Abstract
Background
We aimed to investigate the prognostic significance of lymph node density (LND), and pre-operative neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) for outcome measuring in tongue squamous cell carcinoma (TSCC)’ patients.
Methods
A total of 129 patients who underwent surgery for TSCC were enrolled in this retrospective study. LND and pre-operative NLR and PLR were used as outcome measures and their correlations with different clinicopathological features were examined.
Results
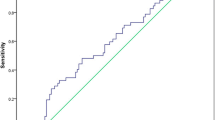
The cutoff values for NLR, PLR, and LND were obtained 1.21, 97.81, and 0.02, respectively, by receiver operating characteristic (ROC) curve approach. Only LND was found to be significantly associated with decreased overall survival (HR = 4.24; 95% CI 1.49–12.10; P = 0.007) and disease-free survival (HR = 3.48; 95% CI 1.43–8.45; P = 0.006) both in univariate and multivariate analyzes.
Conclusion
Based on the findings, the LND has superiority over pre-operative NLR and PLR in predicting outcomes for the patients with TSCC.




Similar content being viewed by others
References
Feller L, Lemmer J (2012) Oral squamous cell carcinoma: epidemiology, clinical presentation and treatment. J Cancer Ther 3(04):263
Palve DH, Tupkari JV (2008) Clinico-pathological correlation of micronuclei in oral squamous cell carcinoma by exfoliative cytology. J Oral MaxillofacPathol 12(1):2
Bachar G, Hod R, Goldstein D, Irish J, Gullane P, Brown D et al (2011) Outcome of oral tongue squamous cell carcinoma in patients with and without known risk factors. Oral Oncol 47(1):45–50
Veness MJ, Morgan GJ, Sathiyaseelan Y, Gebski V (2005) Anterior tongue cancer and the incidence of cervical lymph node metastases with increasing tumour thickness: should elective treatment to the neck be standard practice in all patients? ANZ J Surg 75(3):101–105
Ganly I, Goldstein D, Carlson DL, Patel SG, O’Sullivan B, Lee N et al (2013) Long-term regional control and survival in patients with “low-risk”, early stage oral tongue cancer managed by partial glossectomy and neck dissection without postoperative radiation: the importance of tumor thickness. Cancer 119(6):1168–1176
Zhang L, Zhou X, Yao X, Wu Y, Zhang Q, Zhang L (2012) Oral tongue cancer patients show a better overall survival than base of tongue cancer patients. J Cancer Res ClinOncol 138(2):341–346
Tsai YD, Wang CP, Chen CY, Lin LW, Hwang TZ, Lu LF et al (2014) Pretreatment circulating monocyte count associated with poor prognosis in patients with oral cavity cancer. Head Neck 36(7):947–953
Piccard H, Muschel R, Opdenakker G (2012) On the dual roles and polarized phenotypes of neutrophils in tumor development and progression. Crit Rev OncolHematol 82(3):296–309
Zhou C, Liu J, Tang Y, Liang X (2012) Inflammation linking EMT and cancer stem cells. Oral Oncol 48(11):1068–1075
Chua W, Charles K, Baracos V, Clarke S (2011) Neutrophil/lymphocyte ratio predicts chemotherapy outcomes in patients with advanced colorectal cancer. Br J Cancer 104(8):1288
Yodying H, Matsuda A, Miyashita M, Matsumoto S, Sakurazawa N, Yamada M et al (2016) Prognostic significance of neutrophil-to-lymphocyte ratio and platelet-to-lymphocyte ratio in oncologic outcomes of esophageal cancer: a systematic review and meta-analysis. Ann SurgOncol 23(2):646–654
Wei X, Wang F, Zhang D, Qiu M, Ren C, Jin Y et al (2015) A novel inflammation-based prognostic score in esophageal squamous cell carcinoma: the C-reactive protein/albumin ratio. BMC Cancer 15(1):350
Hashimoto K, Ikeda Y, Korenaga D, Tanoue K, Hamatake M, Kawasaki K et al (2005) The impact of preoperative serum C-reactive protein on the prognosis of patients with hepatocellular carcinoma. Cancer 103(9):1856–1864
Azab B, Bhatt VR, Phookan J, Murukutla S, Kohn N, Terjanian T et al (2012) Usefulness of the neutrophil-to-lymphocyte ratio in predicting short-and long-term mortality in breast cancer patients. Ann SurgOncol 19(1):217–224
Krenn-Pilko S, Langsenlehner U, Thurner E, Stojakovic T, Pichler M, Gerger A et al (2014) The elevated preoperative platelet-to-lymphocyte ratio predicts poor prognosis in breast cancer patients. Br J Cancer 110(10):2524
Kitano Y, Yamashita Y-I, Yamamura K, Arima K, Kaida T, Miyata T et al (2017) Effects of preoperative neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios on survival in patients with extrahepaticcholangiocarcinoma. Anticancer Res 37(6):3229–3237
Chen S, Guo J, Feng C, Ke Z, Chen L, Pan Y (2016) The preoperative platelet–lymphocyte ratio versus neutrophil–lymphocyte ratio: which is better as a prognostic factor in oral squamous cell carcinoma? TherAdv Med Oncol 8(3):160–167
Osawa T, Abe T, Shinohara N, Harabayashi T, Sazawa A, Kubota K et al (2009) Role of lymph node density in predicting survival of patients with lymph node metastases after radical cystectomy: a multi-institutional study. Int J Urol 16(3):274–278
Patel S, Amit M, Yen T, Liao C, Chaturvedi P, Agarwal J et al (2013) Lymph node density in oral cavity cancer: results of the International Consortium for Outcomes Research. Br J Cancer 109(8):2087
Huang SH, O’Sullivan B (2017) Overview of the 8th edition TNM classification for head and neck cancer. Curr Treat Options Oncol 18(7):40
Amit M, Tam S, Takahashi H, Choi KY, Zafereo M, Bell D et al (2019) Prognostic performance of the American Joint Committee on Cancer 8th edition of the TNM staging system in patients with early oral tongue cancer. Head Neck 41(5):1270–1276
Sun W, Zhang L, Luo M, Hu G, Mei Q, Liu D et al (2016) Pretreatment hematologic markers as prognostic factors in patients with nasopharyngeal carcinoma: Neutrophil-lymphocyte ratio and platelet-lymphocyte ratio. Head Neck 38(S1):E1332–E1340
Ma X, Wang Y, Sheng H, Tian W, Qi Z, Teng F et al (2014) Prognostic significance of thrombocytosis, platelet parameters and aggregation rates in epithelial ovarian cancer. J ObstetrGynaecol Res 40(1):178–183
Gentles AJ, Newman AM, Liu CL, Bratman SV, Feng W, Kim D et al (2015) The prognostic landscape of genes and infiltrating immune cells across human cancers. Nat Med 21(8):938–945
Wu L, Saxena S, Awaji M, Singh RK (2019) Tumor-associated neutrophils in cancer: going pro. Cancers 11(4):564
Gargiulo P, Dietrich D, Herrmann R, Bodoky G, Ruhstaller T, Scheithauer W et al (2019) Predicting mortality and adverse events in patients with advanced pancreatic cancer treated with palliative gemcitabine-based chemotherapy in a multicentre phase III randomized clinical trial: the APC-SAKK risk scores. TherapAdv Med Oncol 11:1758835918818351
Ozturk K, Akyildiz NS, Uslu M, Gode S, Uluoz U (2016) The effect of preoperative neutrophil, platelet and lymphocyte counts on local recurrence and survival in early-stage tongue cancer. Eur Arch Otorhinolaryngol 273(12):4425–4429
Ong HS, Gokavarapu S, Wang LZ, Tian Z, Zhang CP (2017) Low pretreatment lymphocyte–monocyte ratio and high platelet-lymphocyte ratio indicate poor cancer outcome in early tongue cancer. J Oral MaxillofacSurg 75(8):1762–1774
Grimm M, Rieth J, Hoefert S, Krimmel M, Rieth S, Teriete P et al (2016) Standardized pretreatment inflammatory laboratory markers and calculated ratios in patients with oral squamous cell carcinoma. Eur Arch Otorhinolaryngol 273(10):3371–3384
Acharya S, Rai P, Hallikeri K, Anehosur V, Kale J (2017) Preoperative platelet lymphocyte ratio is superior to neutrophil lymphocyte ratio to be used as predictive marker for lymph node metastasis in oral squamous cell carcinoma. Journal of investigative and clinical dentistry 8(3):e12219
Sano Y, Kogashiwa Y, Araki R, Enoki Y, Ikeda T, Yoda T et al (2018) Correlation of inflammatory markers, survival, and COX2 expression in oral cancer and implications for prognosis. Otolaryngology-Head and Neck Surgery 158(4):667–676
Zhang Y, Zheng L, Quan L, Du L. Prognostic role of platelet‐to‐lymphocyte ratio in oral cancer: A meta‐analysis. Journal of Oral Pathology & Medicine. 2019.
Yu W, Dou Y, Wang K, Liu Y, Sun J, Gao H et al (2019) Preoperative neutrophil lymphocyte ratio but not platelet lymphocyte ratio predicts survival and early relapse in patients with oral, pharyngeal, and lip cancer. Head Neck 41(5):1468–1474
Bharath V, Balagopal P, Nebu A, Jayasudha A, Iqbal MA, Sebastian P (2018) Can Metastatic Lymph node ratio be used as an independent prognostic factor in Carcinoma tongue? The Gulf journal of oncology 1(28):6–10
Lieng H, Gebski VJ, Morgan GJ, Veness MJ (2016) Important prognostic significance of lymph node density in patients with node positive oral tongue cancer. ANZ J Surg 86(9):681–686
Kim K-Y, Cha I-H (2012) Risk stratification of oral cancer patients using a combined prognostic factor including lymph node density and biomarker. J Cancer Res ClinOncol 138(3):483–490
Kim SY, Nam SY, Choi S-H, Cho K-J, Roh J-L (2011) Prognostic value of lymph node density in node-positive patients with oral squamous cell carcinoma. Ann SurgOncol 18(8):2310–2317
Suzuki H, Hanai N, Hirakawa H, Nishikawa D, Hasegawa Y (2015) Lymph node density is a prognostic factor in patients with major salivary gland carcinoma. Oncology letters 10(6):3523–3528
Martin TA, Ye L, Sanders AJ, Lane J, Jiang WG. Cancer invasion and metastasis: molecular and cellular perspective. Madame Curie Bioscience Database [Internet]. Landes Bioscience; 2013.
Jones D, Pereira ER, Padera TP (2018) Growth and immune evasion of lymph node metastasis. Frontiers in oncology 8:36
Wang Q, Zhu D (2019) The prognostic value of systemic immune-inflammation index (SII) in patients after radical operation for carcinoma of stomach in gastric cancer. Journal of gastrointestinal oncology 10(5):965
Li C, Tian W, Zhao F, Li M, Ye Q, Wei Y et al (2018) Systemic immune-inflammation index, SII, for prognosis of elderly patients with newly diagnosed tumors. Oncotarget 9(82):35293
Diao P, Wu Y, Li J, Zhang W, Huang R, Zhou C et al (2018) Preoperative systemic immune-inflammation index predicts prognosis of patients with oral squamous cell carcinoma after curative resection. J Transl Med 16(1):365
Acknowledgements
This work was carried out at Cancer Institute, Tehran University of Medical Sciences, Tehran, Iran and financially was supported by Tehran University of Medical Sciences, Tehran, Iran [Grant NO# 97-02-51-39760]. The authors would like to give special thanks to the all staffs of Cancer Institute and Medical University of Tehran.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no financial or commercial conflicts of interest and are responsible for the content and writing of this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Khazravi, M., Shirkhoda, M., Saffar, H. et al. Prognostic Value of Lymph Node Density Compared to Pre-operative Platelet-to-Lymphocyte Ratio and Neutrophil-to-Lymphocyte Ratio in Patients with Tongue Squamous Cell Carcinoma. J. Maxillofac. Oral Surg. 21, 845–855 (2022). https://doi.org/10.1007/s12663-021-01524-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-021-01524-1