Abstract
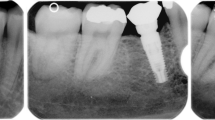
The aims of this study were to analyze prospectively and comparatively the peri-implant bone crest levels, bone density, stability and success rate of implants with different surface treatments in human edentulous mandibles. Twenty edentulous patients were selected. Four different implants were placed between the mental foramen. Four groups were evaluated: (1) laser-modified surface (LASER), (2) surface modified by laser with deposition of apatites (LASER + HA), (3) surface modified by double acid etching (ACID, Implacil De Bortoli) and (4) surface modified by sandblasting and acid etching (SLActive®, Straumann). Clinical, radiographic, resonance frequency and tomographic analyses were used. After 4 months, mandibular fixed implant prostheses were installed. Clinical and radiographic analyses were performed at times T0 (immediately after implant placement), T1 (15 days), T2 (30 days), T3 (60 days), T4 (90 days), T5 (120 days), T6 (180 days) and T7 (360 days), post-implant placement. The resonance frequency analysis (RFA) was measured at T0, T4, T6 and T7. The tomographic analysis was performed at T0, T4 and T7. In the radiographic bone density analysis, a statistical difference was found between the SLActive® and LASER + HA groups at T4 (p < 0.05). Statistical differences were observed in RFA at T4 (90 days), between the SLActive® and LASER groups (p < 0.05) and between the SLActive® and LASER + HA groups (p < 0.05). At T6 and T7, statistical differences were found between the SLActive® group and all other implant surfaces (p < 0.01). The experimental surfaces analyzed showed encouraging positive outcomes compared to those of the SLActive® surface. Long-term follow-up should be performed to confirm these results.






Similar content being viewed by others
References
Wennerberg A, Albrektsson T (2009) Effects of titanium surface topography on bone integration: a systematic review. Clin Oral Implants Res 20:172–184
Al-Hamdan SH, Al-Hamdan K, Junker R et al (2012) Effect of implant surface properties on peri-implant bone healing: implant stability and microcomputed tomographic analysis. Int J Oral Maxillofac Implants 27:77–83
Insua A, Monje A, Wang HL et al (2017) Basis of bone metabolism around dental implants during osseointegration and peri-implant bone loss. J Biomed Mater Res A 105:2075–2089
Bedrossian E, Sullivan RM, Fortin Y et al (2008) Fixed-prosthetic implant restoration of the edentulous maxilla: a systematic pretreatment evaluation method. J Oral Maxillofac Surg 66:112–122
Zhao K, Mai QQ, Wang XD et al (2013) Occlusal designs on masticatory ability and patient satisfaction with complete denture: a systematic review. J Dent 41:1036–1042
Peck CC (2016) Biomechanics of occlusion–implications for oral rehabilitation. J Oral Rehabil 43:205–214
Moradpoor H, Salari F, Ebadian B et al (2018) Patient satisfaction with occlusal scheme of conventional complete dentures: a randomised clinical trial (Part II). J Oral Rehabil 45:702–709
Troiano G, Lo Russo L, Canullo L et al (2018) Early and late implant failure of submerged versus non-submerged implant healing: A systematic review, meta-analysis and trial sequential analysis. J Clin Periodontol 45:613–623
Falco A, Berardini M, Trisi P (2018) Correlation between implant geometry, implant surface, insertion torque, and primary stability: in vitro biomechanical analysis. Int J Oral Maxillofac Implants 33:824–830
Guastaldi FP, Yoo D, Marin C, et al (2003) Plasma treatment maintains surface energy of the implant surface and enhances osseointegration. Int J Biomater 1–6
Queiroz TP, Souza FA, Guastaldi AC et al (2013) Commercially pure titanium implants with surfaces modified by laser beam with and without chemical deposition of apatite. Biomechanical and topographical analysis in rabbits. Clin Oral Implants Res 24:896–903
Souza FA, Queiroz TP, Guastaldi AC et al (2013) Comparative in vivo study of commercially pure Ti implants with surfaces modified by laser with and without silicate deposition: biomechanical and scanning electron microscopy analysis. J Biomed Mater Res B 101:76–84
Faeda RS, Tavares HS, Sartori R et al (2009) Biological performance of chemical hydroxyapatite coating associated with implant surface modification by laser beam: biomechanical study in rabbit tibias. J Oral Maxillofac Surg 67:1706–1715
Mistry S, Roy S, Jyoti Maitra N et al (2016) Safety and efficacy of additive and subtractive surface modification of Ti6Al4V endosseous implant in goat bone. J Mech Behav Biomed Mater 57:69–87
Braga FJC, Marques RFC, Almeida Filho E et al (2007) Surface modification of Ti dental implants by Nd:YVO4 laser irradiation. Appl Surf Sci 253:9203–9208
Faeda RS, Spin-Neto R, Marcantonio E et al (2012) Laser ablation in titanium implants followed by biomimetic hydroxyapatite coating: Histomorphometric study in rabbits. Microsc Res Tech 75:940–948
Sisti KE, de Andrés MC, Johnston D et al (2016) Skeletal stem cell and bone implant interactions are enhanced by LASER titanium modification. Biochem Biophys Res Commun 473:719–725
Bressel TAB, de Queiroz JDF, Gomes Moreira SM et al (2017) Laser-modified titanium surfaces enhance the osteogenic differentiation of human mesenchymal stem cells. Stem Cell Res Ther 8:269
Almeida KP, Delgado-Ruiz R, Carneiro LG et al (2016) Influence of drilling speed on stability of tapered dental implants: an ex vivo experimental study. Int J Oral Maxillofac Implants 31:795–798
Sennerby L, Meredith N (2000) Implant stability measurements using resonance frequency analysis: biological and biomechanical aspects and clinical implications. Periodontol 2008(47):51–66
Sennerby L, Andersson P, Verrocchi D et al (2012) One-year outcomes of Neoss bimodal implants. A prospective clinical, radiographic, and RFA study. Clin Implant Dent R 14:313–320
Gabay E, Cohen O, Machtei EE (2012) A novel device for resonance frequency assessment of one-piece implants. Int J Oral Maxillofac Implants 27:523–527
Schouten C, Meijer G, Beucken J et al (2009) The quantitative assessment of peri-implant bone responses using histomorphometry and micro-computed tomography. Biomaterials 30:4539–4549
Hsu JT, Huang HL, Chang CH et al (2013) Relationship of three-dimensional bone-to-implant contact to primary implant stability and peri-implant bone strain in immediate loading: microcomputed tomographic and in vitro analyses. Int J Oral Maxillofac Implants 28:367–374
World Medical Association (2013) World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA 310:2191–2194
Vazquez L, Nizamaldin Y, Combescure C et al (2013) Accuracy of vertical height measurements on direct digital panoramic radiographs using posterior mandibular implants and metal balls as reference objects. Dentomaxillofac Radiol 42:20110429
Vazquez L, Saulacic N, Belser U et al (2008) Efficacy of panoramic radiographs in the preoperative planning of posterior mandibular implants: a prospective clinical study of 1527 consecutively treated patients. Clin Oral Implants Res 19:81–85
Smeets R, Stadlinger B, Schwarz F, et al (2016) Impact of dental implant surface modifications on osseointegration. Biomed Res Int 6285620
Queiroz TP, de Molon RS, Souza FA et al (2017) In vivo evaluation of cp Ti implants with modified surfaces by laser beam with and without hydroxyapatite chemical deposition and without and with thermal treatment: topographic characterization and histomorphometric analysis in rabbits. Clin Oral Investig 21:685–699
Sisti KE, de Rossi R, Antoniolli AM et al (2012) Surface and biomechanical study of titanium implants modified by laser with and without hydroxyapatite coating, in rabbits. J Oral Implantol 38:231–237
Sisti KE, Piattelli A, Guastaldi AC et al (2013) Nondecalcified histologic study of bone response to titanium implants topographically modified by laser with and without hydroxyapatite coating. Int J Periodont Restor Dent 33:689–696
Souza FA, Queiroz TP, Sonoda CK et al (2014) Histometric analysis and topographic characterization of cp Ti implants with surfaces modified by laser with and without silica deposition. J Biomed Mater Res B 102:1677–1688
Sisti KE, Garcia IR Jr, Guastaldi AC et al (2006) Analysis of titanium surface irradiated with laser, with and without deposited of durapatite. Acta Circ Bras 21:57–62
Oliveira NT, Guastaldi FP, Perrotti V et al (2013) Biomedical Ti-Mo alloys with surface machined and modified by laser beam: biomechanical, histological, and histometric analysis in rabbits. Clin Implant Dent R 15:427–437
Queiroz TP, Aguiar SC, Margonar R et al (2015) Clinical study on survival rate of short implants placed in the posterior mandibular region: resonance frequency analysis. Clin Oral Implants Res 26:1036–1042
Pontes AE, Ribeiro FS, da Silva VC et al (2008) Clinical and radiographic changes around dental implants inserted in different levels in relation to the crestal bone, under different restoration protocols, in the dog model. J Periodontol 79:486–494
Laurell L, Lundgren D (2011) Marginal bone level changes at dental implants after 5 years in function: a meta-analysis. Clin Implant Dent Res 13:19–28
Fernandez-Formoso N, Rilo B, Mora MJ et al (2012) Radiographic evaluation of marginal bone maintenance around tissue level implant and bone level implant: a randomised controlled trial. A 1-year follow-up. J Oral Rehabil 39:830–837
Kinaia BM, Shah M, Neely AL et al (2014) Crestal bone level changes around immediately placed implants: a systematic review and meta-analyses with at least 12 months’ follow-up after functional loading. J Periodontol 85:1537–1548
Aimetti M, Ferrarotti F, Mariani GM et al (2015) Soft tissue and crestal bone changes around implants with platform-switched abutments placed nonsubmerged at subcrestal position: a 2-year clinical and radiographic evaluation. Int J Oral Maxillofac Implants 30:1369–1377
Filippi A, Higginbottom FL, Lambrecht T et al (2013) A prospective noninterventional study to document implant success and survival of the Straumann Bone Level SLActive dental implant in daily dental practice. Quintessence Int 44:499–512
Roccuzzo M, Bonino L, Dalmasso P et al (2014) Long-term results of a three arms prospective cohort study on implants in periodontally compromised patients: 10-year data around sandblasted and acid-etched (SLA) surface. Clin Oral Implants Res 25:1105–1112
van Velzen FJ, Ofec R, Schulten EA et al (2015) 10-year survival rate and the incidence of peri-implant disease of 374 titanium dental implants with a SLA surface: a prospective cohort study in 177 fully and partially edentulous patients. Clin Oral Implants Res 26:1121–1128
Liedke GS, Spin-Neto R, da Silveira HED et al (2017) Factors affecting the possibility to detect buccal bone condition around dental implants using cone beam computed tomography. Clin Oral Implants Res 28:1082–1088
Liedke GS, Spin-Neto R, da Silveira HED et al (2018) Accuracy of detecting and measuring buccal bone thickness adjacent to titanium dental implants-a cone beam computed tomography in vitro study. Oral Surg Oral Med Oral Pathol Oral Radiol 126:432–438
Schropp L, Stavropoulos A, Spin-Neto R et al (2012) Implant image quality in dental radiographs recorded using a customized imaging guide or a standard film holder. Clin Oral Implants Res 23:55–59
Acknowledgements
The authors gratefully acknowledge financial support from the São Paulo Research Foundation (FAPESP; 2014/05626-8). The authors are thankful to Implacil De Bortoli (São Paulo, SP, Brazil) for providing their implants and abutments.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This study was approved by the Research Ethics Committee of the Dentistry Course of the University of Araraquara (UNIARA, SP, Brazil), protocol #580.879, (Certificate of Presentation for Ethical Appreciation: 24020613.8.0000.5383).
Patient Consent
All patients were informed of the study protocol and agreed to sign the consent form prior to being enrolled in the study. All patients were treated according to the principles embodied in the World Medical Association Helsinki Declaration of 1975 for biomedical research involving human subjects, as revised in 2013 (World Medical Association).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Guastaldi, F.P.S., Queiroz, T.P., Marques, D.O. et al. Comparative Evaluation of Implants with Different Surface Treatments Placed in Human Edentulous Mandibles: A 1-Year Prospective Study. J. Maxillofac. Oral Surg. 21, 815–823 (2022). https://doi.org/10.1007/s12663-021-01600-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-021-01600-6