Abstract
Background
Non-alcoholic fatty liver disease (NAFLD) has become a major health concern. Focal fat deposition frequently seems to involve segment IV b. This indicates a consistent pattern of fat deposition in the liver. The present study evaluates the pattern of fat distribution in the liver using computed tomogram (CT) attenuation index.
Methods
Two radiologists evaluated 517 non-contrast CT scan images of the abdomen and pelvis. Two 40-mm2 regions of interest (ROIs) were selected from each segment. The hepatic segmental densities (HSDs) were obtained by calculating the mean densities of areas of corresponding liver segments. The mean hepatic attenuation (MHA) was quantified by obtaining the mean segmental densities. Densities were compared between the segments and with the MHA.
Results
The mean age (SD) of the patients was 55.5 year (15.6), and 276 (53.4%) were males. The overall mean hepatic density was 53.05 (95% CI, 52.95–53.15) Hounsfield units (HU). The lowest mean HSD was observed in segment IV b and the highest mean HSD was observed in segment V. Segments I, IV a and IV b showed significantly lower mean HSDs and segments V, VI and VIII showed significantly higher mean HSDs compared with the overall mean MHA/mean hepatic density (MHD), whereas mean HSDs of segments II, III and VII were not significantly different from the overall mean MHA/MHD.
Conclusion
Segment IV b seems to be the most vulnerable site for fat deposition; focal lesions here should be carefully evaluated. Segments II, III and VII seem to closely represent MHD.



Similar content being viewed by others
References
Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA. 2015;313:2263–73.
Duseja A. Non-alcoholic fatty liver diseases in India - a lot done, yet more required! Indian J Gastroenterol. 2010;29:217–25.
Alam S, Gupta UD, Alam M, et al. Clinical, anthropometric, biochemical and histological characteristics of non obese non-alcoholic fatty liver disease patients of Bangladesh. Indian J Gastroenterol. 2014;33:452–7.
Siriwardana RC, Niriella MA, Liyanage CA, et al. Cryptogenic cirrhosis is the leading cause for listing for liver transplantation in Sri Lanka. Indian J Gastroenterol. 2013;32:397–9.
Michelotti GA, Machado MV, Diehl AM. NAFLD, NASH and liver cancer. Nat Rev Gastroenterol Hepatol. 2013;10:656–65.
Décarie PO, Lepanto L, Billiard JS, et al. Fatty liver deposition and sparing: a pictorial review. Insights Imaging. 2011;2:533–8.
Yamamoto K, Takada Y, Fujimoto Y, et al. Nonalcoholic steatohepatitis in donors for living donor liver transplantation. Transplantation. 2007;83:257–62.
Yoshikawa J, Matsui O, Takashima T, et al. Focal fatty change of the liver adjacent to the falciform ligament: CT and sonographic findings in five surgically confirmed cases. AJR Am J Roentgenol. 1987;149:491–4.
Limanond P, Raman SS, Lassman C, et al. Macrovesicular hepatic steatosis in living related liver donors: correlation between CT and histologic findings. Radiology. 2004;230:276–80.
Boyce CJ, Pickhardt PJ, Kim DH, et al. Hepatic steatosis (fatty liver disease) in asymptomatic adults identified by unenhanced low-dose CT. AJR Am J Roentgenol. 2010;194:623–8.
Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of non-alcoholic fatty liver disease: practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 2012;55:2005–23.
Couinaud C, Delmas A, Patel J. Le foie: études anatomiques et chirurgicales. Paris: Masson & Cie; 1957.
Park YS, Park SH, Lee SS, et al. Biopsy-proven nonsteatotic liver in adults: estimation of reference range for difference in attenuation between the liver and the spleen at nonenhanced CT. Radiology. 2011;258:760–6.
Matsui O, Takahashi S, Kadoya M, et al. Pseudolesion in segment IV of the liver at CT during arterial portography: correlation with aberrant gastric venous drainage. Radiology. 1994;193:31–5.
Matsui O, Kadoya M, Takahashi S, et al. Focal sparing of segment IV in fatty livers shown by sonography and CT: correlation with aberrant gastric venous drainage. AJR Am J Roentgenol. 1995;164:1137–40.
Vávra P, Vávrová M, Delongová P, et al. Hepatic pseudolesions adjacent to the falciform ligament. Rozhl Chir. 2015;94:449–53.
Kobayashi K, Matsui O, Yoshikawa J, et al. Right hepatic arterial supply to the posterior aspect of segment IV of the liver: analysis by CT during hepatic arteriography. Abdom Imaging. 1999;24:591–3.
Wang X, Xue HD, Jin ZY, et al. Quantitative hepatic CT perfusion measurement: comparison of Couinaud’s hepatic segments with dual-source 128-slice CT. Eur J Radiol. 2013;82:220–6.
Nalbantoglu IL, Brunt EM. Role of liver biopsy in non-alcoholic fatty liver disease. World J Gastroenterol. 2014;20:9026–37.
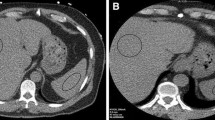
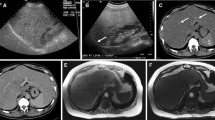
Delli Pizzi A, Mastrodicasa D, Sessa B, et al. Multiple liver pseudotumors due to hepatic steatosis and fatty sparing: a non invasive imaging approach. Eur J Radiol Open. 2019;6:56–9.
Wu S, Tu R, Zheng E, et al. Findings and implications of focal fatty sparing of the liver at follow-up: a preliminary study based on sonography, computed tomography, and magnetic resonance imaging. J Ultrasound Med. 2013;32:1695–702.
Myers RP, Pollett A, Kirsch R, et al. Controlled attenuation parameter (CAP): a non invasive method for the detection of hepatic steatosis based on transient elastography. Liver Int. 2012;32:902–10.
Author information
Authors and Affiliations
Contributions
Siriwardana Rohan Chaminda designed, conducted and did the manuscript writing.
Sivasundaram Thenuka conducted CT reporting, analysis and manuscript writing.
Paranaheva Lakmali conducted CT reporting and planning the study.
Ediriweera Deleepa Senajith conducted the data analysis and manuscript writing.
Corresponding author
Ethics declarations
Conflict of interest
RCS, TS, LP, and DSE declare that they have no conflicts of interest.
Ethics statement
The study was performed conforming to the Helsinki declaration of 1975, as revised in 2000 and 2008 concerning human and animal rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Disclaimer
The authors are solely responsible for the data and the contents of the paper. In no way, the Honorary Editor-in-Chief, Editorial Board Members, or the printer/publishers are responsible for the results/findings and content of this article.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This paper was presented as an oral presentation in Joint International congress ILTS, ELITA and LICAGE in Prague 2017.
Rights and permissions
About this article
Cite this article
Siriwardana, R.C., Sivasundaram, T., Paranaheva, L. et al. Computed tomography–based evaluation of segmental variation of liver density and its implications. Indian J Gastroenterol 39, 60–65 (2020). https://doi.org/10.1007/s12664-019-01008-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-019-01008-8