Abstract
Background
The most common material used for lateral sinus floor augmentation (LSFA) is xenogenic deproteinized bovine bone (DBB). However, in cases with significantly decreased residual bone height (RBH) (2–3 mm or less) where the osteogenic potential and vasculature of the recipient area are compromised the efficacy of the DBB is debatable. The aim of the study was to investigate the structural properties of the subantral bone regenerate by micro-CT in patients treated for significant alveolar ridge atrophy (RBH less than 3 mm) with LSFA and DBB grafts.
Materials and Methods
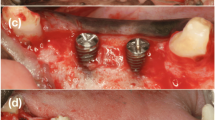
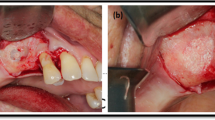
Twenty patients (10 men and 10 women) were included in the study and divided into two groups: (1) the main group–10 patients with edentulous posterior maxilla and RBH less than 3 mm, where LSFA was performed to create the appropriate bone volume for installation of the implants; (2) the control group–10 patients with RBH more than 10 mm and no necessity for bone augmentation procedures. In all patients, the bone samples were taken during the insertion of the implants in the area of interest. All samples were analyzed by micro-CT method. 3-D morphometric parameters were evaluated and compared in both groups.
Results
There were no significant differences in parameters that reflected 3-D morphometric structure and density of the edentulous alveolar bone with sufficient bone volume and augmented bone in patients with RBH less than 3 mm (p > 0.05). The slight differences were observed in trabecular architecture: In operated patients, the lower porosity, bone volume-to-surface ratio, anisotropy rate and increased trabecular pattern factor as a result of continuous functional remodeling process were observed.
Conclusion
Maxillary sinus floor elevation with DBB alone is a strategy, providing an appropriate 3-D architecture of the newly formed bone tissue and adequate primary stability of the dental implants. The biological properties and long-term remodeling of the augmented bone in patients of this category requires the further investigation.




Similar content being viewed by others
References
Pjetursson BE et al (2008) A systematic review of the success of sinus floor elevation and survival of implants inserted in combination with sinus floor elevation. J Clin Periodontol 35:216–240
Browaeys H, Peter De Bouvry H (2007) A literature review on biomaterials in sinus augmentation procedures. Clin Implant Dent Relat Res 9(3):166–177
Lie SAN, Claessen RMMA, Leung CAW et al (2022) Non-grafted versus grafted sinus lift procedures for implantation in the atrophic maxilla: a systematic review and meta-analysis of randomized controlled trials. Int J Oral Maxillofac Surg 51(1):122–132
Park Y-S (2019) Section plane effects on morphometric values of microcomputed tomography. Bio Med Res Int 9:120–124
Muller R, Van Campenhout H, Van Damme B et al (1998) Morphometric analysis of human bone biopsies: a quantitative structural comparison of histological sections and micro-computed tomography. Bone 23:59–66
Weiss P, Obadia L, Magne D, Bourges X, Rau C, Weitkamp T, Khairoun I, Bouler JM, Chappard D, Gauthier O, Daculsi G (2003) Synchrotron X-ray microtomography (on a micron scale) provides three-dimensional imaging representation of bone ingrowth in calcium phosphate biomaterials. Biomaterials 24(25):4591–4601
Plachokova AS, van den Dolder J, van den Beucken JP, Jansen JA (2009) Bone regenerative properties of rat, goat and human platelet-rich plasma. Int J Oral Maxillofac Surg 38(8):861–869
Fajardo J, Müller R, Ketcham RA et al (2007) Nonhuman anthropoid primate femoral neck trabecular architecture and its relationship to locomotor mode. Anot Rec 290(4):422–436
Cuijpers VMJI, Jaroszewicz J, Anil S et al (2014) Resolution, sensitivity, and in vivo application of high-resolution computed tomography for titanium-coated polymethyl methacrylate (PMMA) dental implants. Clin Oral Implants Res 25(3):359–365
Chappard C, Peyrin F, Bonnassie A et al (2006) Subchondral bone micro-architectural alterations in osteoarthritis: a synchrotron micro-computed tomography study. Osteoarth Cartilage 14(3):215–223
Ortiz MC, García-Sanz A, Bentley MD, Fortepiani LA, GarcíaEstañ J, Ritman EL, Romero JC, Juncos LA (2000) Microcomputed tomography of kidneys following chronic bile duct ligation. Kidney Int 58(4):1632–1640
Verna C, Dalstra M, Wikesjö UM, Trombelli L, Bosch C (2002) Healing patterns in calvarial bone defects following guided bone regeneration in rats. A micro-CT scan analysis. J Clin Periodontol 29(9):865–870
Marco Esposito, Pietro Felice, Helen V Worthington. Interventions for replacing missing teeth: augmentation procedures of the maxillary sinus. Cochrane Oral Health Group, School of Dentistry, The University of Manchester, Manchester, UK. University of Bologna, Bologna, Italy.
HU and BMD calibration in Bruker-MicroCT (2013) CT-analyser. Method note MN 9:1–30
Kanda Y (2013) Investigation of the free available easy-to-usesoftware ‘EZR’ for medical statistics. Bone Marrow Transplant 48:452–458
Lee J-H, Kim H-J, Yun J-H (2017) Three-dimensional microstructure of human alveolar trabecular bone: a micro-computed tomography study. J Periodontal Implant Sci 47(1):20–29
Hallman M, Sennerby L, Lundgren S (2002) A clinical and histologic evaluation of implant integration in the posterior maxilla after sinus floor augmentation with autogenous bone, bovine hydroxyapatite, or a 20:80 mixture. Int J Oral Maxillofac Implants 17(5):635–643
Merli M, Moscatelli M, Mariotti G et al (2013) Autogenous bone versus deproteinised bovine bone matrix in 1-stage lateral sinus floor elevation in the severely atrophied maxilla: a randomised controlled trial. Eur J Oral Implantol 6:27–37
Raghoebar GM, Schortinghuis J, Liem RS, Ruben JL, van der Wal JE, Vissink A (2005) Does platelet-rich plasma promote remodeling of autologous bone grafts used for augmentation of the maxillary sinus floor? Clin Oral Implant Res 16(3):349–356
Torres J, Tamimi F, Martinez PP et al (2009) Effect of platelet-rich plasma on sinus lifting: a randomized-controlled clinical trial. J Periodontol 36:677–687
Bouxsein ML, Boyd SK, Christiansen BA, Guldberg RE, Jepsen KJ, Muller R (2010) Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res 25:1468–1486
Bouxsein ML, Boyd SK, Blaine Christiansen A et al (2010) Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J Bone Miner Res 25(7):1468–1486
Márton K, Tamás SB, Orsolya N, Béla C, Ferenc D, Péter N, Csaba DN, Lajos C, Zsombor L, Eitan M, György S (2018) Microarchitecture of the augmented bone following sinus elevation with an albumin impregnated demineralized freeze-dried bone allograft (BoneAlbumin) versus anorganic bovine bone mineral: a randomized prospective clinical, histomorphometric, and micro-computed tomography study. Materials 11(2):202
Seo S-J, Kim Y-G (2020) In-situ analysis of the hydration ability of bone graft material using a synchrotron radiation X-ray micro-CT. Appl Biomater Funct Mater 18:2280800020963476
Kon K, Shiota M, Ozeki M, Yamashita Y (2009) Bone augmentation ability of autogenous bone graft particles with different sizes: a histological and micro-computed tomography study. Clin Oral Implants Res 20(11):1240–1246
Ulrich D, Hildebrand T, Van Rietbergen B, Müller R (1997) P Rüegsegger The quality of trabecular bone evaluated with micro-computed tomography, FEA and mechanical testing. Stud Health Technol Inform 40:97–112
Acknowledgment
The project No. TKP2021-NVA-07 and TKP2021-EGA-13 have been implemented with the support provided from the National Research, Development and Innovation Fund of Hungary, financed under the TKP2021-NVA and TKP2021-EGA funding schemes.
Funding
This work was supported by a research grant from the Ministry of Health of Ukraine (state registration number 0122U001339).
Author information
Authors and Affiliations
Contributions
AK, OS contributed to conception and design, analysis and interpretation of data, drafting the article. OS, TK contributed to data collection, analysis and interpretation of data. AK, ZH critically revised the article and supervised the study.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest. The founders had no role in the design of the study, in the collection, analyses, or interpretation of data, in the writing of the manuscript, or in the decision to publish the results.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shpachynskyi, O., Kiss, T., Helyes, Z. et al. Maxillary Bone Microstructure After Lateral Sinus Flour Augmentation with Deproteinized Bovine Bone Material in Severe Alveolar Bone Atrophy: Comparative Micro-CT Study. J. Maxillofac. Oral Surg. (2024). https://doi.org/10.1007/s12663-024-02113-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12663-024-02113-8