Abstract
Introduction
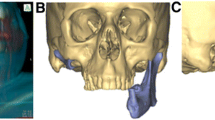
Mandibular reconstruction is often challenging. However, the revolution of computer-assisted design and computer-assisted manufacturing (CAD/CAM), virtual surgical planning (VSP) and 3D printing technology have changed this notion.
Patients and Methods
In this article, we have described six case scenarios where various aspects of VSP and 3D printing technology have been utilized for complex mandibular reconstruction procedures, to provide the patients with the best possible outcome in terms of form, function, and aesthetics.
Discussion
Virtual planning for tumour resection and fibula osteotomies and 3D printing of cutting guides and stereolith models have changed the face of mandibular reconstruction techniques. Increased accuracy, rehabilitation of normal anatomical configuration, appropriate dental rehabilitation, decreased intra-operative time and post-operative complications are some of the advantages. In addition, patient-specific implants eliminate the need for a separate donor site. 3D printed titanium cribs or meshes not only provide robustness, but also incorporates additional features that enable bone graft placement and excellent dental rehabilitation.
Conclusion
These modalities show promising results for reconstruction of complex mandibular defects.






Similar content being viewed by others
References
Weitz J, Bauer FJ, Hapfelmeier A, Rohleder NH, Wolff KD, Kesting MR (2016) Accuracy of mandibular reconstruction by three-dimensional guided vascularised fibular free flap after segmental mandibulectomy. Br J Oral Maxillofac Surg 54(5):506–510
Zhou L, Wang P, Han H, Li B, Wang H, Wang G, Zhao J, Liu Y, Wu W (2014) Prototyped grafting plate for reconstruction of mandibular defects. J Cranio-Maxillofacial Surg 42(8):1723–1729
Alalawy H, Abdulnabi HA (2022) The use of virtual surgical planning and 3D printing in reconstruction of a mandibular symphesial defect, challenges and gains: a case report. Adv Oral Maxillofacial Surg 5:100235
Bartier S, Mazzaschi O, Benichou L, Sauvaget E (2021) Computer-assisted versus traditional technique in fibular free-flap mandibular reconstruction: a CT symmetry study. Eur Ann Otorhinolaryngol Head Neck Dis 138(1):23–27
Tarsitano A, Ceccariglia F, Bevini M, Breschi L, Felice P, Marchetti C (2023) Prosthetically guided mandibular reconstruction using a fibula free flap: three-dimensional Bologna plate, an alternative to the double-barrel technique. Int J Oral Maxillofac Surg 52(4):436–441. https://doi.org/10.1016/j.ijom.2022.08.006
Li DTS, Leung YY (2023) Patient-specific implants in orthognathic surgery. Oral Maxillofac Surg Clin North Am 35(1):61–69. https://doi.org/10.1016/j.coms.2022.06.004
Brown JS, Barry C, Ho M, Shaw R (2016) A new classification for mandibular defects after oncological resection. Lancet Oncol 17(1):e23-30
Mahendru S, Jain R, Aggarwal A, Aulakh HS, Jain A, Khazanchi RK, Sarin D (2020) CAD-CAM vs conventional technique for mandibular reconstruction with free fibula flap: a comparison of outcomes. Surg Oncol 34:284–291
Bedogni A, Bettini G, Bedogni G, Menapace G, Sandi A, Michelon F, Di Carlo R, Franco P, Saia G (2021) Safety of boneless reconstruction of the mandible with a CAD/CAM designed titanium device: the replica cohort study. Oral Oncol 112:105073
Marechek A, AlShare A, Pack S, Demko C, Quereshy FA, Baur D (2019) Nonvascularized bone grafts for reconstruction of segmental mandibular defects: is length of graft a factor of success? J Oral Maxillofac Surg 77(12):2557–2566
Gil RS, Roig AM, Obispo CA, Morla A, Pagès CM, Perez JL (2015) Surgical planning and microvascular reconstruction of the mandible with a fibular flap using computer-aided design, rapid prototype modelling, and precontoured titanium reconstruction plates: a prospective study. Br J Oral Maxillofac Surg 53(1):49–53
Zhang L, Liu Z, Li B, Yu H, Shen SG, Wang X (2016) Evaluation of computer-assisted mandibular reconstruction with vascularized fibular flap compared to conventional surgery. Oral Surg Oral Med Oral Pathol Oral Radiol 121(2):139–148
Foley BD, Thayer WP, Honeybrook A, McKenna S, Press S (2013) Mandibular reconstruction using computer-aided design and computer-aided manufacturing: an analysis of surgical results. J Oral Maxillofac Surg 71(2):e111–e119
Rodby KA, Turin S, Jacobs RJ, Cruz JF, Hassid VJ, Kolokythas A, Antony AK (2014) Advances in oncologic head and neck reconstruction: systematic review and future considerations of virtual surgical planning and computer aided design/computer aided modeling. J Plast Reconstr Aesthet Surg 67(9):1171–1185
Ismail MB, Darwich K (2022) Reconstruction of large mandibular bone defects extended to the condyle using patient-specific implants based on CAD-CAM technology and 3D printing. Adv Oral Maxillofacial Surg 5:100229
Qaisi M, Zheng W, Al Azzawi T, Murphy J (2022) Patient specific bony and soft-tissue fibular reconstruction: perforator virtual surgical planning technique. Adv Oral Maxillofacial Surg 8:100363
Salinero L, Boczar D, Barrow B, Berman ZP, Diep GK, Trilles J, Howard R, Chaya BF, Rodriguez Colon R, Rodriguez ED (2022) Patient-centred outcomes and dental implant placement in computer-aided free flap mandibular reconstruction: a systematic review and meta-analysis. Br J Oral Maxillofac Surg 60(10):1283–1291. https://doi.org/10.1016/j.bjoms.2022.09.006
Sato H, Tanaka M, Inada T, Yamaguchi K, Katada R, Shirota T (2022) Reconstruction with an individualized titanium mesh cage following wide excision of a mandibular tumor under an intraoperative navigation system: a case series. Oral Maxillofacial Surg Cases 8(2):100258
Qassemyar Q, Assouly N, Temam S, Kolb F (2017) Use of a three-dimensional custom-made porous titanium prosthesis for mandibular body reconstruction. Int J Oral Maxillofac Surg 46(10):1248–1251
Lin CH, Hsu CH, Adarsh K, Hsu CM, Wu CM (2022) Real-time intraoperative computed tomography can accurize virtual surgical planning on the double-barrel fibular flap for mandibular reconstruction. J Plast Reconstr Aesthet Surg 75(8):2702–2705. https://doi.org/10.1016/j.bjps.2022.02.083
Soh HY, Hu LH, Yu Y, Wang T, Zhang WB, Peng X (2022) Navigation-assisted maxillofacial reconstruction: accuracy and predictability. Int J Oral Maxillofac Surg 51(7):874–882
Qaisi M, Kolodney H, Swedenburg G, Chandran R, Caloss R (2016) Fibula jaw in a day: state of the art in maxillofacial reconstruction. J Oral Maxillofac Surg 74(6):1284-e1
Ettinger KS, Morris JM, Alexander AE, Nathan JM, Arce K (2022) Accuracy and precision of the computed tomographic angiography perforator localization technique for virtual surgical planning of composite osteocutaneous fibular free flaps in head and neck reconstruction. J Oral Maxillofac Surg 80(8):1434–1444. https://doi.org/10.1016/j.joms.2022.03.018
Tsioukas V, Pikridas C, Karolos IA (2020) Challenges, opportunities, and limitations in 3D printing. 3D Print Appl Med Surg, pp 151–155.
Eshkalak SK, Ghomi ER, Dai Y, Choudhury D, Ramakrishna S (2020) The role of three-dimensional printing in healthcare and medicine. Mater Des 194:108940
Centers for Disease Control and Prevention. The National Institute for Occupational Safety and Health (NIOSH). https://www.cdc.gov/niosh/index.htm
Acknowledgements
We thank Osteo3DTM for helping us with virtual surgical planning and providing stereolith models. We thank CTARS – (Center for Technology Assisted Reconstructive Surgery) and Zimmer Biomet for printing the Patient Specific Implants.
Funding
The authors did not receive support from any organization for the submitted work.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Surgical procedures and material preparation were performed by AK, JT, GS, and ATK. The first draft of the manuscript was written by MS, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interests
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
Institutional Ethics Committee approval was not required for this article.
Informed Consent
Informed consent was obtained from all individual participants included in the article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kudva, A., Thomas, J., Saha, M. et al. Mandibular Reconstruction Modalities Using Virtual Surgical Planning and 3D Printing Technology: A Tertiary Care Centre Experience. J. Maxillofac. Oral Surg. (2024). https://doi.org/10.1007/s12663-024-02112-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12663-024-02112-9