Abstract
Background
Magnetic resonance enterography (MRE) has emerged as a novel tool for the assessment of disease activity in Crohn’s disease (CD). Real world data from Indian subcontinent on performance of MRE in terminal ileal CD are lacking.
Methods
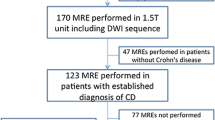
Retrospective analysis of patients with terminal ileal CD who underwent both ileo-colonoscopy and MRE was performed. Ileo-colonoscopy was considered the gold standard for assessment of disease activity. On ileo-colonoscopy, a simple endoscopic score for Crohn’s disease (SES-CD) ≥2 was considered active disease; presence of ulcers indicated severe disease. MRE scoring of the disease activity was performed using magnetic resonance index of activity (MARIA) and simplified MARIA (MARIAs). The measure of agreement between ileo-colonoscopy and MRE and comparison of MARIA and MARIAs for assessment of disease activity and sensitivity of MRE to detect mucosal ulcerations were calculated.
Results
Seventy patients with terminal ileal CD (mean age 40.74±15.56 years; 71.4% males [n=50]) were evaluated. The sensitivities of MARIA and MARIAs scores to detect active disease were 0.76 and 0.84, respectively. The area under the receiver operating characteristic curve (AUROC) for detecting severe disease was 0.836 (p<0.0001) for MARIA and 0.861 (p<0.0001) for MARIAs. For mild active disease, there was no agreement between SES-CD and MARIA or MARIAs; however, for severe disease, the agreement was fair and moderate for MARIA and MARIAs, respectively. MARIA and MARIAs were comparable for identification of active and severe disease (κ 0.759, p<0.0001 and κ 0.840, p<0.0001, respectively). MRE was 68.18% sensitive to detect mucosal ulcers.
Conclusion
MRE is a reliable and sensitive tool for detection of endoscopically severe, but not mild, terminal ileal CD.



Similar content being viewed by others
References
Kedia S, Sharma R, Makharia G, et al. Indian guidelines on imaging of the small intestine in Crohn’s disease: a joint Indian Society of Gastroenterology and Indian Radiology and Imaging Association consensus statement. Indian J Radiol Imaging. 2019;29:111–32.
Maaser C, Sturm A, Vavricka SR, et al. ECCO-ESGAR guideline for diagnostic assessment in IBD Part 1: Initial diagnosis, monitoring of known IBD, detection of complications. J Crohns Colitis. 2019;13:144–64.
Kim SH. Computed tomography enterography and magnetic resonance enterography in the diagnosis of Crohn’s disease. Intest Res. 2015;13:27–38.
Hammer MR, Podberesky DJ, Dillman JR. Multidetector computed tomographic and magnetic resonance enterography in children: state of the art. Radiol Clin N Am. 2013;51:615–36.
Rimola J, Rodriguez S, García-Bosch O, et al. Magnetic resonance for assessment of disease activity and severity in ileocolonic Crohn’s disease. Gut. 2009;58:1113–20.
Jairath V, Ordas I, Zou G, et al. Reliability of measuring ileo-colonic disease activity in crohn’s disease by magnetic resonance enterography. Inflamm Bowel Dis. 2018;24:440–9.
Rimola J, Alvarez-Cofiño A, Pérez-Jeldres T, et al. Comparison of three magnetic resonance enterography indices for grading activity in Crohn’s disease. J Gastroenterol. 2017;52:585–93.
Steward MJ, Punwani S, Proctor I, et al. Non-perforating small bowel Crohn’s disease assessed by MRI enterography: derivation and histopathological validation of an MR-based activity index. Eur J Radiol. 2012;81:2080–8.
Ordás I, Rimola J, Alfaro I, et al. Development and validation of a simplified magnetic resonance index of activity for Crohn’s disease. Gastroenterology. 2019;157:432–439.e1.
Oussalah A, Laurent V, Bruot O, et al. Diffusion-weighted magnetic resonance without bowel preparation for detecting colonic inflammation in inflammatory bowel disease. Gut. 2010;59:1056–65.
Joshi H, Mehta N, Desai D, Abraham P, Gupta T, Joshi A. Comparison of CT enterography with MR enterography, and utility of MRI severity index, in Crohn’s disease: a retrospective analysis. Trop Gastroenterol. 2019;39:117–23.
Hwang J, Kim JS, Kim AY, et al. Cryptogenic multifocal ulcerous stenosing enteritis: radiologic features and clinical behavior. World J Gastroenterol. 2017;23:4615–23.
Daperno M, D’Haens G, Van Assche G, et al. Development and validation of a new, simplified endoscopic activity score for Crohn’s disease: the SES-CD. Gastrointest Endosc. 2004;60:505–12.
Allen BC, Leyendecker JR. MR enterography for assessment and management of small bowel Crohn disease. Radiol Clin N Am. 2014;52:799–810.
Tolan DJ, Greenhalgh R, Zealley IA, Halligan S, Taylor SA. MR enterographic manifestations of small bowel Crohn disease. RadioGraphics. 2010;30:367–84.
Albert JG, Martiny F, Krummenerl A, et al. Diagnosis of small bowel Crohn’s disease: a prospective comparison of capsule endoscopy with magnetic resonance imaging and fluoroscopic enteroclysis. Gut. 2005;54:1721–7.
Masselli G, Casciani E, Polettini E, Gualdi G. Comparison of MR enteroclysis with MR enterography and conventional enteroclysis in patients with Crohn’s disease. Eur Radiol. 2008;18:438–47.
Rimola J, Ordás I, Rodríguez S, Ricart E, Panés J. Imaging indexes of activity and severity for Crohn’s disease: current status and future trends. Abdom Imaging. 2012;37:958–66.
Puylaert CAJ, Tielbeek JAW, Bipat S, Stoker J. Grading of Crohn’s disease activity using CT, MRI, US and scintigraphy: a meta-analysis. Eur Radiol. 2015;25:3295–313.
Taylor SA, Punwani S, Rodriguez-Justo M, et al. Mural Crohn disease: correlation of dynamic contrast-enhanced MR imaging findings with angiogenesis and inflammation at histologic examination--pilot study. Radiology. 2009;251:369–79.
Khater NH, Fahmy HS, Ali HI. Value of MR enterography in assessment of Crohn’s disease: Correlation with capsule endoscopy and colonoscopy. Egypt J Radiol Nucl Med. 2017;48:51–60.
Horsthuis K, Bipat S, Stokkers PCF, Stoker J. Magnetic resonance imaging for evaluation of disease activity in Crohn’s disease: a systematic review. Eur Radiol. 2009;19:1450–60.
Masselli G, Gualdi G. MR imaging of the small bowel. Radiology. 2012;264:333–48.
Sinha R, Murphy P, Sanders S, et al. Diagnostic accuracy of high-resolution MR enterography in Crohn’s disease: comparison with surgical and pathological specimen. Clin Radiol. 2013;68:917–27.
Pomerri F, Al Bunni F, Zuliani M, et al. Assessing pediatric ileocolonic Crohn’s disease activity based on global MR enterography scores. Eur Radiol. 2017;27:1044–51.
Puylaert CAJ, Nolthenius CJT, Tielbeek JAW, et al. Comparison of MRI activity scoring systems and features for the terminal ileum in patients with Crohn disease. Am J Roentgenol. 2019;212:W25–31.
Zhu N-Y, Zhao X-S, Miao F. Magnetic resonance imaging and Crohn’s disease endoscopic index of severity: correlations and concordance. World J Gastroenterol. 2018;24:2279–90.
Tsai R, Mintz A, Lin M, et al. Magnetic resonance enterography features of small bowel Crohn’s disease activity: an inter-rater reliability study of small bowel active inflammation in clinical practice setting. Br J Radiol. 2019; 92:20180930.
Naganuma M, Okuda S, Hisamatsu T, et al. Findings of ulceration and severe stricture on MRE can predict prognosis of Crohn’s disease in patients treated with anti-TNF treatment. Abdom Radiol. 2017;42:141–51.
Büning C, von Kraft C, Hermsdorf M, et al. Visceral adipose tissue in patients with crohn’s disease correlates with disease activity, inflammatory markers, and outcome. Inflamm Bowel Dis. 2015;21:2590–7.
Van Der Sloot KWJ, Joshi AD, Bellavance DR, et al. Visceral adiposity, genetic susceptibility and risk of complications among individuals with Crohn’s disease. Inflamm Bowel Dis. 2017;23:82–8.
Connelly TM, Juza RM, Sangster W, Sehgal R, Tappouni RF, Messaris E. Volumetric fat ratio and not body mass index is predictive of ileocolectomy outcomes in Crohn’s disease patients. Dig Surg. 2014;31:219–24.
Ding Z, Wu X-R, Remer EM, et al. Association between high visceral fat area and postoperative complications in patients with Crohn’s disease following primary surgery. Colorectal Dis. 2016;18:163–72.
Boparai G, Kedia S, Kandasamy D, et al. Combination of sarcopenia and high visceral fat predict poor outcomes in patients with Crohn's disease. Eur J Clin Nutr. 2021;75:1491–8.
Buisson A, Joubert A, Montoriol P-F, et al. Diffusion-weighted magnetic resonance imaging for detecting and assessing ileal inflammation in Crohn’s disease. Aliment Pharmacol Ther. 2013;37:537–45.
Bertin B, Desreumaux P, Dubuquoy L. Obesity, visceral fat and Crohn’s disease. Curr Opin Clin Nutr Metab Care. 2010;13:574–80.
Pringle PL, Stewart KO, Peloquin JM, et al. Body mass index, genetic susceptibility, and risk of complications among individuals with Crohn’s disease. Inflamm Bowel Dis. 2015;21:2304–10.
Erhayiem B, Dhingsa R, Hawkey CJ, Subramanian V. Ratio of visceral to subcutaneous fat area is a biomarker of complicated Crohn’s disease. Clin Gastroenterol Hepatol. 2011;9:684–687.e1.
Kucharzik T, Maaser C. Intestinal ultrasound and management of small bowel Crohn’s disease. Ther Adv Gastroenterol. 2018;11:1756284818771367.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
CK, AS, RM, VM, SG, VN, KG, DS, NB, KS, and AS declare no competing interests.
Ethics statement
The study was performed conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, the Indian Society of Gastroenterology or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kakkar, C., Singh, A., Mahajan, R. et al. Correlation between magnetic resonance enterography and ileo-colonoscopy for assessment of disease activity in terminal ileal Crohn’s disease. Indian J Gastroenterol 41, 465–474 (2022). https://doi.org/10.1007/s12664-022-01242-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-022-01242-7