sciences, 10(11), 1471–1478. https://doi.org/10.7150/ijms.6743
Clarke, J., & Nicholson, J. (2010). Resilience: bounce back from whatever life throws at you. Hachette UK.
Cohen-Katz, J., Wiley, S. D., Capuano, T., Baker, D. M., & Shapiro, S. (2005). The effects of mindfulness-based stress reduction on nurse stress and burnout, Part II: A quantitative and qualitative study. Holistic Nursing Practice, 19(1), 26–35. https://doi.org/10.1097/00004650-200501000-00008
De Kock, J. H., Latham, H. A., Leslie, S. J., Grindle, M., Munoz, S.-A., Ellis, L., Polson, R., & O’Malley, C. M. (2021). A rapid review of the impact of COVID-19 on the mental health of healthcare workers: Implications for supporting psychological wellbeing. BMC Public Health, 21(1), 1–18. https://doi.org/10.1186/s12889-020-10070-3
Desson, Z., Weller, E., McMeekin, P., & Ammi, M. (2020). An analysis of the policy responses to the COVID-19 pandemic in France, Belgium, and Canada. Health Policy and Technology, 9(4), 430–446. https://doi.org/10.1016/j.hlpt.2020.09.002
Detsky, A. S., & Bogoch, I. I. (2020). COVID-19 in Canada: Experience and response. JAMA, 324(8), 743–744. https://doi.org/10.1001/jama.2020.14033
Djalante, R., Shaw, R., & De Wit, A. (2020). Building resilience against biological hazards and pandemics: COVID-19 and its implications for the Sendai Framework. Progress in Disaster Science, 6, 100080. https://doi.org/10.1016/j.pdisas.2020.100080
Dreison, K. C., Luther, L., Bonfils, K. A., Sliter, M. T., McGrew, J. H., & Salyers, M. P. (2018). Job burnout in mental health providers: A meta-analysis of 35 years of intervention research. Journal of Occupational Health Psychology, 23(1), 18. https://doi.org/10.1037/ocp0000047
Frank, J. L., Reibel, D., Broderick, P., Cantrell, T., & Metz, S. (2015). The effectiveness of mindfulness-based stress reduction on educator stress and wellbeing: Results from a pilot study. Mindfulness, 6(2), 208–216. https://doi.org/10.1007/s12671-013-0246-2
Gramaglia, C., Marangon, D., Azzolina, D., Guerriero, C., Lorenzini, L., Probo, M., Rudoni, M., Gambaro, E., & Zeppegno, P. (2021). The mental health impact of 2019-nCOVID on healthcare workers from North-Eastern Piedmont, Italy. Focus on burnout. Frontiers in public health, 9, 667379. https://doi.org/10.3389/fpubh.2021.667379
Happell, B., Martin, T., & Pinikahana, J. (2003). Burnout and job satisfaction: A comparative study of psychiatric nurses from forensic and a mainstream mental health service. International Journal of Mental Health Nursing, 12(1), 39–47. https://doi.org/10.1046/j.1440-0979.2003.00267.x
Hardin, J. W. (2005). Generalized estimating equations (GEE). Encyclopedia of Statistics in Behavioral Science. https://doi.org/10.1002/0470013192.bsa250
Heymann, D. L., & Shindo, N. (2020). COVID-19: What is next for public health? The Lancet, 395(10224), 542–545. https://doi.org/10.1016/s0140-6736(20)30374-3
Ireland, M. J., Clough, B., Gill, K., Langan, F., O’Connor, A., & Spencer, L. (2017). A randomized controlled trial of mindfulness to reduce stress and burnout among intern medical practitioners. Medical Teacher, 39(4), 409–414. https://doi.org/10.1080/0142159x.2017.1294749
Irving, J. A., Dobkin, P. L., & Park, J. (2009). Cultivating mindfulness in health care professionals: A review of empirical studies of mindfulness-based stress reduction (MBSR). Complementary Therapies in Clinical Practice, 15(2), 61–66. https://doi.org/10.1016/j.ctcp.2009.01.002
Iwanicki, E. F., & Schwab, R. L. (1981). A cross validation study of the Maslach Burnout Inventory. Educational and Psychological Measurement, 41(4), 1167–1174. https://doi.org/10.1177/001316448104100425
Jasbi, M., et al. (2018). Influence of adjuvant mindfulness-based cognitive therapy (MBCT) on symptoms of posttraumatic stress disorder (PTSD) in veterans–results from a randomized control study. Cognitive Behaviour Therapy, 47(5), 431–446.
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology: Science and Practice, 10(2), 144–156. https://doi.org/10.1093/clipsy.bpg016
Klatt, M. D., Bawa, R., Gabram, O., Blake, A., Steinberg, B., Westrick, A., & Holliday, S. (2020). Embracing change: A mindful medical center meets COVID-19. Global Advances in Health and Medicine, 9, 2164956120975369. https://doi.org/10.1177/2164956120975369
Lamothe, M., Rondeau, É., Malboeuf-Hurtubise, C., Duval, M., & Sultan, S. (2016). Outcomes of MBSR or MBSR-based interventions in health care providers: A systematic review with a focus on empathy and emotional competencies. Complementary Therapies in Medicine, 24, 19–28. https://doi.org/10.1016/j.ctim.2015.11.001
Lasalvia, A., Amaddeo, F., Porru, S., Carta, A., Tardivo, S., Bovo, C., Ruggeri, M., & Bonetto, C. (2021). Levels of burn-out among healthcare workers during the COVID-19 pandemic and their associated factors: a cross-sectional study in a tertiary hospital of a highly burdened area of north-east Italy. BMJ Open, 11(1), e045127. https://doi.org/10.1136/bmjopen-2020-045127
Leo, C. G., Sabina, S., Tumolo, M. R., Bodini, A., Ponzini, G., Sabato, E., & Mincarone, P. (2021). Burnout among healthcare workers in the COVID 19 era: a review of the existing literature. Frontiers in public health, 9, 750529. https://doi.org/10.3389/fpubh.2021.750529
Luberto, C. M., Goodman, J. H., Halvorson, B., Wang, A., & Haramati, A. (2020). Stress and coping among health professions students during COVID-19: A perspective on the benefits of mindfulness. Global Advances in Health and Medicine, 9, 2164956120977827. https://doi.org/10.1177/2164956120977827
MacDougall, A. G., Price, E., Vandermeer, M. R., Lloyd, C., Bird, R., Sethi, R., Shanmugalingam, A., Carr, J., Anderson, K. K., & Norman, R. M. (2019). Youth-focused group mindfulness-based intervention in individuals with early psychosis: A randomized pilot feasibility study. Early Intervention in Psychiatry, 13(4), 993–998. https://doi.org/10.1111/eip.12753
Marotta, M., Gorini, F., Parlanti, A., Berti, S., & Vassalle, C. (2022). Effect of Mindfulness-Based Stress Reduction on the Wellbeing, Burnout and Stress of Italian Healthcare Professionals during the COVID-19 Pandemic. Journal of Clinical Medicine, 11(11), 3136. https://doi.org/10.3390/jcm11113136
Maslach C., Jackson S. E., & Leiter M. P. (1996). Maslach Burnout Inventory manual (3rd ed.). Consulting Psychologists Press.
Maunder, R. G., Leszcz, M., Savage, D., Adam, M. A., Peladeau, N., Romano, D., Rose, M., & Schulman, R. B. (2008). Applying the lessons of SARS to pandemic influenza. Canadian Journal of Public Health, 99(6), 486–488. https://doi.org/10.1007/bf03403782
Morse, G., Salyers, M. P., Rollins, A. L., Monroe-DeVita, M., & Pfahler, C. (2012). Burnout in mental health services: A review of the problem and its remediation. Administration and Policy in Mental Health and Mental Health Services Research, 39(5), 341–352. https://doi.org/10.1007/s10488-011-0352-1
Murphy, Y. (2014). The role of job satisfaction, resilience, optimism and emotional intelligence in the prediction of burnout (Bachelors final year project). Dublin Business School, Ireland. Diperoleh dari. https://esource.dbs.ie/handle/10788/2276
Nagoski, E., & Nagoski, A. (2020). Burnout: The secret to unlocking the stress cycle. Ballantine Books.
Nunnally, J. C., & Bernstein, I. (1978). Psychometric testing. McGraw-Hill.
Osman, I., Hamid, S., & Singaram, V. S. (2021). Efficacy of a brief online mindfulness-based intervention on the psychological wellbeing of health care professionals and trainees during the COVID-19 pandemic: A mixed method design. Health SA Gesondheid (online), 26, 1–9. https://doi.org/10.4102/hsag.v26i0.1682
Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G., Papoutsi, E., & Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain, Behavior, and Immunity, 88, 901–907. https://doi.org/10.2139/ssrn.3594632
Pérula-de Torres, L. Á., Verdes-Montenegro-Atalaya, J. C., Melús-Palazón, E., García-de Vinuesa, L., Valverde, F. J., Rodríguez, L. A., Lietor-Villajos, N., Bartolomé-Moreno, C., Moreno-Martos, H., & García-Campayo, J. (2021). Comparison of the effectiveness of an abbreviated program versus a standard program in mindfulness, self-compassion and self-perceived empathy in tutors and resident intern specialists of family and community medicine and nursing in Spain. International Journal of Environmental Research and Public Health, 18(8), 4340. https://doi.org/10.3390/ijerph18084340
Polizzi, C., Lynn, S. J., & Perry, A. (2020). Stress and coping in the time of COVID-19: pathways to resilience and recovery. Clinical Neuropsychiatry, 17(2), 59–62. https://doi.org/10.36131/CN20200204
Prasad, K., McLoughlin, C., Stillman, M., Poplau, S., Goelz, E., Taylor, S., Nankivil, N., Brown, R., Linzer, M., & Cappelucci, K. (2021). Prevalence and correlates of stress and burnout among US healthcare workers during the COVID-19 pandemic: A national cross-sectional survey study. EClinicalMedicine, 35, 100879. https://doi.org/10.1016/j.eclinm.2021.100879
Public Health Ontario. (2020). Enhanced Epidemiological Summary: COVID-19 in Ontario: a summary of wave 1 transmission patterns and case identification. Public Health Ontario.
Sandhu, H. S., Smith, R. W., Jarvis, T., O’Neill, M., Di Ruggiero, E., Schwartz, R., Rosella, L. C., Allin, S., & Pinto, A. D. (2022). Early Impacts of the COVID-19 Pandemic on Public Health Systems and Practice in 3 Canadian Provinces From the Perspective of Public Health Leaders: A Qualitative Study. Journal of Public Health Management and Practice, 28(6), 702–711. https://doi.org/10.1097/phh.0000000000001596
Shaw, S. C. (2020). Hopelessness, helplessness and resilience: The importance of safeguarding our trainees’ mental wellbeing during the COVID-19 pandemic. Nurse Education in Practice, 44, 102780. https://doi.org/10.1016/j.nepr.2020.102780
Smith, G. D., Ng, F., & Li, W. H. C. (2020). COVID-19: Emerging compassion, courage and resilience in the face of misinformation and adversity. Journal of Clinical Nursing, 29(9–10), 1425–1428. https://doi.org/10.1111/jocn.15231
Smith-Carrier, T., Koffler, T., Mishna, F., Wallwork, A., Daciuk, J., & Zeger, J. (2015). Putting your mind at ease: Findings from the Mindfulness Ambassador Council programme in Toronto area schools. Journal of Children’s Services, 10(4), 376–392. https://doi.org/10.1108/jcs-10-2014-0046
Sultana, A., Sharma, R., Hossain, M. M., Bhattacharya, S., & Purohit, N. (2020). Burnout among healthcare providers during COVID-19: Challenges and evidence-based interventions. Indian J Med Ethics, 5(4), 308–311. https://doi.org/10.20529/ijme.2020.73
Tan, B. Y., Kanneganti, A., Lim, L. J., Tan, M., Chua, Y. X., Tan, L., Sia, C. H., Denning, M., Goh, E. T., & Purkayastha, S. (2020). Burnout and associated factors among health care workers in Singapore during the COVID-19 pandemic. Journal of the American Medical Directors Association, 21(12), 1751–175. e81755. https://doi.org/10.1016/j.jamda.2020.09.035
Tuite, A. R., Fisman, D. N., Odutayo, A., Bobos, P., Allen, V., Bogoch, I., Allen, V., Bogoch, I. I., Brown, A. D., Evans, G. A., Greenberg, A., Hopkins, J., Maltsev, A., Manuel, D. G., McGeer, A., Morris, A. M., Mubareka, S., Munshi, L., Murty, V. K., ..., Jüni P. on behalf of the Ontario COVID-19 Science Advisory Table. (2021). COVID-19 hospitalizations, ICU admissions and deaths associated with the new variants of concern. Science Briefs of the Ontario COVID-19 Science Advisory Table, 1(18), 1–10. https://doi.org/10.47326/ocsat.2021.02.18.1.0
Wagaman, M. A., Geiger, J. M., Shockley, C., & Segal, E. A. (2015). The role of empathy in burnout, compassion satisfaction, and secondary traumatic stress among social workers. Social Work, 60(3), 201–209. https://doi.org/10.1093/sw/swv014
Acknowledgements
We thank Fariha Chowdhury and Nadine Proulx for conducting a literature review, Nicole Adams for her support in data collection, and Nicole Mace for her support in tailoring the mindfulness program, and promoting and implementing the mindfulness program for healthcare workers through a frontline wellness program. We also thank Mindfulness Without Borders for their support in retooling the mindfulness program and Georgian College for their help in the study. Most importantly, we thank all the healthcare workers and facilitators who participated in this study.
Funding
This study was supported by a College and Community Innovation Program- Applied Research Rapid Response to COVID-19 Grant funded by the Natural Sciences and Engineering Research Council of Canada (Award # COVPJ 554453–20).
Author information
Authors and Affiliations
Contributions
All authors: conceptualization. Soyeon Kim: data curation, writing—original draft preparation, quantitative data analysis. Sarah Hunter: critical revisions, writing—reviewing and editing.
Corresponding author
Ethics declarations
Ethics Approval and Consent To Participate
All data collection, analysis, and dissemination protocols were reviewed and approved by the Waypoint Centre for Mental Healthcare’s ethics review board (Protocol ref. # HPRA#20.07.27).
Informed Consent
Written informed consent was obtained from the participants for anonymized participant information to be published in this article.
Conflict of Interest
Soyeon Kim declares no conflict of interest. During the data collection period, Sarah Hunter worked with Mindfulness Without Border (MWB), facilitating mindfulness programs for other institutions. Sarah Hunter was no longer in contract with MWB during the manuscript preparation period.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kim, S., Hunter, S. Can Brief Online Mindfulness Programs Mitigate Healthcare Workers’ Burnout amid the COVID-19 Pandemic?. Mindfulness 14, 1930–1939 (2023). https://doi.org/10.1007/s12671-023-02175-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-023-02175-8