Abstract
Compassion is an essential component of medical practice but is difficult to sustain over time. This problem is increasingly recognized in medical curricula. Mindfulness-based interventions have the potential to enhance compassion in medicine but this has not yet been tested. This study evaluated whether a brief mindfulness induction increased compassionate responding to difficult patients among medical students and assessed whether trait self-compassion moderated the impact of this experimental manipulation. A sample of 83 medical students completed baseline questionnaires including trait self-compassion prior to a laboratory session. In the laboratory, participants were gender block-randomized to mindfulness or control conditions before completing tasks assessing compassionate behaviour and decision-making in difficult patient vignettes. Finally, a covert behavioural measure allowed direct observation of responses to a request for help. The induction elicited mindfulness as intended and equivalently at both high and low levels of self-compassion. ANCOVAs showed that mindfulness predicted greater patient “liking” and “caring” but only among persons lower in self-compassion. The mindfulness intervention predicted greater helping behaviour, but primarily among those with higher self-compassion. A brief mindfulness induction showed some promise in enhancing compassionate responses and behaviour among medical students. Mindfulness training may offer a means of sustaining and enhancing compassion among some medical professionals but further research is needed.
Similar content being viewed by others
Introduction
Compassion is an essential component of medical practice. It is expected by patients (Emanuel and Dubler 1995; Fogarty et al. 1999; Meagher 2006; Old et al. 2011; Wiggins et al. 2009; Youngson 2011, 2012), regulatory bodies (American Medical Association; New Zealand Medical Association) and doctors themselves (Lown et al. 2011). More than being an expectation, however, compassionate care matters. Compassion predicts greater patient satisfaction, better patient-physician relationships, and better patient health outcomes (Canale et al. 2012; Fogarty et al. 1999; Lelorain et al. 2012; Steinhausen et al. 2014).
In medicine as elsewhere, compassion is often confused with empathy. However, while empathy refers to the cognitive and emotional processes involved in adopting another’s perspective (Engelen and Röttger-Rössler 2012), compassion involves the additional step of wanting to relieve suffering (Goetz et al. 2010; Jazaieri et al. 2014; Klimecki et al. 2013). However, sustaining compassion in medicine can be difficult (Hojat et al. 2009) and compassion fatigue impacts between 20 and 70 % of physicians (Benson et al. 2009; Lee et al. 2008; Markwell and Wainer 2009; Shanafelt et al. 2002); nearly half of patients and doctors report that compassionate care is missing in the health care system (Lown et al. 2011). Developing educational approaches and interventions that enhance or sustain compassion have become serious challenges in modern medicine and medical training (Fernando and Consedine 2014).
One approach that is gaining increasing traction as being of possible benefit in enhancing compassion is found in the study of mindfulness. Mindfulness, a continuous awareness of present moment experience in a calm and non-judgmental manner, has the potential to enhance compassionate care (Epstein, 1999; Fernando et al. 2014). In theory, mindfulness may help clinicians become more aware of their own psychological processes, biases, and prejudices, attend to the patient better, and become more flexible (Epstein 1999). Although their impact on compassion among medical trainees has yet to be investigated, mindfulness interventions reduce stress and burnout among health professionals (Beckman et al. 2012; Fortney et al. 2013; Goodman and Schorling 2012; Krasner et al. 2009), and enhance physician-patient connection (Beach et al. 2013; Krasner et al. 2009). Perhaps because of such benefits, mindfulness training is increasingly a part of the teaching curriculum in medical schools in the US (University of Rochester), Canada (University of Toronto), Australia (Monash University), and New Zealand (University of Auckland) (Dobkin and Hutchinson 2013).
However, despite evidence that compassion is often compromised in medical care (Lown et al. 2011; Youngson 2011, 2012) and that compassion can be increased with training (Weng et al. 2013), studies assessing the possible efficacy of interventions to enhance compassion among medical practitioners or evaluating the groups in which they might be successful are scant. One small, uncontrolled, pre-post study among 30 primary care physicians found benefits in physician mental health but no benefits in terms of self-reported compassion (Fortney et al. 2013). Another pre-post study testing a broad intervention including mindfulness training among 70 primary care physicians found that increases in mindfulness predicted improvements in self-rated perspective taking (Krasner et al. 2009). Such benefits are consonant with interview data suggestive of potential benefits following a “mindful communication” program among primary care physicians (Beckman et al. 2012). Data from non-medical populations has found that mindfulness training predicts greater odds of compassionate responding (offering a seat to a person on crutches) to a suffering stranger; whether such findings will replicate among medical professionals is unclear (Condon et al. 2013; Lim et al. 2015).
Overall then, while early studies among medical professionals show promise, our capacity to make empirically informed decisions regarding compassion-enhancing interventions and educational programs is limited insofar as designs have tended to be pre-post (i.e. experimental controls are lacking), are based in self-report data alone, and fail to control for social desirability biases in a domain where the target behaviour (compassion) is a professional requirement and thus expected. In addition, prior work suggests that personality factors may moderate the impact of mindfulness interventions, with persons higher in dispositional mindfulness at baseline sometimes showing greater benefits (including increases in empathy) (Shapiro et al. 2011). Following suggestions that self-compassion may be a necessary precursor to other-focused compassion, we tested whether a brief mindfulness induction would equally impact compassionate responding at different levels of dispositional self-compassion (Neff and Pommier 2013). Self-compassion entails being kind and understanding towards oneself in instances of pain or failure, perceiving one’s experiences as part of the larger human experience and holding painful thoughts and feelings in mindful awareness rather than over-identifying with them (Neff, 2003). Self-compassion has an established link to mindfulness (Neff and Dahm 2015) and is linked with altruistic behaviours including empathetic concern and other-focused compassion (Neff and Pommier 2013). The current report presents an experimental design, assesses both self-reported and objective indices of compassionate behaviour, and takes several steps to control for social desirability bias. Our primary aim was to assess whether randomization to a brief mindfulness induction would lead to greater compassionate responding and behaviour among trainee physicians using clinical vignettes and a behavioural test. A second aim was to test the possibility that trait self-compassion may be either (a) a better predictor of compassionate responding or (b) may moderate the impact of mindfulness intervention.
Method
Participants
After obtaining ethics approval (University of Auckland Human Participants Ethics Committee Ref 010361), we recruited 83 currently enrolled medical students, aged 18+ years and fluent in English. Participants were recruited through social media, advertising, and word of mouth. The advertisement mentioned about a study on “emotions and clinical decision making” but did not make reference to empathy or compassion. Participants ranged from 18 to 37 years (M = 21.41, SD = 3.12), 54.2 % were female, and students reported an average of 2.75 years of training (SD = 1.17).
Procedure
After providing consent, participants completed an online questionnaire including a measure assessing trait self-compassion before attending a 40-min laboratory session. Once at the laboratory, participants were greeted and asked to take a seat, before listening to a 10-min mindfulness induction exercise (mindfulness condition) or a speech on civic service (control condition) through headphones. Participants were randomised prior to the laboratory session. The mindfulness induction consisted of information about mindfulness and experiential exercises designed to increase state mindfulness (Erisman and Roemer 2010). After the induction, participants completed a state mindfulness and emotions manipulation check (below) and attached a small microphone to their clothing. The experimenter then left the room and participants viewed a series of clinical vignettes in which they made ratings about several difficult patients. After rating likely responses to each patient on several dimensions, an audio recording of their verbal response to each patient was recorded; these data are analysed elsewhere. Next, having rated all vignettes, participants allocated the time to be spent with each hypothetical patient within a constrained total of 60 min. A covert behavioural compassion test followed before the participant was thanked and debriefed, and the study terminated.
Measures
Trait Measures
A baseline questionnaire assessed several measures based on their relevance to the core mindfulness and compassion constructs. In line with recommendations regarding the reduction of method bias (Podsakoff et al. 2003), the measurement of the potential trait moderator (dispositional self-compassion) and the outcome ratings in the laboratory were separated in time, reducing the tendency for measures to covary for methodological reasons (Podsakoff et al. 2012). Although several measures were administered in the baseline phase, this report concentrates on those relevant to the data being presented here.
Trait Self-Compassion
Because self-compassion may be a necessary precursor for compassionate responding to others (Neff and Pommier 2013), participants completed the Self-Compassion Scale (Neff 2003). The SCS is a 26-item measure that uses a 1 (almost never) to 5 (almost always) metric to rate several aspects of dispositional self-compassion. Example items include, “I try to be understanding and patient toward aspects of my personality I don’t like” and “I’m disapproving and judgmental about my own flaws and inadequacies”. The scale has adequate psychometric properties and was internally reliable in this sample (α = 0.90).
Social Desirability
Given that medical training normatively includes the development and maintenance of prosocial traits, the expectation that trainee health professionals will be compassionate is very high; such bias is likely exaggerated by recruiting and conducting the study in the training context (Burks and Kobus 2012). Consequently, we administered the Marlowe-Crowne Short Form C (MCSF-C), a scale that allows for the brief measurement of presentational concerns likely to bias self-reports (W. M. Reynolds 1982). The MCSF-C is a 13-item true/false scale that is widely used and has adequate psychometric properties; it was reliable in this sample (α = 0.76).
Laboratory Measures
State Mindfulness
To ensure that the mindfulness induction was successful, the 13-item Toronto Mindfulness Scale was administered immediately following the manipulation (Lau et al. 2006). Participants rate items on a scale of 1 (not at all) to 5 (very much) according to how well each statement describes current experience. The TMS can be aggregated into two subscales—decentering and curiosity—or a total score, with higher scores indicating greater mindfulness. Internal reliability was adequate for both decentering (α = 0.79) and curiosity (α = 0.88) subscales. However, because of our focus on the possibility that mindfulness may allow trainee physicians to experience negative emotions in response to difficult patients without necessarily acting emotionally, we concentrated on the decentering component. Decentering is generally viewed as the ability or tendency to be present-focused but with a non-judgmental and accepting stance regarding thoughts and feelings (Fresco et al. 2007). It has been suggested that decentering may allow people to have negative emotional responses without translating them into behaviour (Reynolds et al. 2015).
State Affect
To ensure that our manipulation was specific to mindfulness rather than eliciting changes in related constructs, we administered the Brief Differential Emotions Scale (Brief DES) (Malatesta and Izard 1984). The Brief DES is an adaptation of the “state” version of the Differential Emotions Scale (DES III), a 30-item scale assessing 10 emotions (three items per subscale) with strong psychometric properties (Izard 1972; Youngstrom and Green 2003). In the Brief DES, each of the 10 emotions is described by the three synonyms taken from items in the original scale and, in this case, was supplemented by a single item with three adjectives specifically assessing each of low arousal positive (calm, at rest, peaceful) and negative emotions (dull, sleepy, sluggish) (Malatesta and Izard 1984). This brief form is useful when multiple measures are being used and excessive measurement might produce measurement effects. For this report, items were grouped into general positive and negative affect, with the low arousal positive emotions item examined independently. Internal reliabilities for the two-item positive affect scale was slightly low (α = 0.48) while that for negative affect (α = 0.63) was adequate.
Clinical Vignettes
To test whether self-compassionate traits or a brief mindfulness induction predicted compassionate responding among trainee physicians, participants were given a series of hypothetical case vignettes. Vignettes described initial interactions with a series of patients with challenging personal and clinical characteristics, a key barrier to compassion and diagnostic decision-making (Fernando and Consedine 2014). Methodologically, vignettes can convey complex data relevant to decision-making in a controlled and efficient manner (Greenhalgh et al. 2006). Patients were designed to be difficult in order to (a) counteract the “demand” for compassion among medical trainees and (b) evoke feelings of judgement, suspicion, or powerlessness (Steinmetz and Tabenkin 2001). To reduce the impact of idiosyncratic interpretation, five named patient vignettes were developed from the “difficult patient” literature (Paddam et al. 2010; Wilson 2005). However, preliminary analyses indicated Vignette 5 was responded to very differently from the other vignettes and we thus proceeded to analyse data for only the first four vignettes.
In a standard order, participants rated how they felt towards each patient and what they would do during consultations, two important and separate aspects of physician response (Greenhalgh et al. 2006). Ratings were made regarding how much participants liked the patient, wanted to help, and felt caring towards the patient. Because of their high sensitivity, naturalistic nature and superior numerical properties, ratings were made on 10 cm VAS (visual analogue scale) (Erisman and Roemer 2010; Price et al. 1983). A final rating regarding subjective closeness to patients was made using the Inclusion of Other in Self Scale, a method that asks participants to choose among a series of 7 images in which two circles overlap to varied degrees; greater overlap indicates greater feelings of closeness to the hypothetical patient (Bakker et al. 2000). Other exploratory ratings regarding possible referrals, patient responsibility, and acceding to patient demands were difficult to interpret and are not considered here.
Objective Measures
Two additional measures assessed more objective aspects of compassionate responding. First, participants were required to allocate consultation time to each patient within a constrained period (totalling 60 min across patients); allocating and balancing time is a clinically important process and differences may reflect aspects of compassion. Finally, a covert behavioural measure assessed compassionate behaviour directly. Having been told the study was finished, participants were asked to help the research assistant with an unrelated administrative task (45 min of help with questionnaire compilation work that was outstanding because of a personal commitment). Given skew in the raw data, responses were scored as 0 (No help), 1 (willing to help but less than 45 min), or 2 (willing to help for 45 min or more if needed) for analytic purposes.
Data Analysis
A 2 (high versus low trait self-compassion) × 2 (mindfulness versus control condition) MANOVA was used to assess differences between groups on the TMS state mindfulness measure (and the measures of state emotion). To address our primary questions, we assessed patient vignette ratings, time allocations, and the behavioural measure using parallel 2 (trait) × 2 (condition) ANCOVAs in which social desirability was controlled.
Results
Manipulation Check
We first sought to verify that mindfulness had been effectively elicited in the appropriate condition. A 2 (high versus low trait self-compassion) × 2 (mindfulness versus control condition) MANOVA showed that decentering scores were substantially higher in the mindfulness condition, F(1, 79) = 11.55, p < 0.001, part η 2 = 0.13. Conversely, however, there were no differences in positive affect, F(1, 79) = 0.25, p > 0.05, part η 2 = 0.00, negative affect, F(1, 79) = 1.68, p > 0.05, part η2 = 0.02, or calm affect, F(1, 79) = 0.01, p > 0.05, part η2 = 0.00, as a result of the manipulation (see Table 1). As importantly, there was no effect for trait self-compassion, F(1, 79) = 0.53, or an interaction between self-compassion and mindfulness, F(1, 79) = 0.52, indicating mindfulness was induced equivalently at both levels of trait self-compassion (see Table 1).
Trait Self-Compassion and State Mindfulness: Vignette Ratings
Having established that mindfulness was elicited as intended, we moved to consider whether trait self-compassion and/or state mindfulness were associated with more compassionate responses to hypothetical difficult patients. Means and standard deviations for these ratings can be seen in Table 2.
Greater trait self-compassion predicted greater liking, F(1, 79) = 4.37, p < 0.04, part η 2 = 0.05, but mindfulness did not, F(1, 79) = 0.01. Greater social desirability predicted marginally greater liking ratings, F(1, 77) = 3.88, p = 0.053, part η 2 = 0.05; interestingly, the interaction between self-compassion and condition was also significant, F(1, 77) = 4.18, p < 0.04, part η 2 = 0.05. Inspection of the interaction plot and follow-up testing (see Fig. 1a) showed that while high self-compassion participants expressed greater liking in the control condition, there were no differences as a function of self-compassion following the mindfulness induction.
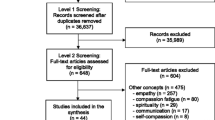
a Mean patient liking scores as a function of experimental condition and dichotomized trait self-compassion. b Mean desire to help patient scores as a function of experimental condition and dichotomized trait self-compassion. c Mean care for patient scores as a function of experimental condition and dichotomized trait self-compassion. d Mean subjective closeness to patient scores as a function of experimental condition and dichotomized trait self-compassion
A parallel model on ratings of participant’s desire to help showed that neither trait self-compassion, F(1, 79) = 0.53, mindfulness condition, F(1, 79) = 0.47, or their interaction, F(1, 79) = 2.26, predicted desire to help (see Fig. 1b); as might be expected greater social desirability was associated with greater reports of a desire to help, F(1, 79) = 6.74, p < 0.01, part η 2 = 0.03.
Third, we tested whether trait self-compassion and/or state mindfulness were associated with reporting greater care for difficult patients. Again, neither trait self-compassion, F(1, 79) = 0.27, mindfulness condition, F(1, 79) = 0.49, predicted reports of caring for hypothetical patients; greater social desirability was associated with marginally greater reports of caring F(1, 79) = 3.51, p = 0.06, and the interaction between self-compassion and mindfulness condition was again significant, F(1, 79) = 7.08, p < 0.01, part η 2 = 0.08. Inspection of this interaction (see Fig. 1c) showed that while the mindfulness induction increased caring among those with lower self-compassion, it had the opposite effect among those with greater self-compassion.
A final model was conducted on ratings of patient closeness. Trait self-compassion predicted ratings of marginally greater closeness, F(1, 79) = 3.54, p = 0.06, part η 2 = 0.04, but mindfulness condition, F(1, 79) = 0.55, and social desirability, F(1, 79) = 0.37, were unrelated. Once more, the interaction between self-compassion and mindfulness condition was significant, F(1, 79) = 8.08, p < 0.05, part η 2 = 0.09. Inspection of this interaction (see Fig. 1d) revealed a pattern similar to the liking ratings insofar as while persons with greater self-compassion rated themselves as closer in the control condition, the mindfulness induction increased closeness ratings among the less self-compassionate portion of the sample.
Trait Self-Compassion and State Mindfulness: Objective Measures
In the final phase of analysis, we tested whether trait self-compassion, induced mindfulness or their interaction predicted time allocations and actual helping behaviour in the laboratory setting. A mixed model factorial ANCOVA with vignette as a within-subject variable, trait compassion and condition served as between-subject variables, and controlling for desirability was conducted on time allocations. Unsurprisingly, given the constrained “total time” nature of the task, there were no effects for trait self-compassion, F(1, 79) = 1.45, mindfulness, F(1, 79) = 0.08, or their interaction, F(1, 79) = 0.21; social desirability scores were also non-significant, F(1, 79) = 1.80. However, there was a significant interaction between vignette and self-compassion, Wilk’s λ = 0.90, p < 0.05, part η 2 = 0.10 (see Fig. 2a), which showed that while persons with lower self-compassion varied the amount of time allocated to each patient, persons with high self-compassion allocated a relatively consistent amount of time for each.
Finally, a factorial ANCOVA predicting helping behaviour in the laboratory showed no main effects for either trait self-compassion, F(1, 79) = 0.90, or mindfulness, F(1, 79) = 1.06. However the interaction between self-compassion and mindfulness induction was significant, F(1,79) = 7.57, p < 0.05, part η 2 = 0.09. Inspection of the interaction (see Fig. 2b) showed that the mindfulness induction increased the helping behaviour of those higher in self-compassion and did not impact behaviour among the less self-compassionate.
Discussion
Compassion is central to the practice of medicine. It is expected by patients, regulatory bodies, and doctors themselves and is an important component of patient-centred medical education (Youngson 2011). However, compassion appears to fade with time and large numbers of clinicians suffer from compassion fatigue (Benson et al. 2009; Huggard 2003; McCray et al. 2008; Najjar et al. 2009; Showalter 2010). Only a few studies have assessed whether mindfulness increases compassion and none of these interventions have been tested among doctors or medical students. This study extends the literature linking mindfulness and compassion by testing whether a brief mindfulness induction increased compassionate decision making and behaviours among trainee physicians. Below, we revisit our findings regarding whether mindfulness might be suited to increasing compassionate attitudes and behaviour among medical students, consider the specific subsamples of trainee physicians for whom it might be more or less suited, and consider implications for intervention and medical education.
Our analysis showed that the brief mindfulness induction induced state mindfulness comparably across differing levels of trait self-compassion. However, somewhat inconsistent with preliminary work suggesting possible self-rated benefits to mindfulness training (Krasner et al. 2009), studies among non-medical student samples (Condon et al. 2013; Lim et al. 2015) and suggestions from commentators (Epstein 1999), the brief mindfulness induction per se was unsuccessful in engendering greater medical compassion, at least as indexed by ratings in response to difficult patient vignettes. We had expected that decentering, the aspect of state mindfulness perhaps most analogous to the “non-reacting” and “non-judging” components of trait mindfulness, might reduce the tendency for negative emotional responses to “push” through into ratings and behaviour.
It may be that there is something special about compassion or helping in medical contexts (where care is mandated), although theory suggests this is unlikely (Fernando and Consedine 2014). It is possible, for example, that the repeated nature of helping or the fact that it is expected in medical contexts lead to different (weaker) effects than those seen in other samples (Condon et al. 2013; Lim et al. 2015). This possibility noted, while prior mindfulness interventions have shown improvements in self-reported mental health, stress and burnout (Bazarko et al. 2013; Beckman et al. 2012; Fortney et al. 2013; Goodman and Schorling 2012; Krasner et al. 2009), and self-rated perspective taking among primary care physicians (Krasner et al. 2009), one prior study has failed to find changes in compassion (Fortney et al. 2013). Initially then, our findings appear more consistent with the Fortney et al. (2013) report insofar as the brief mindfulness induction did not lead to systematic increases in compassionate responses to patients. Also, our study compared to the other studies mentioned was a brief 10 min mindfulness induction versus much longer mindfulness training consisting of several weeks.
A second focus of the current study was to evaluate whether mindfulness might differentially impact compassionate responding in distinct subsamples of trainee physicians. Analyses showed that the brief mindfulness induction predicted a favourable pattern—greater “liking” and “caring” (and marginally greater “closeness”)—but only among medical students with lower self-compassion. In the absence of prior work testing the effects of a brief mindfulness induction on compassion among medical trainees, interpretation of this pattern is not simple.
One possible explanation is that the mindfulness induction differentially reduced the tendency to negatively appraise or blame the difficult patients among those with low self-compassion. Prior studies in non-medical samples have also found mindfulness to be more beneficial among less self-compassionate and more self-critical groups (Lown et al. 2011; Neff and Pommier 2013). Self-compassion—the ability/tendency to approach our own suffering and inadequacies with warmth and understanding—may be a necessary precursor to other-focused compassion (Neff 2012). Thus, because persons with lower self-compassion are more judgmental of both the self and others and might thus be less compassionate when the “other” is seen as responsible for their suffering, increasing mindfulness might differentially impact the less self-compassionate (Oveis et al. 2010; Petersen et al. 2012; Skitka et al. 2002). Because the patients most in need of compassion are also differentially likely to be those seen as responsible for their suffering, further work assessing this possibility is clearly needed.
Conversely, however, the intervention did not improve patient ratings among the more self-compassionate subsample and, in some instances, appear to have led to less compassionate patient ratings. A proposed explanation for the lack of improvement in patient ratings is that medical trainees with greater self-compassion (who probably were more mindful at baseline) became more aware of their (negative) responses to difficult patient vignettes which was then reflected their negative patient ratings. It is also possible that what is seen as “helpful” for a patient is not a simple matter or that the short induction was not “dosed” enough to cause a positive shift in this group’s perspective taking. The scenarios included a demanding woman with multiple medically unexplained symptoms and a middle-aged very overweight, unkempt, smelly and non-compliant man asking for his penis to be checked after having sex with a prostitute. Hence, while these are the very patients that likely most need compassion, they are not easy patients to like. It has been suggested that state mindfulness may increase the awareness of emotionality during decisional tasks (Reynolds et al. 2014; Reynolds et al. 2015), leading to greater incorporation of emotions in decision-making (Langer 1989) or more “direct” and honest ratings.
Perhaps more importantly in terms of healthcare delivery, the mindfulness induction increased actual helping behaviour among those with higher self-compassion in the laboratory context. The compassionate responding occurred despite having no change in the trainee physician’s appraisal of negative vignettes. Data from non-medical samples suggests that mindfulness training predicts offering a seat to a suffering stranger (a person on crutches) (Condon et al. 2013), even when the intervention is mindfulness-based, administered online, and comparatively brief (Lim et al. 2015). Mindfulness is associated with increased perspective taking and empathic concern which can facilitate increased actual helping behaviour which was observed in this experiment. The helping behaviour test occurred after difficult patient vignettes were presented to the students, and despite this, the high self-compassion mindfulness group was still willing to assist the laboratory assistant with an unrelated task. This may be perhaps because greater decentering helps people accept negative emotions such that they do not manifest in behaviour as readily (L. M. Reynolds et al. 2015). It may be that the improvements in emotion regulation (Hölzel et al. 2011) and decentering (Fresco et al. 2007) that accompany mindful states attenuate the extent to which negative emotional responses transition into behaviour. Decentering allows an individual to disindentify from their internal experience and be more non-judgmental with reduced reactivity when confronted with negative stimuli (Bernstein et al. 2015). More speculatively (given that it was not directly tested), it may be that in accepting, experiencing, and reporting negative responses to patients, mindful trainee physicians may actually be more willing to help them. As to why the high self-compassion subset appeared more willing to help may be explained by previous work suggesting that higher levels of self-compassion are linked to greater perspective taking, compassion to humanity, empathetic concern, and altruism (Neff and Dahm 2015; Neff and Pommier 2013).
Implications for Medical Education
In addition to acquisition of medical knowledge, medical education values training that emphasizes the alleviation of suffering—the essence of compassion (Association of American Medical Colleges 2014; Stern 1998). With the recent Stafford Hospital scandal (Francis 2013) and several findings suggesting that empathy and, potentially, compassion decline with progress through medical school (Cox et al. 2006; Hojat et al. 2009) training to sustain and enhance compassion in trainee physicians is no longer optional. Though there are some controlled studies on empathy, a precursor for compassion, there are no studies on compassion training among medical students or doctors (Riess et al. 2012; Satterfield and Hughes 2007).
A review of different compassion-enhancing protocols includes mindfulness training as a core feature (Jazaieri et al. 2012; Krasner et al. 2009; Weng et al. 2013). Mindfulness training is increasingly becoming a part of the global medical curriculum (Dobkin and Hutchinson 2013) as such training can mitigate physician burnout (Krasner et al. 2009) and improve physician medical diagnostic errors (Sibinga and Wu 2010). Consistent with the shift to patient-centred medical care (Laine and Davidoff 1996), mindfulness training has also been shown to increase physician-patient connection (Beach et al. 2013; Krasner et al. 2009). Our study adds to the list of potential benefits of mindfulness in medical education suggesting that, at least among low self-compassion students, interventions may encourage a more favourable disposition towards difficult patients and that helping behaviours may be increased among others.
Limitations and Future Directions
Although these findings represent a useful contribution to the understanding of how mindfulness-based interventions might be leveraged in the service of enhancing medical compassion, these data are not without their limitations. Limitations include the duration of the mindfulness intervention being only 10 min and concerns that the “dose” is insufficient to elicit a robust or valid mindfulness state. Although our analyses indicated that state changes were restricted to decentering mindfulness rather than manifesting in emotions, state and trait mindfulness likely operate differently (L. M. Reynolds et al. 2015). Examining the effects of more substantial mindfulness training protocols on medical compassion will be an interesting future direction (Krasner et al. 2009). Equally, the fact that vignettes were used should be borne in mind; using videos or simulated difficult patient actors to assess compassionate responding is an obvious and more ecologically valid next step. Lastly, the behavioural measure of helping a research assistant may or may not correspond to actual compassionate behaviour towards patients. While analyses controlled for social desirability, it may be that the mindfulness induction differentially heightens an awareness of the demand for prosociality in some groups and additional work testing the effects of mindfulness on patient-centred compassion is needed. Although the covert helping task shares similarities with a medical consultation in that it is a private transaction between a helper and a recipient of help, it is not overtly “medical” and occurs in the absence of a legislative or professional obligation to care; as such, it may be less ecologically valid when compared with a simulated, controlled medical set-up with standardized actors/patients.
A central aspect of patient-centred medical care, compassion, has been shown to be enhanced using mindfulness among some medical students in this study. Specifically, a brief mindfulness induction benefitted those at risk for having less compassion towards patients in vignettes and increased helping behaviour on those with greater self-compassion. Our results add to the evidence base surrounding the potential inclusion of mindfulness training in the education of future doctors.
References
American Medical Association. AMA’s Code of Medical Ethics Retrieved 24th October 2012, from http://www.ama-assn.org/ama/pub/physician-resources/medical-ethics/code-medical-ethics/principles-medical-ethics.page?
Association of American Medical Colleges. (2014) Retrieved 10 July, 2014, from https://www.aamc.org/about/
Bakker, A. B., Schaufeli, W. B., Sixma, H. J., Bosveld, W., & Van Dierendonck, D. (2000). Patient demands, lack of reciprocity, and burnout: a five-year longitudinal study among general practitioners. Journal of Organizational Behavior, 21(4), 425–441.
Bazarko, D., Cate, R., Azocar, F., & Kreitzer, M. (2013). The impact of an innovative mindfulness-based stress reduction program on the health and well-being of nurses employed in a corporate setting. Journal of Workplace Behavior and Health, 28(2), 107–122.
Beach, M. C., Roter, D., Korthuis, P. T., Epstein, R. M., Sharp, V., Ratanawongsa, N., & Saha, S. (2013). A multicenter study of physician mindfulness and health care quality. The Annals of Family Medicine, 11(5), 421–428. doi:10.1370/afm.1507.
Beckman, H., Wendland, M., Mooney, C. J., Krasner, M. S., Quill, T. E., Suchman, A. L., & Epstein, R. M. (2012). The impact of a program in mindful communication on primary care physicians. Academic Medicine, 87(6), 815–819. doi:10.1097/ACM.0b013e318253d3b2.
Benson, S., Sammour, T., Neuhaus, S. J., Findlay, B., & Hill, A. G. (2009). Burnout in Australasian younger fellows. ANZ Journal of Surgery, 79(9), 590–597.
Bernstein, A., Hadash, Y., Lichtash, Y., Tanay, G., Shepherd, K., & Fresco, D. M. (2015). Decentering and related constructs: a critical review and metacognitive processes model. Perspectives on Psychological Science, 10(5), 599–617.
Burks, D. J., & Kobus, A. M. (2012). The legacy of altruism in health care: the promotion of empathy, prosociality and humanism. Medical Education, 46(3), 317–325.
Canale, S. D., Louis, D. Z., Maio, V., Wang, X., Rossi, G., Hojat, M., & Gonnella, J. S. (2012). The relationship between physician empathy and disease complications: an empirical study of primary care physicians and their diabetic patients in Parma, Italy. Academic Medicine, 87(9), 1243–1249.
Condon, P., Desbordes, G., Miller, W. B., & DeSteno, D. (2013). Meditation increases compassionate responses to suffering. Psychological Science, 24(10), 2125–2127.
Cox, M., Irby, D. M., Cooke, M., Sullivan, W., & Ludmerer, K. M. (2006). American medical education 100 years after the Flexner report. New England Journal of Medicine, 355(13), 1339–1344.
Dobkin, P. L., & Hutchinson, T. A. (2013). Teaching mindfulness in medical school: where are we now and where are we going? Medical Education, 47(8), 768–779. doi:10.1111/medu.12200.
Emanuel, E. J., & Dubler, N. N. (1995). Preserving the physician-patient relationship in the era of managed care. JAMA, 273(4), 323–329.
Engelen, E.-M., & Röttger-Rössler, B. (2012). Current disciplinary and interdisciplinary debates on empathy. Emotion Review, 4(1), 3–8. doi:10.1177/1754073911422287.
Epstein, R. M. (1999). MIndful practice. JAMA, 282(9), 833–839. doi:10.1001/jama.282.9.833.
Erisman, S., & Roemer, L. (2010). A preliminary investigation of the effects of experimentally induced mindfulness on emotional responding to film clips. Emotion, 10(1), 72.
Fernando, A. T., & Consedine, N. S. (2014). Beyond compassion fatigue: the Transactional Model of Physician Compassion. Journal of Pain and Symptom Management, 48(2), 289–298. doi:10.1016/j.jpainsymman.2013.09.014.
Fernando, A. T., Hill, A. G., & Consedine, N. S. (2014). Mindfulness for surgeons. Australia and New Zealand Journal of Surgery, 82, 722–724.
Fogarty, L. A., Curbow, B. A., Wingard, J. R., McDonnell, K., & Somerfield, M. R. (1999). Can 40 seconds of compassion reduce patient anxiety? Journal of Clinical Oncology, 17(1), 371–379.
Fortney, L., Luchterhand, C., Zakletskaia, L., Zgierska, A., & Rakel, D. (2013). Abbreviated mindfulness intervention for job satisfaction, quality of life, and compassion in primary care clinicians: a pilot study. The Annals of Family Medicine, 11(5), 412–420. doi:10.1370/afm.1511.
Francis, R. (2013). Report of the Mid Staffordshire NHS foundation trust public inquiry: executive summary (Vol. 947): The Stationery Office.
Fresco, D. M., Moore, M. T., van Dulmen, M. H., Segal, Z. V., Ma, S. H., Teasdale, J. D., & Williams, J. M. (2007). Initial psychometric properties of the experiences questionnaire: validation of a self-report measure of decentering. Behavior Therapy, 38(3), 234–246.
Goetz, J. L., Keltner, D., & Simon-Thomas, E. (2010). Compassion: an evolutionary analysis and empirical review. Psychological Bulletin, 136(3), 351–374.
Goodman, M. J., & Schorling, J. B. (2012). A mindfulness course decreases burnout and improves well-being among healthcare providers. International Journal of Psychiatry in Medicine, 43(2), 119–128.
Greenhalgh, T., Chowdhury, M., & Wood, G. W. (2006). Story-based scales: development and validation of questionnaires to measure subjective health status and cultural adherence in British Bangladeshis with diabetes. Psychology, health & medicine, 11(4), 432–448.
Hojat, M., Vergare, M. J., Maxwell, K., Brainard, G., Herrine, S. K., Isenberg, G. A., & Gonnella, J. S. (2009). The devil is in the third year: a longitudinal study of erosion of empathy in medical school. Academic Medicine, 84(9), 1182–1191.
Hölzel, B. K., Lazar, S. W., Gard, T., Schuman-Olivier, Z., Vago, D. R., & Ott, U. (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6(6), 537–559.
Huggard, P. (2003). Compassion fatigue: how much can I give? Medical Education, 37(2), 163–164. doi:10.1046/j.1365-2923.2003.01414.x.
Izard, C. E. (1972). Patterns of emotions: a new analysis of anxiety and depression. New York: Academic.
Jazaieri, H., Jinpa, G., McGonigal, K., Rosenberg, E., Finkelstein, J., Simon-Thomas, E, Goldin, P. (2012). Enhancing compassion: a randomized controlled trial of a compassion cultivation training program. Journal of Happiness Studies, 1-14. doi: 10.1007/s10902-012-9373-z
Jazaieri, H., McGonigal, K., Jinpa, T., Doty, J. R., Gross, J. J., & Goldin, P. R. (2014). A randomized controlled trial of compassion cultivation training: effects on mindfulness, affect, and emotion regulation. Motivation and emotion, 38(1), 23–35.
Klimecki, O. M., Leiberg, S., Lamm, C., & Singer, T. (2013). Functional neural plasticity and associated changes in positive affect after compassion training. Cerebral Cortex, [published online June 1, 2012]. doi: 10.1093/cercor/bhs142
Krasner, M. S., Epstein, R. M., Beckman, H., Suchman, A. L., Chapman, B., Mooney, C. J., & Quill, T. E. (2009). Association of an educational program in mindful communication with burnout, empathy, and attitudes among primary care physicians. JAMA, 302(12), 1284–1293. doi:10.1001/jama.2009.1384.
Laine, C., & Davidoff, F. (1996). Patient-centered medicine: a professional evolution. JAMA, 275(2), 152–156.
Langer, E. J. (1989). Mindfulness. Cambridge, MA: Da Capo Press.
Lau, M. A., Bishop, S. R., Segal, Z. V., Buis, T., Anderson, N. D., Carlson, L., & Devins, G. (2006). The Toronto mindfulness scale: development and validation. Journal of Clinical Psychology, 62(12), 1445–1467.
Lee, F. J., Stewart, M., & Brown, J. B. (2008). Stress, burnout, and strategies for reducing them: what’s the situation among Canadian family physicians? Canadian Family Physician, 54(2), 234–235.
Lelorain, S., Brédart, A., Dolbeault, S., & Sultan, S. (2012). A systematic review of the associations between empathy measures and patient outcomes in cancer care. Psycho-Oncology, 21(12), 1255–1264. doi:10.1002/pon.2115.
Lim, D., Condon, P., & DeSteno, D. (2015). Mindfulness and compassion: an examination of mechanism and scalability. PLoS One, 10(2), e0118221.
Lown, B. A., Rosen, J., & Marttila, J. (2011). An agenda for improving compassionate care: a survey shows about half of patients say such care is missing. Health Affairs, 30(9), 1772–1778.
Malatesta, C. Z., & Izard, C. E. (1984). The facial expression of emotion: young, middle-aged, and older adult expressions. Emotion in adult development, 253-273.
Markwell, A. L., & Wainer, Z. (2009). The health and wellbeing of junior doctors: insights from a national survey. Medical Journal of Australia, 191(8), 441–444.
McCray, L. W., Cronholm, P. F., Bogner, H. R., Gallo, J. J., & Neill, R. A. (2008). Resident physician burnout: is there hope? Family Medicine, 40(9), 626–632.
Meagher, G. (2006). What can we expect from paid carers? Politics & Society, 34(1), 33–54. doi:10.1177/0032329205284755.
Najjar, N., Davis, L. W., Beck-Coon, K., & Carney Doebbeling, C. (2009). Compassion Fatigue. Journal of Health Psychology, 14(2), 267–277. doi:10.1177/1359105308100211.
Neff, K. D. (2003). The development and validation of a scale to measure self-compassion. Self and Identity, 2(3), 223–250.
Neff, K. D. (2012). The science of self-compassion. In C. K. Germer & R. D. Siegel (Eds.), Wisdom and compassion in psychotherapy: deepening mindfulness in clinical practice (pp. 79–92). New York: Guilford Press.
Neff, K. D., & Dahm, K. A. (2015). Self-compassion: what it is, what it does, and how it relates to mindfulness Handbook of Mindfulness and Self-Regulation (pp. 121-137): Springer.
Neff, K. D., & Pommier, E. (2013). The relationship between self-compassion and other-focused concern among college undergraduates, community adults, and practicing meditators. Self and Identity, 12(2), 160–176.
New Zealand Medical Association. NZMA Code of Ethics Retrieved 24th October 2012, from http://www.nzma.org.nz/about/ethics.html
Old, A., Adams, B., Foley, P., & White, H. D. (2011). Society’s expectation of the role of the doctor in New Zealand: results of a national survey. New Zealand Medical Journal, 124(1342), 10–22.
Oveis, C., Horberg, E., & Keltner, D. (2010). Compassion, pride, and social intuitions of self-other similarity. Journal of personality and social psychology, 98(4), 618–630.
Paddam, A., Barnes, D., & Langdon, D. (2010). Constructing vignettes to investigate anger in multiple sclerosis: Anisha Paddam, David Barnes and Dawn Langdon explain how to use vignettes effectively. Nurse researcher, 17(2), 60–73.
Petersen, M. B., Sznycer, D., Cosmides, L., & Tooby, J. (2012). Who deserves help? evolutionary psychology, social emotions, and public opinion about welfare. Political psychology, 33(3), 395–418.
Podsakoff, P. M., MacKenzie, S. B., Lee, J.-Y., & Podsakoff, N. P. (2003). Common method biases in behavioral research: a critical review of the literature and recommended remedies. Journal of applied psychology, 88(5), 879.
Podsakoff, P. M., MacKenzie, S. B., & Podsakoff, N. P. (2012). Sources of method bias in social science research and recommendations on how to control it. Annual Review of Psychology, 63, 539–569.
Price, D. D., McGrath, P. A., Rafii, A., & Buckingham, B. (1983). The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain, 17(1), 45–56.
Reynolds, L. M., Consedine, N. S., & McCambridge, S. A. (2014). Mindfulness and disgust in colorectal cancer scenarios: non-judging and non-reacting components predict avoidance when it makes sense. Mindfulness, 5(4), 442–452.
Reynolds, L. M., Lin, Y. S., Zhou, E., & Consedine, N. S. (2015). Does mindfulness reduce disgust-driven social avoidance and decision-making: an experimental investigation. Journal of Behavioral Medicine, 38(1), 98–109.
Reynolds, W. M. (1982). Development of reliable and valid short forms of the Marlowe‐Crowne Social Desirability Scale. Journal of Clinical Psychology, 38(1), 119–125.
Riess, H., Kelley, J. M., Bailey, R. W., Dunn, E. J., & Phillips, M. (2012). Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. Journal of General Internal Medicine, 27(10), 1280–1286.
Satterfield, J. M., & Hughes, E. (2007). Emotion skills training for medical students: a systematic review. Medical Education, 41(10), 935–941.
Shanafelt, T. D., Bradley, K. A., Wipf, J. E., & Back, A. L. (2002). Burnout and self-reported patient care in an internal medicine residency program. Annals of Internal Medicine, 136(5), 358–367.
Shapiro, S. L., Brown, K. W., Thoresen, C., & Plante, T. G. (2011). The moderation of mindfulness-based stress reduction effects by trait mindfulness: results from a randomized controlled trial. Journal of Clinical Psychology, 67(3), 267–277.
Showalter, S. E. (2010). Compassion fatigue: What is it? Why does it matter? Recognizing the symptoms, acknowledging the impact, developing the tools to prevent compassion fatigue, and strengthen the professional already suffering from the effects. American Journal of Hospice & Palliative Medicine, 27(4), 239–242.
Sibinga, E. M., & Wu, A. W. (2010). Clinician mindfulness and patient safety. JAMA, 304(22), 2532–2533.
Skitka, L. J., Mullen, E., Griffin, T., Hutchinson, S., & Chamberlin, B. (2002). Dispositions, scripts, or motivated correction?: understanding ideological differences in explanations for social problems. Journal of personality and social psychology, 83(2), 470.
Steinhausen, S., Ommen, O., Thüm, S., Lefering, R., Koehler, T., Neugebauer, E., & Pfaff, H. (2014). Physician empathy and subjective evaluation of medical treatment outcome in trauma surgery patients. Patient Education and Counseling, 95(1), 53–60.
Steinmetz, D., & Tabenkin, H. (2001). The ‘difficult patient’ as perceived by family physicians. Family Practice, 18(5), 495–500.
Stern, D. T. (1998). Practicing what we preach? An analysis of the curriculum of values in medical education. The American Journal of Medicine, 104(6), 569–575.
Weng, H. Y., Fox, A. S., Shackman, A. J., Stodola, D. E., Caldwell, J. Z. K., Olson, M. C., & Davidson, R. J. (2013). Compassion training alters altruism and neural responses to suffering. doi:10.1177/0956797612469537. Psychological Science, Retrieved from http://pss.sagepub.com/content/early/2013/05/20/0956797612469537.abstract.
Wiggins, M. N., Coker, K., & Hicks, E. K. (2009). Patient perceptions of professionalism: implications for residency education. Medical Education, 43(1), 28–33. doi:10.1111/j.1365-2923.2008.03176.x.
Wilson, H. (2005). Reflecting on the ‘difficult’ patient. New Zealand Medical Journal, 118(1212).
Youngson, R. (2011). Compassion in healthcare—the missing dimension of healthcare reform. In I. Renzenbrink (Ed.), Caregiver Stress and Staff Support in Illness, Dying, and Bereavement (p. 37). Oxford: Oxford University Press.
Youngson, R. (2012). Time to care: how to love your patients and your job. Rebelheart Publishers.
Youngstrom, E. A., & Green, K. W. (2003). Reliability generalization of self-report of emotions when using the Differential Emotions Scale. Educational and Psychological Measurement, 63(2), 279–295.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fernando, A.T., Skinner, K. & Consedine, N.S. Increasing Compassion in Medical Decision-Making: Can a Brief Mindfulness Intervention Help?. Mindfulness 8, 276–285 (2017). https://doi.org/10.1007/s12671-016-0598-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12671-016-0598-5