Abstract
Objectives
The objective of this systematic review and meta-analysis was to examine controlled trial evidence for the effectiveness of mindfulness-based interventions on stress, anxiety and depression in the perinatal period in women without pre-existing mental health issues.
Methods
Six databases were searched for studies exploring the effects of mindfulness-based interventions on mental health outcomes of women during the perinatal period. Quality of both controlled trial meeting inclusion criteria were assessed using a tool specifically designed for meta-analyses of mindfulness-based interventions. Effect sizes were extracted for measures of mindfulness, depression, stress and anxiety outcomes. Effects were pooled in separate meta-analyses for all outcomes except anxiety which lacked sufficient studies.
Results
Twelve studies were analysed. Pooled effects suggest that mindfulness-based interventions cause small but clear increases in mindfulness and reductions in depression in women without pre-existing disorders. Effects of mindfulness-based interventions on other outcomes were unclear and confounded by heterogeneity.
Conclusions
Available controlled trial evidence suggests that mindfulness-based interventions improve mindfulness and decrease symptoms of depression during pregnancy in women without pre-existing mental health issues and might be a useful approach to prevent or attenuate the development of depression in the perinatal period.
Similar content being viewed by others
Pregnancy, childbirth and the postnatal period are times of immense physical and emotional change (Cowan, 1991). The transition to motherhood can be stressful, increasing vulnerability to anxiety and depression (Grote & Bledsoe, 2007). Mental health issues are prevalent at this time, with around 1 in 5 women experiencing depression during pregnancy and in the postnatal period (Dhillon et al., 2017; Fairbrother et al., 2015; NICE, 2014). Stress has been found to affect 58% of pregnant women (Stone et al., 2015). Stress and depression during the perinatal period are predictive of short- and long-term negative consequences for mothers and infants (Staneva et al., 2015). Mental health issues during pregnancy have been associated with an increase in the risk of premature and stillbirths (Dunkel Schetter, 2011; Webb et al., 2005) and congenital malformations (Pereira et al., 2011). Maternal mental health issues are also associated with greater risk of the baby going on to develop behavioural and emotional problems in later life, with increased risk of a negative impact on IQ and educational attainment (Stein et al., 2014). Prompt and effective treatment not only minimises the risks for the mother, but also minimises the risks to her child’s emotional, social and cognitive development (National Collaborating Centre for Mental Health, 2018). Perinatal stress is also known to increase the use of analgesia and the risk of surgical/caesarean deliveries and post-partum depression (Saeed et al., 2015; Saunders et al., 2006; Togher et al., 2017). Moreover, suicide continues to be a leading cause of maternal death in the UK (Knight et al., 2015). Given this context, preventing or attenuating stress, anxiety and depression during pregnancy is a crucial public health goal (Cooper & Murray, 1998). The need to establish pathways for effective prevention and treatment of maternal mental health issues has driven substantial government funding into maternal mental health care in England. There are plans to provide evidence-based mental health care in the perinatal period for 30,000 women in England (Maruthappu et al., 2014). As the perinatal period (pregnancy and a year postnatally) is considered a time of increased risk for mental health issues in women (National Maternity Review, 2016), NHS resources are being directed to strategies that are effective for detecting and preventing mental health issues during the perinatal period. Given that prevention is a key public health agenda, the optimal target population for interventions aimed at preventing the development of mental health issues is women without pre-existing mental health disorders (Woolhouse et al, 2014). This is the scope of this review.
The management of mental health problems that develop during pregnancy and the postnatal period presents unique challenges. There are risks associated with taking psychotropic medication in pregnancy and during breastfeeding (NICE, 2016). Given the importance of preventing and managing mental health issues in the perinatal period, and the difficulties associated with medication, mindfulness-based interventions are a potential solution for supporting women during this period. Attending a mindfulness-based intervention has also been described as enabling flexibility in choice during childbirth, with this contributing to positive experiences (Fisher et al., 2012). Kabat-Zinn (2013) described mindfulness as ‘paying attention in a particular way: on purpose, in the present moment, and non-judgmentally’. He outlined nine attitudes underlying mindfulness as beginner’s mind, non-judging, acceptance, letting go, trust, patience, non-striving, gratitude and generosity (Kabat-Zinn, 2019). These attitudes are the foundation of mindfulness-based interventions. Mindfulness teachers are trained to develop an awareness of these attitudes within their mindfulness practice and in delivering mindfulness-based interventions (Crane et al., 2017). Kabat-Zinn (2013) originally developed mindfulness-based stress reduction (MBSR), with mindfulness-based cognitive therapy (MBCT) being developed as a relapse prevention approach for depression (Segal et al., 2013). Mindfulness-based interventions have flourished since their inception in the 1980s, with evidence for their effectiveness with anxiety, depression, stress, managing chronic physical conditions and suicidality (Hofmann & Gómez, 2017; Kuyken et al., 2016; Williams & Swales, 2017; Zhang et al., 2015). Increasing capacity to be aware of and accept situations, thoughts and feelings as they are can lead to greater tolerance of stress and discomfort (Kashdan & Rottenberg, 2010; Warriner et al., 2018). The perinatal period is a time when such skills and attitudes may benefit women through reducing the effects of the stressors involved in this transition.
Previous systematic reviews of mindfulness-based interventions in the perinatal period have included both pre-post and RCT studies, some of which sample from populations of women with pre-existing mental health disorders and others that sample from populations of women without pre-existing disorders. Previous systematic reviews have found some evidence from pre-post studies of reductions in stress, anxiety and depression, but no significant benefit in RCTs (Hall et al., 2016). In agreement with Hall et al. (2016), Lever Taylor et al. (2016) found small to moderate benefits for depression, anxiety, stress and mindfulness from pre-post studies. Larger effect sizes were found for studies on participants with pre-existing, or a history of, depression, anxiety and stress, suggesting, in agreement with Woolhouse et al. (2014), that such participants form a separate study population from participants without pre-existing disorders. Between group comparisons from RCTs again showed no significant benefits for depression, anxiety, stress and mindfulness. The most recent systematic review and meta-analysis found no significant differences between the intervention and control groups for anxiety, depression and perceived stress, with mindfulness being the only outcome variable with a significant between-group difference (Dhillon et al., 2017). Similar to preceding meta-analyses, Dhillon et al. (2017) found significant benefits in pre-post studies for anxiety, depression, perceived stress and mindfulness.
Given contrasting evidence from pre-post versus controlled trials, and acknowledging the inherent bias in, and inability to claim causal effects from, pre-post studies, previous meta-analyses have concluded that additional large-scale, adequately powered, randomised controlled trials are needed to evaluate the effectiveness of mindfulness-based interventions (Dhillon et al., 2017; Hall et al., 2016; Lever Taylor et al., 2016; Matvienko-Sikar et al., 2016; Shi & MacBeth, 2017). This recommendation has also been motivated by high degrees of heterogeneity reported in previous reviews. In response to these recommendations, there have been several studies published since Dhillon et al. (2017).
A source of heterogeneity that does not seem to have been addressed in previous meta-analyses is the pooling together of studies that have sampled from populations with and without pre-existing mental health disorders. Given the large difference in effects from studies on women with and without pre-existing conditions reported by Lever Taylor et al. (2016), it is surprising that subsequent meta-analyses have not sought to examine these populations separately. There is currently no pooled effect size estimate for the benefits of mindfulness interventions in women without pre-existing mental health issues that is not currently clouded by the effects on women that begin mindfulness interventions with pre-existing mental health disorders. Given the inherent bias of pre-post studies, and the absence of pooled evidence for the causal effects of mindfulness interventions on health in women without pre-existing conditions, a systematic review and meta-analysis of controlled trials conducted only on women without existing mental health issues is required. A review of RCT evidence from women without pre-existing mental health disorders is the only way to examine the possible preventative benefits of mindfulness interventions during pregnancy.
Existing meta-analyses examining the efficacy of mindfulness interventions on mental health outcomes in the perinatal period have combined studies sampling from populations with and without pre-existing disorders. The pooling of sample populations prevents a clear summary of the possible preventative benefits of mindfulness interventions for women without pre-existing stress, anxiety or depression. Moreover, existing summaries of evidence and recommendations are confounded by the inclusion of weak and conflicting evidence from pre-post studies. Therefore, the aim of this systematic review and meta-analysis is to provide an up-to-date evaluation of controlled trial evidence for the efficacy of mindfulness-based interventions to attenuate anxiety, depression and stress in the perinatal period in women without pre-existing depression, stress or anxiety disorders.
Methods
Search Strategy and Study Selection
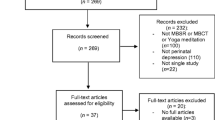
We conducted the review according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Hutton et al., 2015). The content of six databases (Cochrane Library, Web of Science, PsycArticles, MEDLINE and PubMed, CINAHL and Scopus) was searched from inception to 4th April 2020. The databases were chosen due to comprehensive data coverage and their use in previous meta-analyses (Dhillon et al., 2017; Lever Taylor et al., 2016). The following search terms were applied and were based on search strings used in previous systematic reviews in this area: Mindful* OR MBCT OR MBSR AND prenatal OR antenatal OR postnatal OR post-partum OR puerperal OR pregnancy OR pregnant OR trimester OR childbirth.
The search was restricted to peer-reviewed studies written in English and available in full text. Only quantitative controlled trials exploring the effectiveness of a mindfulness-based intervention during the perinatal period (i.e. during pregnancy or the first year following childbirth) were included. A mindfulness-based intervention was defined as mental practice to promote a structured mind set to being aware of the present-moment experience in an accepting, non-judging and non-avoiding way (Kabat-Zinn, 2013). Practices falling under this definition include MBCT, MBSR, ACT, mindfulness-based yoga or other interventions described by the authors. Included studies also needed to include a control group and measures at baseline and after the intervention using validated measures of depression, anxiety, stress and/or mindfulness. No other methodological requirements were set, but study quality was rated.
We included studies if they were available at any time before the date of the search.
Articles from the search were tracked and a further search of potentially relevant articles and review papers in the reference sections was conducted. Duplicates were removed and the remaining studies were further screened by title, abstract and full text. Irrelevant articles were excluded. Inclusion or exclusion decisions were based on the judgment of two independent researchers. Any discrepancies were resolved through discussion.
Inclusion Criteria
In accordance with the PICOS approach (population (P), intervention (I), comparators (C), main outcome (O) and study design (S)), the following inclusion criteria were used:
Participants were pregnant females (P); studies had to include mindfulness-based interventions (as defined above) delivered during the perinatal period (i.e. during pregnancy of the first year after birth) (I); passive-inactive, alternative-active or usual-care control groups not receiving mindfulness interventions were acceptable controls (C); validated quantitative measures of mindfulness, state and/or trait anxiety, stress and depression constituted the outcome measures (O); and only controlled trials (both randomised and non-randomised) were included (S).
After removal of duplicates, 870 papers were screened by abstract. Subsequently, 29 full-text papers were reviewed and 12 met the criteria for inclusion (Fig. 1).
Quality Assessment
Studies were evaluated using a tool developed specifically for a large-scale meta-analysis of mindfulness-based interventions (Khoury et al., 2013). This tool was chosen due to its ability to assess both randomised and non-randomised designs and the inclusion of items specific to the validity of tools used to measure mindfulness, the mindfulness protocol and the training of the therapists to deliver mindfulness interventions (Khoury et al., 2013). The quality scoring tool included items from the Jadad et al. (1996) scale and items not specific to controlled studies. The items assessed by the tool included the following: (1) whether the intervention followed a clearly described protocol based on, or adapted from, an established programme (score of 0 or 1); (2) whether measures were administered at follow-up (score of 0 or 1); (3) whether a validated measure of mindfulness was used (score of 0 or 1); (4) whether therapists were trained in delivering mindfulness-based interventions and (for studies with clinical populations only) were clinically trained based on good practice guidelines for teaching mindfulness-based courses (UK mindfulness-based teacher trainer network, 2015). Mindfulness training was required for any study to obtain a score of 1, but clinical training was only required for studies including clinical populations (score of 0 or 1); (5) whether the study was randomised (score of 0 if not randomised, 1 if randomised with a no intervention/waitlist control, 2 if randomised with a usual-care control and 3 if randomised with an active control); and (6) whether investigators and/or participants were blinded to their allocated condition (score of 0 if not blinded, 1 if single-blinded, 2 if double-blinded). The maximum score from the scale was 9, with higher scores reflecting studies of higher quality. Two independent researchers completed the quality assessments. As with study inclusion, discrepancies were resolved through discussion.
Data Extraction and Analysis
Participant characteristics, demographic data, type and characteristics of intervention, type of control/comparison group, outcome measures and effect sizes for post-intervention difference between intervention and control groups were extracted.
Effect size was calculated as Cohen’s d using the mean difference and pooled SD when reported. Where SD was not reported, it was calculated either from the reported exact p values or from t or F statistics using formulas provided in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al., 2021). Studies not reporting the statistics required to calculate effect size as described were excluded from the analysis.
We extracted only composite scores from mindfulness questionnaires with subscales. Where multiple scales were used to assess depression, the Edinburgh Postnatal Depression Scale (EPDS) (Cox & Holden, 1987) was used in line with other meta-analyses in this area (Lever Taylor et al., 2016; Sockol, 2015;). The EPDS is the most frequently used self-report measure of perinatal depressive symptom severity with strong psychometric properties amongst both pregnant and post-partum samples (Cox & Holden, 1987; Murray & Carothers, 1990). For other outcomes (i.e. anxiety and stress) and in cases where the EPDS was not used to assess depression, but more than one scale was used to measure the construct, the scale with the strongest psychometric properties was used to calculate effect size. Where more than one scale was used to measure the construct, and there was no clear evidence for superiority of one scale over another based on psychometric properties, a weighted mean effect size was calculated to ensure only a single effect size estimate from each study sample (Lipsey & Wilson, 2001, p. 114).
For meta-analysis, random effects models were run in JASP (version 0.14.1). Tables and forest plots were produced for each outcome, and heterogeneity was assessed using the Q statistic and I2 statistic. The I2 statistic was interpreted against the following categories from the Cochrane Handbook for Systematic Reviews of Interventions (Higgins et al., 2021): 0–40% not important; 30–60% moderate; 50–90% substantial; and > 75–100% considerable heterogeneity. Influential case analyses and funnel plots were used to identify outliers and examine publication bias, respectively. Influential cases were identified by a Cook’s distance value of > 0.5 (Viechtbauer & Cheung, 2010). If outliers were identified, they were removed and the analysis was repeated.
Results
Study Characteristics
A summary of studies included for analysis is shown in Table 1. There were 704 participants across the 12 included studies with 635 involved in RCTs and the remaining 69 from non-RCTs. Demographic data from study participants are summarised in Table 2. Of these studies, only Chan (2015) used an intervention not based on an established mindfulness programme. Three RCTs did not measure mindfulness as an outcome of the intervention (Chan, 2015; Muthukrishnan et al., 2016; Zhang et al., 2019). One study examined the impact of a mindfulness-based intervention on outcomes after birth (Perez-Blasco et al., 2013). The remaining RCTs focused on reducing general distress or anxiety or improving wellbeing during the pregnancy period in samples not recruited for elevated baseline measures of depression, stress and anxiety.
There were two non-randomised control trials in the included studies. Bowen et al. (2014) did not explain how participants were allocated to the mindfulness-based intervention or the alternative interpersonal therapy active control groups. Gambrel and Piercy (2015) used a waiting-list control for comparison, with a primary aim of examining the effects of a mindfulness-based intervention during the pregnancy period on relationship satisfaction. Nevertheless, quantitative data were reported for outcomes of interest to this review for the pregnant females separately. Bowen et al. (2014) sought to examine the effects of a mindfulness-based intervention versus interpersonal therapy on depression and worry symptoms in pregnant, anxious and depressed participants.
Across the 12 included studies, the duration of interventions ranged from 4 to 8 weeks, with most delivering approximately eight 2–3 h weekly sessions albeit with some variability between studies. No study explicitly followed the MBCT course structure. The remaining studies mostly used variations or adaptations of MBCT, though two studies delivered bespoke programmes that contained mindfulness elements including: Eastern-based meditation (Chan, 2015) and mindful transition to parenthood (Gambrel & Piercy, 2015). Where reported, the duration of instructor-led and home-practice sessions was generally less than recommended in MBSR or MBCT (see Table 1).
Quality Assessment of Included Studies
Scores on the quality assessment ranged from 3 to 7 out of a possible 9, with a mean score of 4.9, a median of 5 and a modal score of 4. Quality scores were generally reduced by a lack of trained mindfulness practitioners delivering interventions, failure/inability to blind participants and researchers to the allocated conditions, failure to specify the random allocation process and not including an assessment of mindfulness. Assessment scores for all included studies are shown in Table 3.
Intervention Effects
Of the 12 studies included, 11 reported group comparison data for at least one measure of depression (total n = 607), 7 for stress (total n = 403) and 8 for mindfulness (total n = 396). Only 3 studies included measures of general anxiety (total n = 81).
General Anxiety
The effect sizes for anxiety reduction differences between intervention and control groups at post-test ranged from d = − 0.04, d = − 0.25 and d = − 1.23 from Woolhouse et al. (2014), Bowen et al. (2014) and Perez-Blasco et al. (2013), respectively. Because of the small number of, and a large variation in reported effects on general anxiety, a meta-analysis was not performed on this outcome. Perez-Blasco et al. (2013) delivered the mindfulness intervention in the post-partum period with a sample of breastfeeding women. The difference in intervention period could be a factor in the larger reduction observed in that study.
Depression
There was a small and statistically significant reduction in depression after mindfulness interventions compared with controls. The effect size estimate for the intervention-control post-test difference was d = − 0.20 (95% CI, − 0.40, − 0.00, p = 0.04). Moreover, estimates of heterogeneity were statistically non-significant and indicated unimportant between-study variation in effect sizes (Q10 = 11.1, p = 0.35, I2 = 23.1%). There were no influential cases and no indication of publication bias. Figures 2 and 3 display a forest plot and funnel plot respectively for the depression outcome.
Mindfulness
There was a small, statistically significant increase in mindfulness after mindfulness interventions compared with controls. The effect size estimate for the intervention-control post-test difference was d = 0.24 (95% CI, 0.04, 0.43, p = 0.02). Heterogeneity estimates were small and statistically non-significant (Q7 = 6.52, p = 0.48, I2 = 0.01%). There were no influential cases and no indication of publication bias. Figures 4 and 5 display a forest plot and funnel plot respectively for improvement in mindfulness.
Stress
Influence analysis suggested that the unusually large effect size for stress reduction reported by Muthukrishnan et al. (2016) was a clear outlier. After removal of this effect from the analysis, the evidence of the remaining 6 studies estimated a small but statistically non-significant reduction in stress after mindfulness interventions compared with controls. The effect size estimate for the intervention-control post-test difference was d = − 0.21 (95% CI, − 0.59, 0.16, p = 0.27). Heterogeneity statistics were statistically non-significant but suggestive of moderate heterogeneity in the remaining 6 studies (Q5 = 10.5, p = 0.06, I2 = 54.2%). There was no indication of publication bias. Figures 6 and 7 display a forest plot and funnel plot respectively for the stress outcome. Other than lack of evidence for the training of the mindfulness instructors, there were no obvious aspects of the methods used by Muthukrishnan et al. (2016) that could account for the large reduction in stress reported in that study.
Discussion
This systematic review and meta-analysis has sought to provide an up-to-date summary of controlled trials on the effectiveness of mindfulness-based interventions in the perinatal period for reducing stress, anxiety and depression in women without pre-existing stress, anxiety or depression disorders. The analysis included 12 studies comprising 10 randomised and 2 non-randomised controlled trials on this population of women.
There was evidence to suggest that mindfulness interventions result in small, but clear and statistically significant reductions in depression and increases in mindfulness in participants without pre-existing disorders. The evidence for reductions in anxiety and stress was limited and unclear. There were insufficient and highly variable effects for anxiety reduction, and non-significant effects for stress reduction, with potentially problematic heterogeneity in the findings.
Studies were evaluated using a tool developed specifically for a large-scale meta-analysis of mindfulness-based interventions (Khoury et al., 2013). The maximum possible score of 9 would indicate studies of the highest quality in this field of research. The included studies were, on average, of moderate quality despite all being controlled trials. The failure/inability to blind participants to their allocated condition is understandable given the nature of mindfulness interventions; however, it is possible to blind researchers to the allocation, though this was not generally reported. The lack of trained mindfulness practitioners in the delivery of mindfulness interventions is possibly more problematic. Evidence of appropriate training was lacking in 4 of the included studies. There was also considerable variation in the mindfulness-based interventions used, with only one study explicitly following MBCT course structure. The well-established approaches of mindfulness-based cognitive therapy and mindfulness-based stress reduction are adapted in multiple ways, potentially providing different mechanisms for change across studies and accounting for variability and magnitude of effects.
Stress and anxiety effects were confounded by heterogeneity. Even after removal of an outlier, the I2 statistic suggested moderate to problematic heterogeneity in the remaining studies. Though the Q statistic was not significant for the stress outcome, the small number of remaining studies could result in insufficient power to reject the null hypothesis in this test. Meta-analysis was not performed on the anxiety outcome as there were only three studies. Nevertheless, the variation in effect sizes between these three studies was notable and ranged from very small to very large. Even for depression and mindfulness outcomes, the pooled analyses combine relatively small numbers of studies. As such, caution should possibly be exercised in the interpretation of pooled effects, though the non-significant and very low heterogeneity for mindfulness and non-significant and low heterogeneity for depression might provide some reassurance. Potential sources of heterogeneity include length and number of intervention sessions and different tools for measuring outcomes. Studies have also been carried out in different countries with the potential for cultural influences on intervention delivery and effectiveness, though these effects are speculative and beyond the scope of this review to examine. There were also considerable study design limitations, such as small sample sizes, lack of formal sample size estimation and specification of practical/clinically meaningful effects sizes and subsequently, unspecified type two error rates. Studies also often had many outcome measures/hypotheses being tested. Such issues inflate standard error in individual studies and subsequently in the pooled effect size estimate and challenge meta-analysis outcomes (Mayo-Wilson et al., 2017).
This review examined only controlled trials on women without pre-existing mental health issues. The goal was to obtain estimates of the effects of mindfulness interventions in mentally healthy women, free from the bias introduced by samples of women belonging to a population with existing mental health issues. As such, comparisons with previous meta-analyses that pooled samples from populations both with and without mental health disorders may be of limited value. However, our analysis of controlled trials provided no evidence of benefit of mindfulness-based interventions on anxiety and stress, supporting the findings of previous reviews (Dhillon et al., 2017; Lever Taylor et al., 2016). The heterogeneity of these outcomes was also in agreement with the previous analyses, despite our studies being only from the population of women without pre-existing disorders. In contrast to both previous reviews, however, our estimated effect on depression suggested a clear albeit small reduction in depression compared to controls after mindfulness interventions. The pooled effect on depression was unclear/non-significant in the previous two meta-analyses of this topic. In agreement with Dhillon et al. (2017), we found clear evidence for increased mindfulness after mindfulness-based interventions from controlled trials, though the size of effect was smaller in our analysis than previously reported. Lever Taylor et al. (2016) reported similar effect sizes to ours that were non-significant for controlled trials and with significant heterogeneity. The contrast in finding between our review and previous reviews, and the difference in effect size magnitude where findings agreed, could be explained by the single focus on studies from the population of women without pre-existing mental health disorders in this review. It is likely that removing studies on women with existing conditions reduced heterogeneity and allowed for a clearer estimate of the effect size of interest in this review.
Limitations and Future Research
The specific focus on controlled trials and studies of women without pre-existing conditions meant that the pool of studies in this meta-analysis is smaller than previous meta-analyses. However, this volume-quality trade off was required to address the research question.
We performed this review in accordance with PRISMA guidelines (Hutton et al., 2015). To our knowledge, this is the first up-to-date systematic review and meta-analysis of controlled trials on the effectiveness of mindfulness-based interventions on mental health outcomes during pregnancy performed solely in women without pre-existing stress, anxiety or depression. One aspect of the method that could have been strengthened was the approach to quality assessment. Two independent researchers assessed study quality, but inter-rater reliability of scores was not formally calculated. Such formal calculations are, however not often reported in other reviews in this field. The limitations of this review are primarily due to the volume and quality of the studies included. Some studies failed to report effect sizes or statistics from which effect size could be calculated in the results. Several studies included more than one psychometric measure of an outcome variable. Weighted average effect sizes were calculated where psychometric properties of the multiple tools could not differentiate. However, this does not address the issue of multiple and unnecessary hypothesis tests being conducted in the original studies. Such practices are known to inflate type 1 error rate, a problem that, in combination with underpowered studies, further confounds meta-analysis in this field of study. Furthermore, and despite the homogeneity of the outcome for mindfulness and depression, the relatively small number of studies analysed should be considered when interpreting the findings.
Future research should define clinically-meaningful effects for intervention studies using mindfulness. Future studies should limit the number of measurement tools and, where possible, choose single tools with good psychometric properties to assess variables of interest. Future studies should also simplify their designs to use the smallest number of samples of sufficient size to detect a clinically meaningful effect in mental health variables of interest. It would also be of value to explore if the benefits of a mindfulness-based intervention are maintained in the postnatal period, building on the few studies available in this area. In general, and in agreement with the recommendation of the previous meta-analyses on the topic, there is a need for more well-designed, controlled trials with trained mindfulness practitioners and established interventions performed on women without pre-existing stress, anxiety or depression. Moreover, a meta-analysis of controlled trials including only studies on women with pre-existing depression, stress and anxiety disorders is warranted given that different and clearer effects sizes appear when analyses separate studies on women with and without pre-existing conditions.
This study suggests that mindfulness-based interventions cause small reductions in depression and small increases in mindfulness in women without pre-existing disorders. If the cost of offering mindfulness-based interventions is not prohibitive, such interventions could be a useful addition to existing support for pregnant women without existing mental health issues and could serve to prevent or attenuate the development of depression symptoms during the perinatal period. There remains a need for robust controlled trials with clear hypotheses and parsimonious designs.
References
Studies included in the meta-analysis are marked by an (*)
*Beattie, J., Hall, H., Biro, M.A., East, C., & Lau, R. (2017). Effects of mindfulness on maternal stress, depressive symptoms and awareness of present moment experience: a pilot randomised trial. Midwifery, 50, 174-183
*Bowen, A., Baetz, M., Schwartz, L., Balbuena, L., & Muhajarine, N. (2014). Antenatal group therapy improves worry and depression symptoms. Israeli Journal of Psychiatry Related Science, 51(3), 226-231
*Chan, K. (2015). Effects of perinatal meditation on pregnant Chinese women in Hong Kong: a randomised controlled trial. Journal of Nursing Education and Practice, 5(1), 1-18
Cooper, P. J., & Murray, L. (1998). Postnatal depression. British Medical Journal, 316(7148), 1884–1886.
Cox, J. L., & Holden, J. M. (1987). Detection of postnatal depression. Development of the 10-item Edinburgh Postnatal Depression Scale. British Journal of Psychiatry, 150, 782–786.
Cowan, P. H. (1991). Family transitions. Lawrence Erlbaum.
Crane, R. S., Brewer, J., Feldman, C., Kabat-Zinn, J., Santorelli, S., Williams, J. M. G., & Kuyken, W. (2017). What defines mindfulness based programmes? The warp and the weft. Psychological Medicine, 47(6), 990–999.
Dhillon, A., Sparkes, E., & Duarte, R. V. (2017). Mindfulness-based interventions during pregnancy: A systematic review and meta-analysis. Mindfulness, 8, 1421–1437.
*Duncan, L.G., Cohn, M.A., Chao, M.T., Cook, J.G., Riccobonos, J., & Bardacke, N. (2017). Benefits of preparing for childbirth with mindfulness training: a randomized controlled trial with active comparison. Pregnancy and Childbirth, 17, 140-151
Dunkel Schetter, C. (2011). Psychological science on pregnancy: Stress processes, biopsychosocial models, and emerging research issues. Annual Reviews in Psychology, 62, 531–558.
Fairbrother, N., Young, A., Janssen, P., Antony, M. M., & Tucker, E. (2015). Depression and anxiety during the perinatal period. BMC Psychiatry, 15, 206–215.
Fisher, C., Hauck, Y., Bayes, S., & Byrne, J. (2012). Participant experience of mindfulness-based childbirth education: A qualitative study. BMC Pregnancy and Childbirth, 12, 126–136.
*Gambrel, L.E., & Piercy, F.P. (2015). Mindfulness-based relationship education for couples expecting their first child-part 1: a randomised mixed-methods program evaluation. Journal of Mental and Family Therapy, 41(1), 5-24
Grote, N. K., & Bledsoe, S. E. (2007). Predicting postpartum depressive symptoms in new mothers: The role of optimism and stress frequency during pregnancy. Health and Social Work, 32(2), 107–118.
Hall, H. G., Beattie, J., Lau, R., East, C., & Biro, M. A. (2016). Mindfulness and perinatal mental health: A systematic review. Women and Birth, 29(1), 62–71.
Higgins, J.P.T., Thomas, J., Chandler, J. Cumpston, M., Li, T., Page, M.J., and Welch, V.A. (Eds.). Cochrane Handbook for Systematic Reviews of Interventions version 6.2 (updated February 2021). Cochrane, 2021. Available from www.training.cochrane.org/handbook.
Hofmann, S. G., & Gómez, A. F. (2017). Mindfulness-Based Interventions for Anxiety and Depression. The Psychiatric Clinics of North America, 40(4), 739–749.
Hutton, B., Salanti, G., Caldwell, D. M., Chaimani, A., Schmidt, C. H., Cameron, C., Ioannidis, J. P., Straus, S., Thorlund, K., Jansen, J. P., Mulrow, C., Catala-Lopez, F., Gotzche, P. C., Dickersin, K., Boutron, I., Altman, D. G., & Moher, D. (2015). The PRISMA extension statement for reporting systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Annals of Internal Medicine, 162(11), 777–784.
Jadad, A. R., Moore, R. A., Carroll, D., Jenkinson, C., Reynolds, D. J., Gavaghnan, D., & McQuay, H. J. (1996). Assessing the quality of reports of randomised clinical trials: Is blinding necessary? Controlled Clinical Trials, 17(1), 1–12.
Kabat-Zinn, J. (2013). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Penguin Random House.
Kabat-Zinn, J. (2019). Nine mindfulness tips from Jon Kabat-Zinn. Habits for Wellbeing. https://www.habitsforwellbeing.com/nine-mindfulness-tips-from-jon-kabat-zinn/
Kashdan, T. B., & Rottenberg, J. (2010). Psychological flexibility as a fundamental aspect of health. Clinical Psychology Review, 30(7), 865–878.
Khoury, B., Lecomte, T., Fortin, G., Masse, M., Therien, P., Bouchard, V., Chapleau, M. A., Paquin, K., & Hofman, S. G. (2013). Mindfulness-based therapy: A comprehensive meta-analysis. Clinical Psychology Review, 33(6), 763–771.
Knight, M., Tuffnell, D., Kenyon, S., Shakespeare, J., Gray, R., & Kurinczuk, J.J. (Eds.) on behalf of MBRRACE-UK. Saving lives, improving mothers’ care: surveillance of maternal deaths in the UK 2011–13 and lessons learned to inform maternity care from the UK and Ireland confidential enquiries into maternal deaths and morbidity 2009–13. Oxford: National Perinatal Epidemiology Unit, University of Oxford 2015.
Kuyken, W., Warren, F. C., Taylor, R. S., Whalley, B., Crane, C., Bondolfi, G., Hayes, R., Huijbers, M., Ma, H., Schweizer, S., Segal, Z., Speckens, A., Teasdale, J. D., Van Heeringen, K., Williams, M., Byford, S., Byng, R., & Dalgleish, T. (2016). Efficacy of mindfulness-based cognitive therapy in prevention of depressive relapse: An individual patient data meta-analysis from randomized trials. JAMA Psychiatry, 73(6), 565–574.
Lever Taylor, B., Cavanagh, K., & Strauss, C. (2016). The effectiveness of mindfulness-based interventions in the perinatal period: a systematic review and meta-analysis. PLoS ONE 11(5): Article e0155720. https://doi.org/10.1371/journal.pone.0155720
Lipsey, M. W., & Wilson, D. B. (2001). Practical meta-analysis. Sage.
*Lonnberg, A.M., Park, E.R., & Goodman, J.H. (2020). Effects of a mindfulness based childbirth and parenting program on pregnant women’s perceived stress and risk of perinatal depression–Results from a randomized controlled trial. Journal of Affective Disorders, 262, 133–142
Maruthappu, M., Sood, H. S., & Keogh, B. (2014). The NHS Five Year Forward view: Transforming care. The British Journal of General Practice, 64(629), 635.
Matvienko-Sikar, K., Lee, L., Murphy, G., & Murphy, L. (2016). The effects of mindfulness interventions on prenatal well-being: A systematic review. Psychological Health, 31(12), 1415–1434.
Mayo-Wilson, E., Fusco, N., Li, T., Hong, H., Canner, J. K., & Dickersin, K. (2017). Multiple outcomes and analyses in clinical trials create challenges for interpretation and research synthesis. Journal of Clinical Epidemiology, 86, 39–50.
Murray, L., & Carothers, A. D. (1990). The validation of the Edinburgh Post-natal Depression Scale on a community sample. British Journal of Psychiatry, 157, 288–290.
*Muthukrishnan, S., Jain, R., Kohl, S., & Batra, S. (2016). Effect of mindfulness meditation on perceived stress scores and autonomic function tests of pregnant Indian women. Journal of Clinical Diagnostic Research, 10(4), CC05-CC08
National Collaborating Centre for Mental Health. (2018). The Perinatal Mental Health Care Pathways. Full implementation guidance (NHS England Publication No.08020). NHS England. http://www.england.nhs.uk/publication/the-perinatal-mental-health-care-pathways/
National Institute for Health and Care Excellence. (2014). Antenatal and postnatal mental health: clinical management and service guidance. (NICE clinical guideline No. 192). NICE. http://www.nice.org.uk/guidance/cg192
National Institute for Health and Care Excellence. (2016). Antenatal and postnatal mental health. (NICE Quality Standard No. 115). NICE. http://www.nice.org.uk/guidance/qs115
National Maternity Review (2016). Better births: improving outcomes of maternity services in England/A five year forward view for maternity care. NHS England. https://www.england.nhs.uk/wp-content/uploads/2016/02/national-maternity-review-report.pdf
*Pan, W., Chang, C., Chen, S., & Gau, M.L. (2019). Assessing the effectiveness of mindfulness-based programs on mental health during pregnancy and early motherhood - a randomized control trial. BMC Pregnancy Childbirth, 19, 346-354.
Pereira, P. K., Lima, L. A., Magnanini, M. M., Legay, L. F., & Lovisi, G. M. (2011). Severe mental illness in mothers and congenital malformations in newborns: A meta-analysis. Public Health Notebooks, 27(12), 2287–2298.
*Perez-Blasco, J., Vigner, P., & Rodrigo, M.F. (2013). Effects of mindfulness-based intervention on psychological distress, well-being, and maternal self-efficacy in breast-feeding mothers: results of a pilot study. Archives of Women’s Mental Health, 16, 227–236.
Saeed, A., Raana, T., Saeed, A. M., & Humayun, A. (2015). Effect of antenatal depression on maternal dietary intake and neonatal outcome: A prospective cohort. Nutrition Journal, 15(1), 64.
Saunders, T. A., Lobel, M., Veloso, C., & Meyer, B. A. (2006). Prenatal maternal stress is associated with delivery analgesia and unplanned cesareans. Journal of Psychosomatic Obstetrics and Gynecology, 27(3), 141–146.
Segal, Z., Williams, M., & Teasdale, J. (2013). Mindfulness-based cognitive therapy for depression (2nd edn.). Guilford Press.
Shi, Z., & MacBeth, A. (2017). The effectiveness of mindfulness-based interventions on maternal perinatal mental health outcomes: A systematic review. Mindfulness, 8(4), 823–847.
Sockol, L. (2015). A systematic review of the efficacy of cognitive behavioural therapy for treating and preventing perinatal depression. Journal of Affective Disorders, 177, 7–21.
Staneva, A. A., Bogossian, F., & Wittkowski, A. (2015). The experience of psychological distress, depression, and anxiety during pregnancy: A meta-synthesis of qualitative research. Midwifery, 31(6), 563–573.
Stein, A., Pearson, R. M., Goodman, S. H., Rapa, E., Rahman, A., McCallum, M., Howard, L. M., & Pariante, C. M. (2014). Effects of perinatal mental disorders on the fetus and child. The Lancet, 384, 1800–1819.
Stone, S. L., Diop, H., Declercq, E., Cabral, H. J., Fox, M. P., & Wise, L. A. (2015). Stressful events during pregnancy and postpartum depressive symptoms. Journal of Women’s Health, 24, 384–393.
Togher, K. L., Treacy, E., O’Keeffe, G. W., & Kenny, L. C. (2017). Maternal distress in late pregnancy alters obstetric outcomes and the expression of genes important for placental glucocorticoid signalling. Psychiatry Research, 255, 17–26.
UK Mindfulness-based teacher trainer network. (2015). Good practice guidelines for teaching mindfulness-based courses. British Association of Mindfulness-based Approaches. http://www.bamba.org.uk/wp-content/uploads/2019/06/UK-MB-teacher-GPG-2015-final-2.pdf
Viechtbauer, W., & Cheung, M.W.-L. (2010). Outlier and influence diagnostics for meta-analysis. Research Synthesis Methods, 1, 112–125.
Warriner, S., Crane, C., Dymond, M., & Krusch, A. (2018). An evaluation of mindfulness-based childbirth and parenting courses for pregnant women and prospective father/partners within the UK NHS (MBCP-4-NHS). Midwifery, 64, 1–10.
Webb, R., Abel, K., Pickles, A., & Appleby, L. (2005). Mortality in offspring of parents with psychotic disorders: A critical review and meta-analysis. The American Journal of Psychiatry, 162, 1045–1056.
Williams, J. M. G., & Swales, M. A. (2017). The use of mindfulness-based approaches for suicidal patients. Archives of Suicide Research, 8(4), 315–329.
*Woolhouse, H., Mercui, K., Judd, F., & Brown, S.J. (2014). Antenatal mindfulness intervention to reduce depression, anxiety and stress: a pilot randomised controlled trial of the MindBabyBody program in an Australian tertiary maternity hospital. BMC Pregnancy and Childbirth, 14, 369–385
*Zhang, J.Y., Cui, Y.X., Zhou, Y.Q., & Li, Y.L. (2019). Effects of mindfulness-based stress reduction on prenatal stress, anxiety and depression. Psychology, Health & Medicine, 24(1), 51–58
*Zhang, H., & Emory, E.K. (2015). A mindfulness-based intervention for pregnant African-American women. Mindfulness, 6(3), 663–674
Zhang, M.F., Wen, Y.S., Liu, W.Y., Peng, L.F., Wu, X.D., & Liu, Q.W. (2015). Effectiveness of mindfulness-based therapy for reducing anxiety and depression in patients with cancer: a meta-analysis. Medicine, 94(45), article e0897. https://doi.org/10.1097/MD.0000000000000897
Author information
Authors and Affiliations
Contributions
LC had the idea for the review. LC and MW performed the literature search, screening and risk of bias assessment. MW performed the data analysis. LC drafted the introduction and discussion. MW drafted the methods and results. Both authors revised and agreed the final version of the manuscript.
Corresponding author
Ethics declarations
Ethical approval
Not applicable.
Conflict of interest
The authors declare no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Corbally, L., Wilkinson, M. The Effect of Mindfulness-Based Interventions on Stress, Depression and Anxiety During the Perinatal Period in Women Without Pre-existing Stress, Depressive or Anxiety Disorders: a Systematic Review and Meta-analysis of Controlled Trials. Mindfulness 12, 2357–2370 (2021). https://doi.org/10.1007/s12671-021-01697-3
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-021-01697-3