Abstract
Background
There is a paucity of reports on extraintestinal manifestations (EIMs) in patients with inflammatory bowel diseases (IBD) from Asia and India.
Methods
From May 2011 to October 2012, consecutive IBD patients underwent a detailed history and physical examination, also by trained rheumatologist, dermatologist, and ophthalmologist, about whether they experienced any EIM at the time of inclusion or in the past. The disease phenotype/severity and location was classified according to the Montréal classification. All underwent magnetic resonance imaging (MRI) of sacroiliac joints, liver function test (LFT), transabdominal ultrasound, and dual energy X-ray absorptiometry (DEXA) scanning at neck femur (bilateral) and L4-L5 spine.
Results
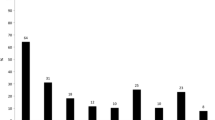
One hundred twenty patients were analyzed, 62 had Crohn’s disease (CD) and 58 had ulcerative colitis (UC). Thirty-eight percent had at least one while 20 % suffered from multiple EIMs. Except for uveitis and episcleritis, the frequency of individual EIMs did not differ between CD and UC patients. Twenty-three percent had peripheral arthritis, 18 % had ankylosing spondylitis, and 13 % had ophthalmological manifestations. Mucocutaneous manifestations, aphthous stomatitis and pyoderma gangrenosum (PG), were seen in 9 %. None had erythema nodosum (EN) or primary sclerosing cholangitis (PSC). Fifty percent of patients had either osteopenia or osteoporosis on DEXA. Multivariable analysis revealed female gender, Hindu religion, severe disease, and steroid usage were significantly associated with the presence of EIMs.
Conclusion
The prevalence of EIM is similar to that reported from Europe and USA, albeit higher than that previously reported in Asian patients. Female sex, religion, severe disease, and steroid use were associated with EIM.


Similar content being viewed by others
References
Danese S, Semeraro S, Papa A, et al. Extraintestinal manifestations in inflammatory bowel disease. World J Gastroenterol. 2005;11:7227–36.
Su CG, Judge TA, Lichtenstein GR. Extraintestinal manifestations of inflammatory bowel disease. Gastroenterol Clin N Am. 2002;31:307–27.
Edwards FC, Truelove SC. The course and prognosis of ulcerative colitis. Gut. 1964;5:1–15.
Farmer RG, Hawk WA, Turnbull RB Jr. Clinical patterns in Crohn’s disease: a statistical study of 615 cases. Gastroenterology. 1975;68:627–35.
Greenstein AJ, Janowitz HD, Sachar DB. The extra-intestinal complications of Crohn’s disease and ulcerative colitis: a study of 700 patients. Medicine. 1976;55:401–12.
Rankin GB, Watts HD, Melnyk CS, Kelly ML Jr. National Cooperative Crohn’s Disease Study: extraintestinal manifestations and perianal complications. Gastroenterology. 1979;77:914–20.
Veloso FT, Carvalho J, Magro F. Immune-related systemic manifestations of inflammatory bowel disease: a prospective study of 792 patients. J Clin Gastroenterol. 1996;23:29–34.
Bernstein CN, Blanchard JF, Rawsthorne P, Yu N. The prevalence of extraintestinal diseases in inflammatory bowel disease: a population-based study. Am J Gastroenterol. 2001;96:1116–22.
Mendoza JL, Lana R, Taxonera C, Alba C, Izquierdo S, Díaz-Rubio M. Extraintestinal manifestations in inflammatory bowel disease: differences between Crohn’s disease and ulcerative colitis. Med Clin (Barc). 2005;125:297–300.
Christodoulou DK, Katsanos KH, Kitsanou M, Stergiopoulou C, Hatzis J, Tsianos EV. Frequency of extraintestinal manifestations in patients with inflammatory bowel disease in Northwest Greece and review of the literature. Dig Liver Dis. 2002;34:781–6.
Lakatos L, Pandur T, David G, et al. Association of extraintestinal manifestations of inflammatory bowel disease in a province of western Hungary with disease phenotype: results of a 25-year follow-up study. World J Gastroenterol. 2003;9:2300–7.
Vavricka SR, Brun L, Ballabeni P, the Swiss IBD Cohort Study Group, et al. Frequency and risk factors for extraintestinal manifestations in the Swiss inflammatory bowel disease cohort. Am J Gastroenterol. 2011;106:110–9.
Bhagat S, Das KM. A shared and unique peptide in the human colon, eye, and joint detected by a monoclonal antibody. Gastroenterology. 1994;107:103–8.
Snook JA, de Silva HJ, Jewell DP. The association of autoimmune disorders with inflammatory bowel disease. Q J Med. 1989;72:835–40.
Bernstein CN, Wajda A, Blanchard JF. The clustering of other chronic inflammatory diseases in inflammatory bowel disease: a population-based study. Gastroenterology. 2005;129:827–36.
Lees CW, Barrett JC, Parkes M, Satsangi J. New IBD genetics: common pathways with other diseases. Gut. 2011;60:1739–53.
Prideaux L, Kamm MA, De Cruz PP, Chan FKL, Ng SC. Inflammatory bowel disease in Asia: a systematic review. J Gastroenterol Hepatol. 2012;27:1266–80.
Yi F, Chen M, Huang M, et al. The trend in newly diagnosed Crohn’s disease and extraintestinal manifestations of Crohn’s disease in central China: a retrospective study of a single center. Eur J Gastroenterol Hepatol. 2012;24:1424–9.
Hwangbo Y, Kim HJ, Park JS, et al. Sacroiliitis is common in Crohn’s disease patients with perianal or upper gastrointestinal involvement. Gut Liver. 2010;4:338–44.
Al-Jarallah K, Shehab D, Al-Azmi W, Al-Fadli A. Rheumatic complications of inflammatory bowel disease among Arabs: a hospital-based study in Kuwait. Int J Rheum Dis. 2013;16:134–8.
Sood A, Midha V, Sood N, Bhatia AS, Avasthi G. Incidence and prevalence of ulcerative colitis in Punjab, North India. Gut. 2003;52:1587–90.
Das K, Ghoshal UC, Dhali GK, Benjamin J, Ahuja V, Makharia GK. Crohn’s disease in India: a multicenter study from a country where tuberculosis is endemic. Dig Dis Sci. 2009;54:1099–107.
Pokharna KR, Kabra KP, Sharma R, Kochar KD. Extraintestinal manifestations of idiopathic ulcerative colitis in northwest India. Indian J Gastroenterol. 2004;23:89–90.
Kochhar R, Mehta SK, Nagi B, Bhatia V, Goenka MK, Malik AK. Extraintestinal manifestations in idiopathic ulcerative colitis. Indian J Gastroenterol. 1991;10:88–9.
Desai D, Patil S, Udwadia Z, Maheshwari S, Abraham P, Joshi A. Pulmonary manifestations in inflammatory bowel disease: a prospective study. Indian J Gastroenterol. 2011;30:225–8.
Khadgawat R, Makharia GK, Puri K. Evaluation of bone mineral density among patients with inflammatory bowel disease in a tertiary care setting in India. Indian J Gastroenterol. 2008;27:103–6.
Lennard-Jones JE. Classification of inflammatory bowel disease. Scand J Gastroenterol. 1989;170:2–6.
Satsangi J, Silverberg MS, Vermeire S, Colombel JF. The Montreal classification of inflammatory bowel disease: controversies, consensus, and implications. Gut. 2006;55:749–53.
Orchard TR, Wordsworth BP, Jewell DP. Peripheral arthropathies in inflammatory bowel disease: their articular distribution and natural history. Gut. 1998;42:387–91.
Rudwaleit R, van der Heijde D, Landewé R, et al. The development of assessment of spondyloarthritis international society classification criteria for axial spondyloarthritis (Part II): validation and final selection. Ann Rheum Dis. 2009;68:777–83.
Rudwaleit R, Jurik AG, Hermann K-G A, et al. Defining active sacroiliitis on magnetic resonance imaging (MRI) for classification of axial spondyloarthritis: a consensual approach by the ASAS/OMERACT MRI group. Ann Rheum Dis. 2009;68:1520–7.
Prevention and management of osteoporosis. Report of a WHO Scientific Group. Geneva, World Health Organization, 2003 (WHO Technical Report Series, No. 921).
Ling KL, Ooi CJ, Luman W, Cheong WK, Choen FS, Ng HS. Clinical characteristics of ulcerative colitis in Singapore, a multiracial city-state. J Clin Gastroenterol. 2002;35:144–8.
Hilmi I, Singh R, Ganesananthan S, et al. Demography and clinical course of ulcerative colitis in a multiracial Asian population: a nationwide study from Malaysia. J Dig Dis. 2009;10:15–20.
Makharia GK, Ramakrishna BS, Abraham P, for Indian Society of Gastroenterology Task Force on Inflammatory Bowel Disease, et al. Survey of inflammatory bowel diseases in India. Indian J Gastroenterol. 2012;31:299–306.
Singh B, Kedia S, Konijeti G, et al. Extraintestinal manifestations of inflammatory bowel disease and intestinal tuberculosis: frequency and relation with disease phenotype. Indian J Gastroenterol. 2015;34:43–50.
Jiang L, Xia B, Li J, et al. Retrospective survey of 452 patients with inflammatory bowel disease in Wuhan city, central China. Inflamm Bowel Dis. 2006;12:212–7.
Ghishan FK, Kiela PR. Advances in the understanding of mineral and bone metabolism in inflammatory bowel diseases. Am J Physiol Gastrointest Liver Physiol. 2011;300:G191–201.
Sharma SC, Singh R, Sharma AK, Mittal R. Incidence of low back pain in workage adults in rural North India. Indian J Med Sci. 2003;57:145–7.
Braun J, Inman R. Clinical significance of inflammatory back pain for diagnosis and screening of patients with axial spondyloarthritis. Ann Rheum Dis. 2010;69:1264–8.
Leclerc-Jacob S, Lux G, Rat AC, et al. The prevalence of inflammatory sacroiliitis assessed on magnetic resonance imaging of inflammatory bowel disease: a retrospective study performed on 186 patients. Aliment Pharmacol Ther. 2014;39:957–62.
Ytting H, Vind I, Bang D, Munkholm P. Sweet’s syndrome—an extraintestinal manifestation in inflammatory bowel disease. Digestion. 2005;72:195–200.
Bargiggia S, Maconi G, Elli M, et al. Sonographic prevalence of liver steatosis and biliary tract stones in patients with inflammatory bowel disease: study of 511 subjects at a single center. J Clin Gastroenterol. 2003;36:417–20.
Unisa S, Jagannath P, Dhir V, Khandelwal C, Sarangi L, Roy TK. Population-based study to estimate prevalence and determine risk factors of gallbladder diseases in the rural Gangetic basin of North India. HPB (Oxford). 2011;13:117–25.
Ye BD, Yang S-K, Boo S-J, et al. Clinical characteristics of ulcerative colitis associated with primary sclerosing cholangitis in Korea. Inflamm Bowel Dis. 2011;17:1901–6.
Acknowledgments
We thank the Department of Health and Family Welfare, Government of West Bengal, India, for their support and encouragement and providing the infrastructure to carry out this study. We thank Dr. David B Sachar for critically reviewing the data. The study did not receive any direct funding.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
DB, SB, PG, AD, AB, GKD, and KD declare that they have no competing interests.
Ethics statement
The study was performed in a manner to conform with the Helsinki Declaration of 1975, as revised in 2000 and 2008, concerning Human and Animal Rights, and the authors followed the policy concerning informed consent as shown on Springer.com.
Rights and permissions
About this article
Cite this article
Bandyopadhyay, D., Bandyopadhyay, S., Ghosh, P. et al. Extraintestinal manifestations in inflammatory bowel disease: Prevalence and predictors in Indian patients. Indian J Gastroenterol 34, 387–394 (2015). https://doi.org/10.1007/s12664-015-0598-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12664-015-0598-8