Abstract
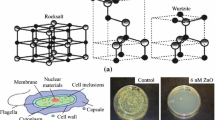
S. aureus produces biofilm, causing bacterial adherence to different surfaces. There are few studies on the antibacterial effects of nickel nanoparticles (Ni-NPs). The aim of the present study is to examine the inhibitory effect of Ni-NPs on biofilm formation against S. aureus treated with low-intensity photodynamic laser therapy for photoactivation by methylene blue (MB) dye. Ni-NPs were synthesized by solution reduction process and characterized by SEM, TEM, UV-Visible spectrum, and EDS analysis. The result shows that Ni-NPs are of high purity. The results revealed that the decrease in bacterial cell conductivity due to cell wall rupture and massive cell death which appears in the ultrastructure of a bacterial cell by TEM. Biofilm formation significantly decreased by increased different concentrations of 50, 100, 150, and 200 μg/ml of Ni-NPs, in the presence of MB which increased the absorption of the laser beam and enhance the killing effect of the cell envelope. It was concluded that the combined therapy of MB loaded into Ni-NPs, light irradiates both MB and the Ni-NPs associated with MB. Our composite has dual effect one coming from the photothermal effect of the Ni-NPs and the other coming from the photodynamic effect of the MB and is the more effective method to destroy S. aureus pathogenic microorganism.
Graphical Abstract















Similar content being viewed by others
References
Chunga, W., Petrofskyb, J. S., Laymonc, M., Logolusoa, J., Parka, J., Leea, J., & Leeb, H. (2014). The effects of low level laser radiation on bacterial growth. Physical Therapy Rehabilitation Science, 3(1), 20.
Gam, A. N., Thorsen, H., & Lønnberg, F. (1993). The effect of low-level laser therapy on musculoskeletal pain: A meta-analysis. Pain, 52, 63.
Wainwright, M. (2000). Methylene blue derivatives - suitable photoantimicrobials for blood product disinfection. International Journal of Antimicrobial Agents, 16(4), 381.
Layegh, E. R., Fathabadi, F. F., Lotfiniac, M., Zarea, F., Tofigh, A. M., Abrishami, S., & Piryaei, A. (2020). Photobiomodulation therapy improves the growth factor and cytokine secretory profile in human type 2 diabetic fibroblasts. Journal of Photochemistry and Photobiology B: Biology, 210(1), 111962.
Wainwright, M. (2005). The development of phenothiazinium photosensitisers. Photodiagnosis and Photodynamic Therapy, 2(4), 263.
Dai, T., Tegos, G. P., Zhiyentayev, T., Mylonakis, E., & Hamblin, M. R. (2010). Photodynamic therapy for methicillin-resistant Staphylococcus aureus infection in a mouse skin abrasion model. Lasers in Surgery and Medicine, 42(1), 44.
Chern-Hsiung, L. Y. (2003). Bactericidal effects of different laser wavelengths on periodontopathic germs in photodynamic therapy. Lasers in Medical Science, 18(1), 51.
Shi, S. F., Jia, J. F., Guo, X. K., Zhao, Y. P., Chen, D. S., Guo, Y. Y., & Zhang, X. L. (2016). Reduced Staphylococcus aureus biofilm formation in the presence of chitosan-coated iron oxide nanoparticles. International Journal of Nanomedicine, 11, 6499.
Lara, H. H., Romero-Urbina, D. G., Pierce, C., Lopez-Ribot, J. L., Arellano-Jimenez, M. J., & Jose-Yacaman, M. (2015). Effect of silver nanoparticles on Candida albicans biofilms: An ultrastructural study. Journal of Nanobiotechnology, 13, 91.
Loo, C. Y., Rohanizadeh, R., Young, P. M., Traini, D., Cav-aliere, R., Whitchurch, C. B., & Wing-Hin, L. (2016). Combination of silver nanoparticles and curcumin nanoparticles for enhanced anti-biofilm activities. Journal of Agricultural and Food Chemistry, 64, 2513.
Kalishwaralal, K., Kanth, S. B. M., Pandian, S. R., Deepak, V., & Gurunathan, S. (2010). Silver nanoparticles impede the biofilm formation by Pseudomonas aeruginosa and Staphylococcus epidermidis. Colloids and Surfaces. B, Biointerfaces, 79, 340.
Argueta-Figueroa, L., Morales-Luckie, R. A., Scougall-Vilchis, R. J., & Olea-Mejia, O. F. (2014). Synthesis, characterization and antibacterial activity of copper, nickel and bimetallic Cu–Ni nanoparticles for potential use in dental materials. Progress in Natural Science: Materials, 24, 321–328.
Wei, L., Fang, Z. Q., Ji Yan, L., Jie, F. U. J., SiJin, L., & Bin, J. G. (2011). Environmental and biological influences on the stability of silver nanoparticles. Chinese Science Bulletin, 56(19), 2009–2015.
Vahedi, M., Jazani, N. H., Yousefi, S., & Ghahremani, M. (2017). Evaluation of anti-bacterial effects of nickel nanoparticles on biofilm production by Staphylococcus epidermidis. Iranian Journal of Microbiology, 9(3), 160–168.
Liang, H., Mao, Y., Sun, Y., Gao, H. (2019). Transcriptional regulator ArcA mediates expression of oligopeptide transport systems both directly and indirectly in Shewanella oneidensis. Scientific Reports, 9(1),13839.
Tawfika, A. A., Alsharnoubib, J., & Morsy, M. (2015). Photodynamic antibacterial enhanced effect of methylene blue-gold nanoparticlesconjugate on Staphylococcal aureusisolated from impetigo lesions in vitro study. Photodiagnosis and Photodynamic Therapy, 12, 215.
Chandra, S., Kumar, A., & Tomar, P. K. (2014). Synthesis of Ni nanoparticles and their characterizations. Journal of Saudi Chemical Society, 18(5), 437.
Abo Neima, S. E., Motaweh, H. A., & Ragab, M. F. (2014). Effects of electric field on histopathological study, electrical properties and enzymes function of liver of albino rats. International Journal of Engineering Science, 4(12), 25.
Bai, W., Zhao, K., & Asami, K. (2007). Effects of copper on dielectric properties of E. coli cells Colloids and Surfaces B. Biointerfaces, 58, 105.
Abo-Neima, S. E., Khedr, Y. I., Kotb, M. M., Elhoseiny, A., & Motaweh, H. A. (2016). Control of metabolic activities of E.coli and S. aureus bacteria by electric field at resonance frequency in vitro study. International Journal of Engineering Science, 6(9), 13.
Greulich, C., Kittler, S., Epple, M., et al. (2009). Studies on the biocompatibility and the interaction of silver nanoparticles with human mesenchymal stem cells (hMSCs). Langenbeck's Archives of Surgery, 394, 495–502.
Narband, N., Tubby, S., Parkin, I. P., & Khan, A. U. (2008). Gold nanoparticles enhance the toluidine blue-induced lethal photosensitisation of Staphylococcus aureus. Current Nanoscience, 4, 409–414.
Sunde, P. T., Olsen, I., Debelian, G. J., & Tronstad, L. (2002). Microbiota of periapical lesions refractory to endodontic therapy. Journal of Endodontia, 28, 304.
Dai, T., Huang, Y., & Hamblin, M. R. (2009). Photodynamic therapy for localized infections–state of the art. Photodiagnosis and Photodynamic Therapy, 6, 170.
Rachel, C., Richard, A., Haverkamp, G., & Pak-Lam, Y. (2004). Investigation of morphological changes to Staphylococcus aureus induced by ovine-derived antimicrobial peptides using TEM and AFM FEMS. Microbiology Letters, 240, 105.
Lok, C. N., Ho, C. M., Chen, R., He, Q. Y., Yu, W. Y., Sun, H., Hang Tam, P. K., Chiu, J., & Che, C. (2006). Proteomic analysis of the mode of antibacterial action of silver nanoparticles. Journal of Proteome Research, 5, 916.
Abo-Neima, S. E., & El-kholy, S. M. (2016). Antibacterial characterization studies of silver nanoparticles against Staphylococcus aureus and Escherichia coli. Journal of Biophysical Biomedical Engineering, 17, 81.
Calixto, G. M. F., Bernegossi, J., De Freitas, L. M., Fontana, C. R., & Chorilli, M. (2016). Nanotechnology-based drug delivery systems for photodynamic therapy of cancer: A review. Molecules, 21, 342.
Silverira Alves, D. R., Almeida Decurcio, D. D., Goncalves Alencar, A. H., et al. (2022). Effect of low-power diode laser on infected root canals. Brazilian Dental Journal, 33(3), 8–17.
Komine, C., & Tsujimoto, Y. (2013). A small amount of singlet oxygen generated via excited methylene blue by photodynamic therapy induces the sterilization of Enterococcus faecalis. Journal of Endodontia, 39, 411.
Klausen, M., Ucuncu, M., & Bradley, M. (2020). Design of photosensitizing agents for targeted antimicrobial photodynamic therapy. Molecules, 25, 5239.
Khan, H. A., Ahmad, A., & Mehboob, R. (2015). Nosocomial infections and their control strategies. Asian Pacific Journal of Tropical Biomedicine, 5(7), 509.
Khosravi, A. D., Rostamian, J., & Moradinegad, P. (2008). Investigation of bactericidal effect of low level laser of gallium-aluminium-arsenide on cariogenic species of streptococci and lactobacillus. Medical Science, 8(6), 579.
Posten, W., Wrone, D. A., Dover, J. S., Arndt, K. A., Silapunt, S., & Alam, M. (2005). Low-level laser therapy for wound healing: Mechanism and efficacy. Dermatologic Surgery, 31(3), 334.
Sanati, M. H., Torkaman, G., Hedayati, M., & Mokhtari, M. (2010). Effect of Ga-As (904nm) and He-Ne (632.8 nm) laser on the improvement of biomechanical characteristics recovery in full thickness wound. Lasers in Medical Science, 7(1), 6.
Da Silva, J. P., Da Silva, M. A., Almeida, A. P., Lombardi, J. I., & Matos, A. P. (2010). Laser therapy in the tissue repair process: A literature review. Photomedicine and Laser Surgery, 28(1), 17.
Ng, G. Y., Fung, D. T., Leung, M. C., & Guo, X. (2004). Comparison of single and multiple applications of GaAlAs laser on rat medial collateral ligament repair. Lasers in Surgery and Medicine, 34(3), 285.
Ahmed, E., El-Gendy, A. O., Hamblin, M. R., & Mohamed, T. (2021). The effect of femtosecond laser irradiation on the growth kinetics of Staphylococcus aureus: An in vitro study. Journal of Photochemistry and Photobiology B: Biology, 221, 112240.
Ranjbar, I. R., & Takhtfooladi, M. A. (2016). The effects of low level laser therapy on Staphylococcus aureus infected third-degree burns in diabetic rats. Acta Cirúrgica Brasileira, 31(4), 250.
Alavi, M., Rai, M., Martinez, F., Kahrizi, D. I., et al. (2022). The efficiency of metal, metal oxide, and metalloid nanoparticles against cancer cells and bacterial pathogens: Different mechanisms of action. Cellular, Molecular and Biomedical Reports, 2(1), 10–21.
Alavi, M., Hamblin, M. R., Martinez, F., & Kennedy, J. F. H. (2022). Synergistic combinations of metal, metal oxide, or metalloid nanoparticles plus antibiotics against resistant and non-resistant bacteria. Micro Nano Bio Aspects, 1(1), 1–9.
Prabhu, S., Thangadurai, T. D., Bharathy, P. V., & Kalugasalam, P. (2022). Synthesis and characterization of nickel oxide nanoparticles using clitoria ternatea flower extract: Photocatalytic dye degradation under sunlight and antibacterial activity. Applications Results in Chemistry, 4, 100285.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The author declares no competing interests.
Research Involving Humans and Animals Statement
None.
Informed Consent
In our work, we do not work Human or Animals to get informed consent.
Research Involving Bacteria Treatment
Basic research in the treatment of a type of gram-negative bacteria called staphylococcus aureus bacteria.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Highlights
• Photosensitizing agent MB dye causes a decrease in the viable count of S. aureus by 35.3%, 38.2%, and 41.1% at 5, 10, and 15 min, respectively.
• Exposure of the suspension of S. aureus bacteria to laser light caused a decrease in the bacterial viable count with increasing the exposure time up to 20 min.
• Exposure of S. aureus suspension treated with MB dye and low-level laser light caused an increase in the percent of reduction to 85%.
• Exposure of S. aureus suspension to laser light in the absence of MB dye showed a decrease in the bacterial count by percent 67.6%.
• Exposure of S. aureus suspension to the combined effect of Ni-NPs, antibiotic, and laser irradiation time 20 min on S. aureus in the absence or presence of MB dye and antibiotic respectively, and decreased to 85% and 96.5% with MB dye and antibiotic, respectively.
• Irradiation of bacterial suspension to low-level laser light with MB dye after being treated by Ni-NPs (combined therapy) decreased the dielectric constant, dielectric loss, and conductivity at all observed frequencies.
• A decrease in dielectric constant, dielectric loss, and conductivity of the suspension could be due to the rupture of the bacterial wall, exiting of the cell content to the suspended medium, and cell death
• Ultrastructure study of S. aureus treated with Ni-NPs showed precipitation of nanoparticles through the bacterial cell wall and cause cell wall rupture, also revealed massive cell death seen with dirty background of rupture cell content.
• Ultrastructure study of S. aureus exposed to laser light with MB dye after treating the suspension of bacteria with Ni-NPs showing cell wall rupture leaving all the contents of the cell out. Adding of MB dye increases the absorption of the laser beam and enhances the killing effect might be due to the striking perturbation of the cell envelope.
• We recommended that we used the combined therapy in the treatment of S. aureus. This method offers an alternate traditional antimicrobial agent for the elimination of the organism from wounds, burns, and carriage sites. Once this method of killing bacteria is approved to physical therapy management of infected skin lesions such that of diabetic foot infections.
• Risks of thermal side effects during treatment are very low so the present method could find a very good acceptance with patients because it involved minimal pain.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Abo-Neima, S.E. Biological Activity of Photodynamic Laser Radiation and Nickel Nanoparticles on Staphylococcus aureus Bacteria. BioNanoSci. 13, 704–717 (2023). https://doi.org/10.1007/s12668-023-01074-5
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12668-023-01074-5