Abstract
Objectives
Chronic pain affects 1 in 5 Europeans, with a prevalence in Spain of 11%. It is one of the main causes of medical consultation and is associated with high personal, social, and economic costs with diverse psychological repercussions. Several studies have shown the effectiveness of psychological therapies in the treatment of chronic pain, including mindfulness-based therapies. In this regard, mindfulness-based pain management (MBPM) has evidenced significant positive changes in patients with chronic pain, but so far, no RCT study has been conducted. Therefore, the main purpose of this study is to explore the results of the MBPM program with chronic pain patients. Additionally, we will analyze the differential efficacy of the MBPM program on fibromyalgia versus non-fibromyalgia chronic pain patients.
Methods
Ninety patients with chronic pain were randomized to experimental group MBPM (50 patients) and wait-list control group (40 patients) and assessed at pre- and post-treatment in demographic and pain-related variables, psychopathological symptoms, cognitive variables, resilience, and quality of life.
Results
Findings showed moderate to large effects in favor of the experimental group in pain management and acceptance, use of analgesics, psychopathological symptoms, general negative thoughts, self-blame, mental-health-related quality of life, and resilience. Non-fibromyalgia chronic pain patients benefited significantly more than participants with fibromyalgia.
Conclusions
The positive impact of the MBPM program on critical variables related to chronic pain provides evidence of its efficacy, which could be enhanced with the inclusion of complementary therapeutic CBT components to address sleep problems, need for control, and rumination.
Trial Registration
ClinicalTrials.gov (NCT03992612).
Similar content being viewed by others
Chronic pain affects 1 in 5 Europeans (19%), with a prevalence in Spain of 11% (Breivik et al., 2006). It is one of the main causes of medical consultation; it affects women more than men, of working age, and it is associated with high personal, social, and economic costs (Díaz et al., 2003). Apart from the enormous societal costs that result from the burden of chronic pain and its suffering, it affects every aspect of patients’ lives. Psychological repercussions of chronic pain are diverse, including sleep disturbances, high levels of anxiety and depression (Naylor et al., 2012), or alterations in social relations (Lledó et al., 2013).
Several pathologies involve chronic pain, such as migraine, lower back pain, osteoarthritis, rheumatoid arthritis, and fibromyalgia, but few studies establish differential profiles among the various patients who have chronic pain (Porter-Moffit et al., 2006). In this regard, fibromyalgia is one identified cause of chronic widespread pain, although of uncertain etiology. It is one of the most disabling types of chronic pain, and is often difficult to diagnose and treat, so a fibromyalgia patient is one of the costliest patients to health services, consuming triple the health resources of any other chronic patient (Pastor et al., 2010).
From a therapeutic point of view, various studies have shown the effectiveness of cognitive-behavioral therapy (CBT) in the treatment of chronic pain—both associated or not with fibromyalgia—albeit with a moderate effect size (Eccleston & Crombez, 2017; Ehde et al., 2014). In a recent meta-analysis of randomized controlled trials on the treatment of chronic pain (Khoo et al., 2019), the authors found 13 studies on the effectiveness of CBT compared to a control group, seven studies on mindfulness-based stress reduction (MBSR) therapy compared to a control group, and only one study comparing these two therapeutic strategies, with good results in both therapies. The MBSR is a group-based intervention that focuses on building awareness and acceptance of moment-to-moment experiences, including physical discomfort and difficult emotions. Core components of MBSR include increasing awareness of one’s body, emotions, sensations, and thoughts, as well as learning self-regulation strategies and more adaptive responses to stress (Kabat-Zinn, 1982, 1990; Kabat-Zinn et al., 1985).
MBSR has been applied to patients with chronic pain, with good results in many studies (Haugmark et al., 2019; Hilton et al., 2017; Khoury et al., 2017). It is considered to belong to the first generation of mindfulness protocols, more focused on attention training, compared to second-generation protocols that integrate ethical and spiritual elements of Buddhism such as “loving kindness,” non-attachment, or compassion (Van Gordon et al., 2015). In this regard, and following the ideas of the second-generation protocols, Burch (2008) designed a specific program for pain management, the mindfulness-based pain management (MBPM).
MBPM has been evaluated by the original authors of the program (Cusens et al., 2010), showing significant positive changes in patients with chronic pain, with medium to large effect sizes on self-report measures of depression, positive outlook, pain acceptance (activity engagement and disengaging from the struggle to control or avoid pain), pain self-efficacy (individual’s confidence in his/her ability to perform specific behaviors while experiencing pain), and pain catastrophizing (rumination, magnification, and helplessness), in the absence of reduced pain intensity. In another study carried out by Brown and Jones (2013), patients with musculoskeletal pain in the MBPM group showed significant improvements in mental health, improved engagement in pain self-management, and greater perceived control of pain, with no reductions in clinical or experimental pain ratings. However, no further RCT studies have been conducted with the MBPM program. Therefore, the main purpose of this study is to explore the results of the MBPM program with chronic pain patients on different variables, such as pain, mental health, negative thoughts, pain catastrophizing, resilience, and quality of life. A second aim of the study is to analyze the differential efficacy of the MBPM program on fibromyalgia versus non-fibromyalgia chronic pain patients. In this regard, we hypothesized that patients receiving the MBPM program will obtain better results than patients in the control group, and that patients with fibromyalgia will have more limited results compared to non-fibromyalgia chronic pain patients.
Method
Participants
To estimate the sample size, a power analysis was performed using the statistical package G*Power version 3.1.9.7 for Windows. An a priori analysis was carried out (using t-tests to calculate differences between two independent groups), with the alpha level set to 0.05 (two-tailed). Based on previous studies related to this population (Brown & Jones, 2013; Cusens et al., 2010), if a medium to large effect size were assumed (d = 0.65), 39 participants would be needed in each group to achieve the recommended minimum power of 0.80 (Cohen, 1988, 1992). Anticipating a higher dropout rate in the experimental group than in the control group, the size of the groups was finally set at 50 and 40, respectively.
The sample consists of patients with non-oncological chronic pain who responded to the announcement of the launch of the MBPM program in the VITHAS Hospital of Vitoria, Spain. This program was provided at no charge to the participants. The admission criteria were the following: (a) being 18 years or older; (b) having a history of chronic pain for over 6 months; (c) not suffering from a severe mental illness (psychosis, bipolar disorder, major depressive disorder) nor an addictive disorder; (d) being able to complete the questionnaires; (e) not undergoing psychological treatment; and (f) providing informed consent. All participants continued to receive usual medical care throughout the intervention.
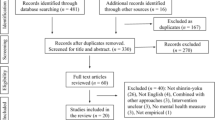
Participants were randomized according to the order of arrival, matching them by gender and fibromyalgia/non-fibromyalgia chronic pain. This RCT complied with the CONSORT (Consolidated Standards of Reporting Trials) guidelines, checklist, and flow diagram (see Fig. 1).
The sample consists of 50 subjects in the experimental group and 40 in the control group, with a mean age of 52 years. The majority are women, living in urban environments, 44% with fibromyalgia and 55% with other types of chronic pain (see Table 1). Nearly half consider they have fair health, and 75.6% have incomes below €2000 per month. There are no significant differences between the control and the experimental groups, except for their work status, since more patients in the control group were active at the time of performing the intervention and more subjects in the experimental group were unemployed.
Procedure
The treatment program was carried out at the social centers of the City Council of Vitoria between April and July 2019. All procedures contributing to this work were performed under the Helsinki Declaration of 1975, revised in 2008.
Participants were assessed by a general health psychologist (the last author) after being informed of the objectives of the study and giving informed consent to participate. Consenting participants were randomized to either the experimental or control group, and subsequently individually assessed in two sessions. Participants in the experimental group were evaluated following the assessment protocol at pre- and post-treatment (after attending the program), whereas controls were assessed at baseline and then three months later. During the wait-list period, they received the usual medical care, which consisted of taking analgesic drugs provided by their doctors. At the end of the wait-list period, they were offered the MBPM program.
The MBPM program consists of group sessions of two and a half hours (20 training hours in total), held weekly for eight weeks. The program focuses on training in awareness of physical, cognitive, and emotional sensations, attentional processes to become an observer of one’s thoughts and emotions, and non-judgmental acceptance, intending to provide greater flexibility to patients to manage pain. The program is fully described in Burch (2008). Covered topics include breath awareness, body scan, mindful movement, kindly awareness, and mindfulness in daily life. Table 2 summarizes the main characteristics of the MBSR and the MBPM.
As the original authors of the program summarize (Cusens et al., 2010, pp. 67–68):
Breath awareness begins with an inquiry into the full-body experience of breathing. A four-stage mindfulness of breathing meditation is subsequently introduced, which allows the mind to become focused on increasingly subtler aspects of the breath experience.
The body scan practice involves systematically moving awareness through each part of the body and noticing the presence of sensation in a detailed and precise way. This enables contact with the actual sensations of the body (as opposed to thoughts, ideas, or fears about these sensations).
Mindful movement involves bringing awareness to physical activity, thus allowing movement of the body within the limits of its physical capability. This is taught by means of a comprehensive sequence of movements based on yoga and Pilates.
“Kindly awareness” is a meditation practice concerned with the development of loving kindness. In the practice, there are five stages in which the individual brings a kindly attitude and intention to (1) themselves, (2) a friend, (3) someone in the periphery of the person’s life, (4) someone with whom there is a difficult relationship, and (5) all living things. Throughout each stage, awareness is brought to bear on shared experience and connectedness.
Mindfulness in daily life involves bringing awareness to ordinary, everyday life, including eating, sleeping, and habitual behavior. Attention is brought to the patterns of “boom and bust,” i.e., over-activity followed by a period of recovery and under-activity. These habits are addressed by means of a systematic, mindful approach to pacing (Cusens et al., 2010, pp. 67-68).
The course facilitator was a general health psychologist with expertise in mindfulness training and experience in treating patients with chronic pain, who in turn was supervised by the first two authors of the study.
All participants attended at least 80% of the group sessions, and they were also given: (1) Burch and Penman’s (2013) book; (2) a workbook with a summary of the sessions and homework; and (3) audio recordings of the meditations to practice at home. Participants were encouraged to develop a 30–45-min daily practice of formal meditation with audio recordings for guidance, together with 5–15 min of informal practices aimed to introduce mindfulness into daily life. Besides, weekly readings of Burch & Penman’s chapters were recommended to complement sessions and to be discussed with the group during the following sessions. Patients were encouraged to practice at home using a journal to register their practices, and all group sessions began with homework review.
Measures
Each participant was interviewed and asked to provide information about several demographic and pain-related variables, including age, civil status, work status, duration of pain, medications, family relations, and self-perceived health.
Lattinen Index (LI) (González-Escalada et al., 2012). It consists of five Likert-type subscales, which score from 0 to 4 for the following items: pain intensity, pain frequency, use of painkillers, degree of incapacity, and hours of sleep, besides a total score. The higher the score, the worse the assessment of the pain. The average score for the Spanish validation of the Lattinen Index is 11.73. Internal and temporal consistency analyses showed alpha coefficients of > 0.7 and an intraclass correlation coefficient of > 0.85, respectively.
Fibromyalgia Impact Questionnaire (FIQ) (Esteve et al., 2007). Only patients diagnosed with fibromyalgia completed this 10-item scale that assesses the impact of the disease on their daily activities. The first item is answered on a scale from 0 to 3, items two and three on a scale from 0 to 7, and the rest on a scale from 0 to 10. The global index is the arithmetic mean of the 10 items. The alpha coefficient is 0.82 in the Spanish validation, with a cutoff point of ≥ 59.
Chronic Pain Acceptance Questionnaire (CPAQ) (Spanish validation, González et al., 2010). It is a 20-item scale with scores ranging between 0 (never true) to 6 (always true), from which three scores are obtained: involvement in activities, openness to pain, and a total score. Alpha coefficients are 0.82 for activities and 0.75 for openness to pain.
Brief Symptom Check List (LSB-50) (De Rivera & Abuin, 2012; Abuin & De Rivera, 2014). It contains nine clinical scales (psychoreactivity, hypersensitivity, obsession-compulsion, anxiety, hostility, somatization, depression, sleep disturbance, expanded sleep disturbance), a psychopathological risk index, three global indexes (frequency of symptoms, intensity, and global impact), and two validity scales (minimization and magnification). It consists of 50 descriptive items on various psychological and psychosomatic symptoms. Higher scores indicate high levels of psychopathological distress. Alpha coefficients range from 0.79 to 0.90.
Health-Related Quality of Life, SF-12 Questionnaire (Ware et al., 1996; Spanish version, Schmidt et al., 2012). It is composed of 12 items that assess the degree of well-being and functional capacity, based on eight dimensions related to physical and mental health. Scores range from 0 to 100. The internal consistency is 0.63 for the physical dimension and 0.72 for the mental dimension. The higher the score, the higher the quality of life.
Inventory of Negative Thoughts in Response to Pain (INTRP) (Cano & Rodriguez, 2002). It assesses the presence of negative thinking in response to pain. It consists of 21 items distributed in five factors: general negative thoughts, negative social thoughts, disability, lack of control and self-blame, and a global score. Alpha coefficients range from 0.60 to 0.85.
Pain Catastrophizing Scale (PCS (Spanish version, Lami et al., 2013). This 13-item scale assesses thoughts and feelings about pain experiences. It consists of three subscales: rumination, magnification, and hopelessness. Each item is scored from 0 to 4, with scores ranging from 0 to 52. The internal consistency of the Spanish version is 0.94.
Spanish adaptation of the Connor-Davidson Resilience Scale (CD-RISC) (Crespo et al., 2014). It consists of 25 items, which are responded to on a scale from 0 (not at all) to 4 (almost always). The score ranges from 0 to 100 and the higher the score, the greater the resilience. The average score for a sample of caregivers to the dependent elderly suffering from chronic stress was 63.84 (SD = 14.61). Cronbach’s alpha was 0.89.
Finally, after finishing the treatment, experimental participants completed the Patient Satisfaction with Treatment Questionnaire (CSQ-8) (Larsen et al., 1979), which consists of eight items (five formulated positively and three negatively) related to the quality and satisfaction of the help received. These items are responded to on a Likert scale from 1 to 4. Internal consistency ranges from 0.86 to 0.94.
Data analyses
Statistical analysis was performed using the Statistical Package for Social Sciences (IBM SPSS version 25). Data were first explored using descriptive statistics: means and standard deviations for quantitative variables and frequencies and percentages for qualitative variables. Differences between the two groups were analyzed using a chi-square test for categorical variables and t-tests for independent measures. Kramer’s V and Cohen’s d were calculated to estimate the magnitude of the differences between groups. Finally, one-way ANOVA analyses and Bonferroni post hoc tests were used to compare participants with or without fibromyalgia.
Results
Dropouts: Differential Characteristics
Only one subject in the control group -with non-fibromyalgia chronic pain- did not complete the evaluation after three months on the waiting list, representing a dropout rate of 2.5%. However, of the 50 experimental participants, 10 did not finish the treatment, which represents a 20% dropout rate; six were fibromyalgia patients and four non-fibromyalgia chronic pain patients. Differential analysis was carried out between those patients in the experimental group who dropped out and those who finished the program, taking into consideration all the assessed variables (see Table 3). Dropouts were characterized by greater intensity of pain and magnification of symptoms, more interpersonal difficulties such as psychoreactivity, hypersensitivity, and hostility, and more anxiety and risk of psychopathology, with large effect sizes. At a cognitive level, they presented more negative thoughts and more feelings of self-blame and showed a worse mental-health-related quality of life and lower resilience. Thus, dropouts presented clinical features of greater psychological affectation than the subjects who complete the intervention program. This suggests that the type of intervention or its group format may not meet the psychological needs of this subgroup of patients, therefore requiring a more exhaustive study.
Between-Group Analysis
Before the intervention, there were no significant differences between the experimental and the control group in any of the variables, indicating that the groups were homogeneous. After the treatment, there were statistically significant differences between both groups in several variables, as mentioned above (see Table 4).
Regarding pain and its acceptance, the MBPM program managed to get patients to reduce the intensity level of pain, its frequency, and the use of analgesics, with moderate effect sizes. In addition, pain acceptance improved, showing greater involvement in daily activities, with moderate differences between control and experimental subjects. Likewise, in the case of participants with fibromyalgia, the program significantly alleviated the impact of this disease, evidenced by a significant reduction in the global score of the experimental subjects on the FIQ, with a moderate to large effect size.
Regarding psychopathology, the intervention allowed patients to reduce their global discomfort, the intensity of their symptoms, and their number, with large effect sizes. It also decreased psychoreactivity, hypersensitivity, levels of anxiety, depression, somatization, and hostility, with moderate to large effect sizes. The intervention also achieved an improvement in the participants’ perception of their mental-health-related quality of life. Regarding cognitive aspects, the intervention reduced automatic and self-blaming thoughts, as well as thoughts that amplify pain, with moderate to large effect sizes. Besides, participants felt more resilient and capable after receiving the MBPM. The patients expressed a high level of satisfaction with the intervention, with a mean of 29.67 (SD = 2.55) on the scale (range 8–32). Therefore, we can affirm that they consider the MBPM program useful and highly satisfactory.
However, the intervention failed to improve sleep quantity and quality, which is a challenge for the future. The program also was unsuccessful to reduce rumination or obsessive-type thoughts; considering the relationship, these processes have with negative emotional states, their treatment constitutes an area of work to consider.
Comparison of the Results of the MBPM Program on Fibromyalgia Versus Non-fibromyalgia Patients
To show whether the program had a differential impact on participants with or without fibromyalgia, we carried out one-way ANOVA analyses of dependent variables after the intervention, considering experimental vs. control participants with fibromyalgia and non-fibromyalgia chronic pain (see Table 5). Additionally, in those cases in which there were significant differences between the subgroups before the intervention, we carried out an ANCOVA taking into account pre-test measures as covariates (see Table 6).
As shown in Tables 5 and 6, most of the significant differences between subgroups are evident between the experimental group without fibromyalgia and the control group with fibromyalgia, among which the most extreme differences are observed. However, there are also significant differences between the experimental and control subgroups without fibromyalgia (a vs. c) in pain acceptance (involvement in activities and total score) and psychopathology (hostility, magnification, and intensity of symptoms), in favor of the experimental group. Between the experimental and control subgroups with fibromyalgia (b vs. d) differences are observed in psychopathology (anxiety, hostility, somatization, magnification, and intensity of symptoms), with no differences in other variables in favor of the MBPM program.
Therefore, patients with chronic pain without fibromyalgia obtain the best results. Experimental fibromyalgia patients compared to fibromyalgia control patients improve slightly in anxiety, hostility, somatization, and intensity of emotional symptoms, but not in variables such as pain management and acceptance or quality of life.
Discussion
The treatment of chronic pain constitutes a challenge from a healthcare point of view. Chronic pain puts an enormous burden on individuals and society and is often associated with psychopathology (Woo, 2010). Several non-pharmacological treatment alternatives can help manage chronic pain, such as mindfulness-based interventions, CBT, or Acceptance and Commitment Therapy, which are psychotherapies that can reduce the perception of pain, increase the quality of life, and reduce emotional symptomatology (Majeed et al., 2018). The objective of the present RCT was to determine the efficacy of the MBPM program (Cusens et al., 2010) for reducing pain, psychopathology, and negative thoughts, as well as improving the quality of life and resilience of patients with chronic pain.
The results showed moderate to large effects in favor of the experimental group in pain management and acceptance, use of analgesics, psychopathological symptoms, general negative thoughts, self-blame, mental-health-related quality of life, and resilience. These results are consistent with the studies reviewed by Hilton et al. (2017).
Although the results of the intervention are positive, further analyses considering the presence or absence of fibromyalgia warrant caution. Patients with fibromyalgia who received the MBPM program improved in emotional distress, anxiety, somatization, and magnification and intensity of symptoms, but not in pain management and acceptance or quality of life. Since the average benefits of CBT and other psychological therapies for FM are also modest (Glombiewski et al., 2010), treatments for this type of patient should be better tailored, perhaps by targeting risks factors that are not directly addressed by current therapies (Haugmark et al., 2019; Lauche et al., 2013; Lumley et al., 2017).
It should be noted that the intervention program is well accepted, the level of adherence is high (patients completed more than 80% of the sessions), and participants show high levels of satisfaction. However, there is a subgroup of patients characterized by greater intensity of pain, magnification of symptoms, more interpersonal difficulties, and hostility that left the therapeutic group. These patients could benefit from an individual approach or internet-delivered therapy (Boersma et al., 2019). In this sense, Henriksson et al. (2016) used an eight-week web-based mindfulness program adapted from the original MBPM (Cusens et al., 2010) that reduced pain intensity, pain-related interference/suffering, and affective distress, and heightened ratings of pain acceptance and life satisfaction in individuals with chronic pain, with medium to large effect sizes. This study further adds to prior evidence (e.g., Davis & Zautra, 2013; Gardner-Nix et al., 2008, 2014) that online mindfulness training in individuals with chronic pain conditions may show effects that rival those observed using the standard face-to-face format. The main challenge reported by the authors is related to the high rates of non-adherence to the home-based training (Henriksson et al., 2016), but this option should not be ruled out for those patients who do not feel comfortable with the group format.
Even though the MBPM program shows positive results, the intervention does not seem to have a large effect on sleep problems, rumination, and obsessive thoughts, factors frequently related to greater deterioration (Martínez et al., 2021). Therefore, these are significant variables to consider, and it seems necessary to add other therapeutic CBT elements to reduce sleep problems, need for control, and rumination (Glombiewski et al., 2010; Lami et al., 2018).
Limitations and Future Research
This study is not without limitations. First, the long-term efficacy of the program is still unclear due to the lack of follow-up, which makes it necessary to design further studies that evaluate whether the results obtained after applying the MBPM program are maintained in the long term and whether a continued practice of meditation would be necessary for this purpose. Regarding this, it would be of interest to use a measure of compliance with the at-home practice between sessions. Second, all the outcome measures were self-reported and did not include objective functional measures, deserving caution when interpreting the results. This may constitute method bias and lead to spurious effects (Podsakoff et al., 2012), so that future research should try to include non-subjective behavioral indices of change. Third, it is undeniable that a larger sample would have helped us to make stronger conclusions about the effects of the intervention on the fibromyalgia vs. non-fibromyalgia subgroups. It would have also allowed us to conduct analyses by gender or time since diagnosis. Fourth, despite having asked the participants about their level of global satisfaction about the program, no specific question was included about the components they found most useful, which would undoubtedly have been of interest for a more detailed assessment of the intervention. Finally, it should be noted that the efficacy of MBPM has been evaluated in comparison to a waiting list control group, so it would be interesting to include in future research an active control group, such as CBT, to compare the differential efficacy of both interventions.
Data Availability
All data to reproduce the analyses are available at the Open Science Framework: https://osf.io/kjwrb/#
References
Abuin, M. R., & De Rivera, L. (2014). La medición de síntomas psicológicos y psicosomáticos: El listado de síntomas breves (LSB-50). Clínica y Salud, 25, 131–141. https://doi.org/10.1016/j.clysa.2014.06.001
Boersma, K., Södermark, M., Hesser, H., Flink, I. K., Gerdle, B., & Linton, S. J. (2019). Efficacy of a transdiagnostic emotion-focused exposure treatment for chronic pain patients with comorbid anxiety and depression: A randomized controlled trial. Pain, 160, 1706–1718. https://doi.org/10.1097/j.pain.0000000000001575
Breivik, H., Collet, B., Ventafridda, V., Cohen, R., & Galagher, A. (2006). Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. European Journal of Pain, 10, 287–333. https://doi.org/10.1016/j.ejpain.2005.06.009
Brown, C. A., & Jones, A. K. (2013). Psychobiological correlates of improved mental health in patients with musculoskeletal pain after a mindfulness-based pain management program. Clinical Journal of Pain, 29, 233–244. https://doi.org/10.1097/AJP.0b013e31824c5d9f
Burch, V. (2008). Living well with pain and illness. The mindful way to free yourself from suffering. Piatkus
Burch, V., & Penman, D. (2013). Mindfulness for health. A practical guide to relieving pain, reducing stress and restoring wellbeing. Piatkus
Cano, F. J., & Rodriguez, L. (2002). Pensamientos automáticos negativos en el dolor crónico. Psiquis, 24, 137–145.
Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Lawrence Erlbaum Associates.
Cohen, J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. https://doi.org/10.1037//0033-2909.112.1.155
Crespo, M., Fernández-Lansac, V., & Soberón, C. (2014). Adaptación española de la escala de resiliencia de Connor-Davidson (CD-RISC) en situaciones de estrés crónico. Psicología Conductual, 22(2), 219–238.
Cusens, B., Duggan, G. B., Thorne, K., & Burch, V. (2010). Evaluation of the breathworks mindfulness-based pain management programme: Effects on well-being and multiple measures of mindfulness. Clinical Psychology and Psychotherapy, 17, 63–78. https://doi.org/10.1002/cpp.653
Davis, M. C., & Zautra, A. J. (2013). An online mindfulness intervention targeting socioemotional regulation in fibromyalgia: Results of a randomized controlled trial. Annals of Behavioral Medicine, 46(3), 273–284. https://doi.org/10.1007/s12160-013-9513-7
De Rivera, L., & Abuín, M. R. (2012). LSB-50. Listado de síntomas breve. TEA Ediciones
Díaz, M. I., Comeche, M. I., & Vallejo, M. A. (2003). Guía de tratamientos psicológicos eficaces en el dolor crónico (pp. 123–140). In M. Pérez, J. R. Fernández, C. Fernández & I. Amigo (Eds.). Guía de tratamientos psicológicos eficaces II. Psicología de la salud. Pirámide
Eccleston, C., & Crombez,G. (2017). Advancing psychological therapies for chronic pain. F1000Research, 6: 461. https://doi.org/10.12688/f1000research.10612.1
Ehde, D. M., Dillworth, T. M., & Turner, J. A. (2014). Cognitive-behavioral therapy for individuals with chronic pain. American Psychologist 69:153–166. https://psycnet.apa.org/doi/https://doi.org/10.1037/a0035747
Esteve, J., Rivera, J., Salvat, M. I., de Gracia, M., & Alegre de Miquel, C. (2007). Propuesta de una versión de consenso del Fibromyalgia Impact Questionnaire (FIQ) para la población española. Reumatología Clínica, 3, 21–24.
Gardner-Nix, J., Backman, S., Barbati, J., & Grummitt, J. (2008). Evaluating distance education of a mindfulness-based meditation programme for chronic pain management. Journal of Telemedicine and Telecare, 14(2), 88–92. https://doi.org/10.1258/jtt.2007.070811
Gardner-Nix, J., Barabati, J., Grummit, J., Pukal, S., & Raponi Newton, R. (2014). Exploring the effectiveness of a pain management course delivered to on-site and offsite patients using telemedicine. Mindfulness, 5, 223–231. https://doi.org/10.1007/s12671-012-0169-3
Glombiewski, J. A., Sawyer, A. T., Gutermann, J., Koenig, K., Rief, W., & Hofman, S. G. (2010). Psychological treatments for fibromyalgia: A meta-analysis. Pain, 151, 280–295. https://doi.org/10.1016/j.pain.2010.06.011
Gonzalez, A., Fernández, P., & Torres, I. (2010). Aceptación del dolor crónico en pacientes con fibromialgia: Adaptación del Chronic Pain Acceptance Questionnaire (CPAQ) a una muestra española. Psicothema, 22, 997–1003.
Gonzalez-Escalada, J. R., Camba, A., Muriel, C., Rodriguez, M., Contreras, D., & de Barutell, C. (2012). Validación del índice de Lattinen para la evaluación del paciente con dolor crónico. Revista Sociedad Española Del Dolor, 19, 181–188.
Haugmark, T., Birger, K., Smedslund, G., & Zangi, H.A. (2019). Mindfulness- and acceptance-based interventions for patients with fibromyalgia- A systematic review and meta-analyses. PloS One 14(9):e0221897. https://doi.org/10.1371/journal.pone.0221897
Henriksson, J., Wasara, E., & Rönnlund, M. (2016). Effects of eight-week-web-based mindfulness training on pain intensity, pain acceptance, and life satisfaction in individuals with chronic pain. Psychological Reports, 119(3), 586–607. https://doi.org/10.1177/0033294116675086
Hilton, L., Hempel, S., Ewing, B. A., Apaydin, E., Xenakis, L., Newberry, S., Colaiaco, B., Ruelaz, A., Shanman, R. M., Sorbero, M. E., & Maglione, M. (2017). Mindfulness meditation for chronic pain: Systematic review and meta-analysis. Annals of Behavioral Medicine, 51, 199–213. https://doi.org/10.1007/s12160-016-9844-2
Kabat-Zinn, J. (1982). An outpatient program in behavioral medicine for chronic patients based on the practice of mindfulness meditation. Theoretical considerations and preliminary results. General Hospital Psychiatry, 4, 33–47. https://doi.org/10.1016/0163-8343(82)90026-3
Kabat-Zinn, J. (1990). Full catastrophe living. Using the wisdom of your body and mind to face stress, pain, and illness. Delacorte Press
Kabat-Zinn, J., Lipworth, L., & Burney, R. (1985). The clinical use of mindfulness meditations for the self-regulation of chronic pain. Journal of Behavioral Medicine, 8(2), 163–190. https://doi.org/10.1007/bf00845519
Khoo, E. L., Small, R., Cheng, W., Hatchard, T., Glynn, B., Rice, D. B., Skidmore, B., Kenny, S., Hutton, B., & Poulin, P. A. (2019). Comparative evaluation of group-based mindfulness-based stress reduction and cognitive behavioural therapy for the treatment and management of chronic pain: A systematic review and network meta-analysis. Evidence Based Mental Health, 22, 26–35. https://doi.org/10.1136/ebmental-2018-300062
Khoury, B., Kanauper, B., Schlosser, M., Carriere, K., & Chiesa, A. (2017). Effectiveness of traditional meditations retreats: A systematic review and meta-analysis. Journal Psychosomatic Research, 92, 16–25. https://doi.org/10.1016/j.jpsychores.2016.11.006
Lami, M. J., Martínez, M. P., Miró, E., & Sánchez, A. I. (2013). Versión española de la escala de catastrofización del dolor: Estudio psicométrico en mujeres sanas. Psicología Conductual, 21(1), 137–156.
Lami, M. J., Martínez, M. P., Miró, E., Sánchez, A. I., Prados, G., Cáliz, R., & Vlaeyen, J. W. S. (2018). Efficacy of combined cognitive-behavioral therapy for insomnia and pain in patients with fibromyalgia: A randomized controlled trial. Cognitive Therapy and Research, 42, 63–79. https://doi.org/10.1007/s10608-017-9875-4
Larsen, D. L., Attkisson, C. C., Hargreaves, W. A., & Nguyen, T. D. (1979). Assessment of client/patient satisfaction: Development of a general scale. Evaluation and Program Planning, 2, 197–207. https://doi.org/10.1016/0149-7189(79)90094-6
Lauche, R., Cramer, H., Dobos, G., Langhorst, J., & Schmidt, S. (2013). A systematic review and meta-analysis of mindfulness-based stress reduction for the fibromyalgia syndrome. Journal of Psychosomatic Research, 75, 500–510. https://doi.org/10.1016/j.jpsychores.2013.10.010
Lledó, A., Pastor, M. A., & López-Roig, S. (2013). Intervención psicológica en la fibromialgia. FOCAD. Consejo General de la Psicología de España
Lumley, M. A., Schubiner, H., Lockhart, N. A., Kidwell, K. M., Harte, S. F., Clauw, D. J., & Williams, D. A. (2017). Emotional awareness and expression therapy, cognitive behavioural therapy and education for fibromyalgia: A cluster randomized controlled trial. Pain, 158, 2354–2363. https://doi.org/10.1097/j.pain.0000000000001036
Majeed, M. H., Ali, A. A., & Sudak, D. M. (2018). Mindfulness-based interventions for chronic pain: Evidence and applications. Asian Journal of Psychiatry, 32, 79–83. https://doi.org/10.1016/j.ajp.2017.11.025
Martínez, M. P., Sánchez, A. I., Cáliz, R., & Miró, E. (2021). Psychopathology as a moderator of the relationship between physical symptoms and impairment in Fibromyalgia Patients. Psicothema, 33, 214–221. https://doi.org/10.7334/psicothema2020.338
Naylor, Ch., Parsonage, M., McDaid, D., Knapp, M., Fossey, M., & Galea, A. (2012). Long-term conditions and mental health. The cost of co-morbidities. The King’s Fund. www.kingsfound.org.uk
Pastor, M. A., Lledó, A., López-Roig, S., Pons, N., & Martín, M. (2010). Predictores de la utilización de recursos sanitarios en la fibromialgia. Psicothema, 22, 549–555.
Podsakoff, P. M., MacKenzie, S. B., & Podsakoff, N. P. (2012). Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology, 63, 539–569. https://doi.org/10.1146/annurev-psych-120710-100452
Porter-Moffitt, S., Gatchel, R. J., Robinson, R. C., Deschner, M., Posamentier, M., Polatin, P., & Lou, L. (2006). Biopsychosocial profiles of different pain diagnostic groups. The Journal of Pain, 7(5), 308–318. https://doi.org/10.1016/j.jpain.2005.12.003
Schmidt, S., Vilagut, G., Garin, O., Cunillera, O., Tresserras, R., Brugulet, P., Mompart, A., Medina, A., Ferrer, M., & Alonso, J. (2012). Normas de referencia para el cuestionario de salud SF-12 versión 2 basados en población general de Cataluña. Medicina Clínica, 139(14), 613–625. https://doi.org/10.1016/j.medcli.2011.10.024
Van Gordon, W., Shonin, E., & Griffiths, M. D. (2015). Towards a second-generation of mindfulness-based interventions. Australia and New Zealand Journal of Psychiatry, 49, 591. https://doi.org/10.1177/0004867415577437
Ware, J. R., Kosinski, M., & Keller, S. D. (1996). A 12-item short-form health survey: Construction of scales and preliminary test reliability and validity. Medicine Care, 34, 220–233. https://doi.org/10.1097/00005650-199603000-00003
Woo, A. K. (2010). Depression and anxiety in pain. British Journal of Pain, 4, 8–12. https://doi.org/10.1177/204946371000400103
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. Open access provided by the University of the Basque Country.
Author information
Authors and Affiliations
Contributions
JIPF and KS: designed the study, wrote the protocol, carried out the statistical analyses, conducted the literature search, and wrote the first draft of the manuscript. ARO: implemented the intervention program and performed the assessments. All authors contributed to and have approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
All procedures performed in this study adhere to the ethical standards of the 1964 Helsinki Declaration and its later amendments or comparable ethical standards and were approved by the Ethics Committee of the Department of Health of the Basque Government (CEIm-E) in December of 2018 (PI2018162).
Consent to Participate
Informed consent was obtained from all participants included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pérez-Fernández, J.I., Salaberria, K. & Ruiz de Ocenda, Á. Mindfulness-Based Pain Management (MBPM) for Chronic Pain: a Randomized Clinical Trial. Mindfulness 13, 3153–3165 (2022). https://doi.org/10.1007/s12671-022-02023-1
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-022-02023-1