Abstract
Introduction
Spontaneous portosystemic shunts (SPSS) are frequent in liver cirrhosis and their prevalence increases as liver function deteriorates, probably as a consequence of worsening portal hypertension, but without achieving an effective protection against cirrhosis complications. This study was conducted to detect the prevalence of portosystemic shunts in liver cirrhosis patients and analyze its prognostic role.
Method
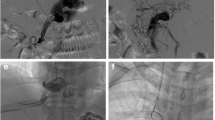
We conducted a prospective observational study, where 92 patients with decompensated cirrhosis were evaluated based on history, physical examination, biochemical tests and abdominal computed tomography (CT) angiography findings. A follow-up was done after six months for the development of cirrhosis-related complications.
Results
Of the 92 cirrhotic patients, 57.6% had SPSS (large SPSS + small SPSS) detected by multi-detector computed tomographic angiography. Overall, we found large SPSS in 24 (26.1%) patients, small SPSS in 29 (31.5%) patients and no shunt in 39 (42.4%) patients. Among the shunts, the splenorenal shunt is the most frequent type (25, 27.2%) followed by the paraumbilical shunt (20.7%). Previous decompensating events, including hepatic encephalopathy, ascites, spontaneous bacterial peritonitis and gastrointestinal bleed, were experienced more frequently by the large SPSS group followed by the small SPSS and without SPSS groups. Regarding follow-up, decompensating episodes of hepatic encephalopathy developed more frequently in patients with large SPSS (41.7%) than in patients with small SPSS (24.1%) followed by patients without SPSS (12.8%).
Conclusion
In summary, all cirrhotic patients should be studied with radiological imaging to detect the presence of portosystemic shunts. In several cases, patients with large SPSS had a more impaired liver function and more frequent complications of portal hypertension. So, these patients would probably benefit from a closer surveillance and more intensive therapy.

Similar content being viewed by others
Data availability
Available.
References
Garcia-Tsao G, Abraldes JG, Berzigotti A, et al. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology. 2017;65:310–35.
Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W. Practice Guidelines Committee of the American Association for the Study of Liver Diseases; Practice Parameters Committee of the American College of Gastroenterology. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46:922–38.
Akahane T, Iwasaki T, Kobayashi N, et al. Changes in liver function parameters after occlusion of gastrorenal shunts with balloon-occluded retrograde transvenous obliteration. Am J Gastroenterol. 1997;92:1026–30.
Arora A, Rajesh S, Meenakshi YS, Sureka B, Bansal K, Sarin SK. Spectrum of hepatofugal collateral pathways in portal hypertension: an illustrated radiological review. Insights Imaging. 2015;6:559–72.
Bagheri M, Hajati A, Hosseini M, Ostad SP. Comparison of findings of spontaneous splenorenal shunt in color Doppler sonography with multislice CT scan (64 slices) in liver transplant candidates. Eur J Radiol. 2012;81:2027–36.
Riggio O, Efrati C, Catalano C, et al. High prevalence of spontaneous portal-systemic shunts in persistent hepatic encephalopathy: a case-control study. Hepatology. 2005;42:1158–65.
Watanabe A. Portal-systemic encephalopathy in non-cirrhotic patients: classification of clinical types, diagnosis and treatment. J Gastroenterol Hepatol. 2000;15:969–79.
Crespin J, Nemcek A, Rehkemper G, Blei AT. Intrahepatic portal-hepatic venous anastomosis: a portal-systemic shunt with neurological repercussions. Am J Gastroenterol. 2000;95:1568–71.
Simón-Talero M, Roccarina D, Martínez J, et al. Association between portosystemic shunts and increased complications and mortality in patients with cirrhosis. Gastroenterology. 2018;154:1694-1705.e4.
Laleman W, Simon-Talero M, Maleux G, et al. Embolization of large spontaneous portosystemic shunts for refractory hepatic encephalopathy: a multicenter survey on safety and efficacy. Hepatology. 2013;57:2448–57.
Singh S, Kamath PS, Andrews JC, Leise MD. Embolization of spontaneous portosystemic shunts for management of severe persistent hepatic encephalopathy. Hepatology. 2014;59:735–6.
An J, Kim KW, Han S, Lee J, Lim YS. Improvement in survival associated with embolisation of spontaneous portosystemic shunt in patients with recurrent hepatic encephalopathy. Aliment Pharmacol Ther. 2014;39:1418–26.
Wu W, He C, Han G. Embolization of spontaneous splenorenal shunt for after-TIPS hepatic encephalopathy in a patient with cirrhosis and variceal bleeding. Hepatology. 2015;61:1761–2.
Doshi M, Pereira K, Carrion A, Martin P. Antegrade embolization of spontaneous splenorenal shunt for posttransjugular intrahepatic portosystemic shunt refractory hepatic encephalopathy. Hepatology. 2016;64:314–5.
Lelio AD, Cestari C, Lomazzi A, Beretta L. Cirrhosis: diagnosis with sonographic study of the liver surface. Radiology. 1989;172:389–92.
Sakurabayashi S, Sezai S, Yamamoto Y, et al. Embolization of portal-systemic shunts in cirrhotic patients with chronic recurrent hepatic encephalopathy. Cardiovasc Intervent Radiol. 1997;20:120–4.
Vilstrup H, Amodio P, Bajaj J, et al. Hepatic encephalopathy in chronic liver disease: 2014 Practice Guideline by the American Association for the Study of Liver Diseases and the European Association for the Study of the Liver. Hepatology. 2014;60:715–35.
Arroyo V, Gines P, Gerbes AL, et al. Definition and diagnostic criteria of refractory ascites and hepatorenal syndrome in cirrhosis. Hepatology. 1996;23:164–76.
Hoefs JC, Canawati HN, Sapico FL, Hopkins RR, Weiner J, Montgomerie JZ. Spontaneous bacterial peritonitis. Hepatology. 1982;2:399–407.
Angeli P, Ginès P, Wong F, et al. Diagnosis and management of acute kidney injury in patients with cirrhosis: revised consensus recommendations of the International Club of Ascites. J Hepatol. 2015;62(4):968–74.
Tarantino G, Citro V, Conca P, et al. What are the implications of the spontaneous spleno-renal shunts in liver cirrhosis? BMC Gastroenterol. 2009;9(1):89.
Chen CH, Wang JH, Lu SN, et al. Comparison of prevalence for paraumbilical vein patency in patients with viral and alcoholic liver cirrhosis. Am J Gastroenterol. 2002;97:2415–8.
Zardi EM, Uwechie V, Caccavo D, et al. Portosystemic shunts in a large cohort of patients with liver cirrhosis: detection rate and clinical relevance. J Gastroenterol. 2009;44:76–83.
Lipinski M, Saborowski M, Heidrich B, et al. Clinical characteristics of patients with liver cirrhosis and spontaneous portosystemic shunts detected by ultrasound in a tertiary care and transplantation centre. Scand J Gastroenterol. 2018;53:1107–13.
von Herbay A, Frieling T, Häussinger D. Color Doppler sonographic evaluation of spontaneous portosystemic shunts and inversion of portal venous flow in patients with cirrhosis. J Clin Ultrasound. 2000;28:332–9.
Cho SK, Shin SW, Lee IH, et al. Balloon occluded retrograde transvenous obliteration of gastric varices: outcomes and complications in 49 patients. AJR Am J Roentgenol. 2007;189:W365–72.
Ohnishi K, Sato S, Saito M, et al. Clinical and portal hemodynamic features in cirrhotic patients having a large spontaneous splenorenal and/or gastrorenal shunt. Am J Gastroenterol. 1986;81:450–5.
Philips CA, Rajesh S, George T, Ahamed R, Mohanan M, Augustine P. Early, late, or no shunt embolization in patients with cirrhosis- and portosystemic shunt-related hepatic encephalopathy. Indian J Gastroenterol. 2020;39:377–87.
Philips CA, Kumar L, Augustine P. Shunt occlusion for portosystemic shunt syndrome related refractory hepatic encephalopathy—a single-center experience in 21 patients from Kerala. Indian J Gastroenterol. 2017;36:411–9.
Author information
Authors and Affiliations
Contributions
Rishabh Kothari: data collection and drafting the article; Deepanshu Khanna: drafting the article, revising, editing, and final approval; Premashis Kar: supervision.
Corresponding author
Ethics declarations
Conflict of interest
RK, DK and PK declare that they have no conflict of interest.
Ethics statement
The study was performed conforming to the Helsinki Declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Ethics approval and consent to participate
Obtained.
Consent for publication
Obtained.
Ethical clearance
Obtained.
Disclaimer
The authors are solely responsible for the data and the content of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/ findings and content of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kothari, R., Khanna, D. & Kar, P. To evaluate the prevalence of spontaneous portosystemic shunts in decompensated cirrhosis patients and its prognostic significance. Indian J Gastroenterol 42, 677–685 (2023). https://doi.org/10.1007/s12664-023-01393-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-023-01393-1