Abstract
Aim & Objectives
To evaluate the ease, efficiency, effectiveness, and associated complications of the technique of percutaneous Gasserian glycerol rhizotomy (PGGR) under real-time fluoroscopic image guidance, for management of severe and refractory cases of primary trigeminal neuralgia, in medical compromised patients. To also assess the long-term efficacy and the necessity, if any, for repeat procedures to salvage recurrences.
Study Design & Setting
In a prospective study conducted at a single institution over a period of three years, 25 cases of Idiopathic Trigeminal Neuralgia refractory to conservative modalities of treatment including medication were managed with PGGR under real-time fluoroscopic image guidance. All the 25 patients included in this study were known surgical risks for relatively invasive treatment procedures, owing to factors such as advanced age and/or presence of co-morbidities.
Material & Methods
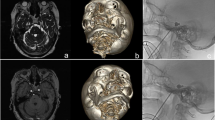
In order to minimize the risks related to the conventional techniques of Trigeminal root rhizotomy based on cutaneous landmarks alone, and to eliminate the need for frequent repositioning of the needle/cannula, we adopted a technique of real-time fluoroscopic image-guided negotiation of a 22 gauge (0.7 mm dia), 10-cm-long spinal nerve block needle through the foramen ovale, to reach the trigeminal cistern within the Meckel’s cave. The efficiency of the technique was assessed in terms of time taken, effort, and ease in performing it. Associated intra- and post-procedural complications were recorded. The immediate and long-term effectiveness of the procedure was evaluated by analysing the degree and duration of pain control achieved, time to recurrence, and the necessity for repeat procedures.
Results & Conclusion
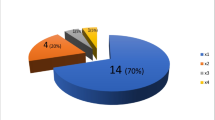
There were nil intra- or post-procedural complications encountered, and no failures associated with this procedure. Real-time fluoroscopic imaging enabled easy, quick, and successful negotiation of the nerve-block needle through the Foramen Ovale, so as to reach the Trigeminal cistern within the Meckel’s cave, within 11 min on an average. An immediate and long lasting post-procedural pain relief was achieved in all the patients. During the follow-up period of 36 months, recurrence of pain was observed in six cases, the mean timing of the recurrence being 26 months or more. Five of these cases were manageable with medication alone, and only one required a repeat procedure. These results indicate that PGGR under real-time fluoroscopic image guidance is a safe, simple, time-efficient, convenient, efficacious, reliable, and minimally invasive means of treating refractory and intractable cases of trigeminal neuralgia.





Similar content being viewed by others
References
Headache Classification Committee of the International Headache Society (IHS) (2018) The international classification of headache disorders, 3rd edition. Cephalagia 38:1–211
Maarbjerg S, Wolfram F, Gozalov A, Olesen J, Bendtsen L (2015) Association between neurovascular contact and clinical characteristics in classical trigeminal neuralgia: a prospective clinical study using 3.0 Tesla MRI. Cephalalgia 35:1077–1084
Devor M, Amir R, Rappaport ZH (2002) Pathophysiology of trigeminal neuralgia: the ignition hypothesis. Clin J Pain 18:4–13
Cohen-Gadol AA (2011) Microvascular decompression surgery for trigeminal neuralgia and hemifacial spasm: nuances of the technique based on experiences with 100 patients and review of the literature. Clin Neurol Neurosurg 113:844–853
Sheehan JP, Ray DK, Monteith S, Yen CP, Lesnick J, Kersh R et al (2010) Gamma Knife radiosurgery for trigeminal neuralgia: the impact of magnetic resonance imaging-detected vascular impingement of the affected nerve. Clin Artic J Neurosurg 113:53–58
Verheul JB, Hanssens PEJ, Lie ST, Leenstra S, Piersma H, Beute GN (2010) Gamma Knife surgery for trigeminal neuralgia: a review of 450 consecutive cases. Clin Artic J Neurosurg 113(Suppl):160–167
Koopman JS, de Vries LM, Dieleman JP, Huygen FJ, Stricker BH, Sturkenboom MC (2011) A nationwide study of three invasive treatments for trigeminal neuralgia. Pain 152:507–513
Cheng JS, Lim DA, Chang EF et al (2014) A review of percutaneous treatments for trigeminal neuralgia. Neurosurgery 10(Suppl 1):25–33
Montano N, Papacci F, Cioni B, Di Bonaventura R, Meglio M (2012) Percutaneous balloon compression for the treatment of trigeminal neuralgia in patients with multiple sclerosis. Analysis of the potentially prognostic factors. Acta Neurochir (Wien) 154:779–783
Bender MT, Bettegowda C (2016) Percutaneous procedures for the treatment of trigeminal neuralgia. Neurosurg Clin N Am 27:277–295
Pickett GE, Bisnaire D, Ferguson GG (2005) Percutaneous retrogasserian glycerol rhizotomy in the treatment of tic douloureux associated with multiple sclerosis. Neurosurgery 56:537–545
Kouzounias K, Lind G, Schechtmann G, Winter J, Linderoth B (2010) Comparison of percutaneous balloon compression and glycerol rhizotomy for the treatment of trigeminal neuralgia. J Neurosurg 113:486–492
Håkenson S (1981) Trigeminal neuralgia treated by the injection of glycerol into the trigeminal cistern. Neurosurgery 9:638–646
Linderoth B, Lind G (2012) Retrogasserian glycerol rhizolysis in trigeminal neuralgia. In: Quin˜ones- Hinojosa A (ed) Schmidek and Sweet’s Operative neurosurgical techniques. Phila Saunders Chapter, vol 123, pp 1393–1408
King JS, Jewett DL, Sundberg HR (1972) Differential blockade of cat dorsal root C fibers by various chloride solutions. J Neurosurg 36:569–583
Bennett MH, Lunsford LD (1984) Percutaneous retrogasserian glycerol rhizotomy for tic douloureux. Part 2: results and implications of trigeminal evoked potential studies. Neurosurgery 14:431–435
Lunsford LD, Bennett MH, Martinez AJ (1985) Experimental trigeminal glycerol injection: Electrophysiologic and morphologic effects. Arch Neurol 42:146–149
Koizuka S, Saito S, Tobe M, Sekimoto K, Obata H, Koyama Y (2010) Percutaneous radiofrequency mandibular nerve rhizotomy guided by high-speed real time computed tomography fluoroscopy. Anesth Analg 111:763–767
Xu SJ, Zhang WH, Chen T, Wu CY, Zhou MD (2006) Neuronavigator-guided percutaneous radiofrequency thermocoagulation in the treatment of intractable trigeminal neuralgia. Chin Med J (Engl) 119:1528–1535
Besi E, Boniface DR, Cregg R, Zakrzewska JM (2015) Comparison of tolerability and adverse symptoms in oxcarbazapine and carbamazepine in the treatment of trigeminal neuralgia and neuralgiform headches using the Liverpool Adverse Events Profile (AEP). J Headache Pain 16:563
Tatli M, Satici O, Kanpolat Y et al (2008) Various surgical modalities for trigeminal neuralgia: literature study of respective long-term outcomes. Acta Neurochir (Wien) 150:243–255
Rappaport ZH, Devor M (1994) Trigeminal neuralgia : the role of self-sustaining discharge in the trigeminal ganglion. Pain 56:127–138
Bendtsen JM, Zakrzewska JA, Braschinsky M, Di Stefano G, Donnet A, Eide PK et al (2019) European academy of neurology guideline on trigeminal neuralgia. Eur J Neurol 26:831–849
Heinskou T, Maarbjerg S, Rochat P, Wolfram F, Jensen RH, Bendtsen L (2015) Trigeminal neuralgia–a coherent cross-specialty management program. J Headache Pain 16:66
Yuan M, Zhou HY, Xiao ZL, Wang W, Li X-L, Chen S-J et al (2016) Efficacy and safety of gabapentin vs carbamazepine in the treatment of trigeminal neuralgia: a meta-analysis. Pain Pract 16:1083–1091
Zakrzewska JM, Coakham HB (2012) Microvascular decompression for trigeminal neuralgia: update. Curr Opin Neurol 25:296–301
Maarbjerg S, Di Stefano G, Bendtsen L, Cruccu G (2017) Trigeminal neuralgia—diagnosis and treatment. Cephalalgia 37:648–657
Egan RA, Pless M, Shults WT (2001) Monocular blindness as a complication of trigeminal radiofrequency rhizotomy. Am J Ophthalmol 131:237–240
Savas A, Sayin M (2010) Subarachnoid bleeding into the superior cerebellopontine cistern after radiofrequency trigeminal rhizotomy: case report. Acta Neurochir (Wien) 152:561–562
Arrese I, Lobato RD, Alén JF, Lagares A, Miranda P (2005) Acute subdural and intratemporal hematoma as a complication of percutaneous compression of the gasserian ganglion for trigeminal neuralgia. Neurocirugia (Astur) 16:177–182
Acknowledgements
The author of this article has not received any research grant, remuneration, or speaker honorarium from any company or committee whatsoever, and neither owns any stock in any company.
Funding
This study was not funded by any organization/society.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The author declares that she does not have any conflict of interest.
Ethical approval
This article does not contain any new studies with human participants or animals performed by the author.
Informed consent
Written informed consent was obtained from all the individual participants in this study, including the parents of the Minors.
Human Participants and/or Animals
All procedures performed on the patients (human participants) involved were in accordance with the ethical standards of the institution and/or national research committee, as well as with the 1964 Helsinki Declaration and its later amendments and comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jeyaraj, P. Efficiency and Efficacy of Real-Time Fluoroscopic Image-Guided Percutaneous Gasserian Glycerol Rhizotomy (PGGR), for Intractable Cases of Trigeminal Neuralgia. J. Maxillofac. Oral Surg. 21, 1053–1064 (2022). https://doi.org/10.1007/s12663-021-01682-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-021-01682-2