Abstract
Objectives
Investigate the activity of rhythmic masseter muscles activity (RMMA) during sleep in patients with dentofacial deformities.
Materials and methods
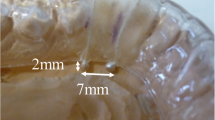
Fifty patients with dentofacial deformities (16 male, 34 female) who required orthognathic surgery. An electrode was attached to the masseter muscle bilaterally, and preoperative polysomnography was performed. The frequency of RMMA onset per hour was measured on the left and the right sides. Values were classified as phasic (grinding: P-RMMA) and tonic (clenching: T-RMMA) to examine the onset of RMMA. Correlation between the RMMA index and various morphological and physical factors were determined including sleep or awake, rapid eye movement (REM), non-rapid eye movement (NREM) phases (NR1-NR4) in the sleep stage, phasic and tonic, gender, and mandibular asymmetry.
Results
The RMMA index values at the time of sleep were significantly small than during awake. The values were significantly higher during the NREM sleep than during the REM sleep and were the highest in the NR1 phase. P-RMMA index was significantly higher than the T-RMMA index. The P-RMMA index was also significantly higher than the T-RMMA index for men. In patients with greater asymmetry in the RMMA index values between the left and the right side (more than 30% difference), deviation between the midpoint of the maxillary and the mandibular incisal edges (U1-L1 deviation) was significantly higher.
Conclusion
RMMA in patients with dentofacial deformity was statistically higher in awake than sleep, higher in NREM sleep than REM sleep, higher in male than female on grinding, and higher in upper and lower incisor high deviation.







Similar content being viewed by others
References
Lobbezoo F, Ahlberg J, Glaros AG, Kato T, Koyano K, Lavigne GJ, Winocur E (2013) Bruxism defined and graded: an international consensus. J Oral Rehabil 40:2–4
Sateia MJ (2014) International classification of sleep disorders–third edition (ICSD-3). Am Acad Sleep Med 146:1387–1394
De Leeuw R (2008) Orofacial pain guidelines for assessment, diagnosis, and management, 4th edn. Quintessence, Chicago
Kalamir A, Pollard H, Vitiello AL, Bonello R (2017) TMD and the problem of bruxism. A review. J Bodyw Mov Ther 11:183–193
Berger M, Szalewski L, Szkutnik J, Ginszt M, Ginszt A (2017) Different association between specific manifestations of bruxism and temporomandibular disorder pain. Neurol Neurochir Pol 51:7–11
Palinkas M, Semprini M, Filho JE, de Luca CG, Regalo IH, Bataglion C, Regalo SCH (2017) Nocturnal sleep architecture is altered by sleep bruxism. Arch Oral Biol 81:56–60
Stuginski-Barbosa J, Porporatti AL, Costa YM, Svensson P, Conti PC (2017) Agreement of the international classification of sleep disorders criteria with polysomnography for sleep bruxism diagnosis: a preliminary study. J Prosthet Dent 117:61–66
Deniz C, Ozdemir F, Eraydin F, Celakil T (2017) Effect of orthognathic surgery on masticatory performance and muscle activity in skeletal Class III patients. CRANIO® 36:174–180
Lavigne GJ, Rompre PH, Montplaisir JY (1996) Sleep bruxism: validity of clinical research diagnostic criteria in a controlled polysomnographic study. J Dent Res 75:546–552
Manfredini D, Ahlberg J, Wetselaar P, Svensson P, Lobbezoo F (2019) The bruxism construct: from cut-off points to a continuum spectrum. J Oral Rehabil 46:991–997
De Oliveira TM, Gómez Rodríguez A (2014) Polysomnographic analysis of bruxism. Gen Dent 62:56–60
Budtz-Jørgensen E (1981) Occlusal dysfunction and stress. J Oral Rehabil 8:1–9
Firmani M, Reyes M, Becerra N, Flores G, Weitzman M, Espinosa P (2015) Sleep bruxism in children and adolescents. Rev Chil Pediatr 86:373–379
Lobbezoo F, Naeije M (2001) Bruxism is mainly regulated centrally, not peripherally. J Oral Rehabil 28:1085–1091
Sugimoto K, Yoshimi H, Sasaguri K, Sato S (2011) Occlusion factors influencing the magnitude of sleep bruxism activity. Cranio 29:127–137
Jokubauskas L, Baltrušaitytė A, Pileičikienė G (2018) Oral appliances for managing sleep bruxism in adults: a systematic review from 2007 to 2017. J Oral Rehabil 45:81–95
Gomes CA, El Hage Y, Amaral AP, Politti F, Biasotto-Gonzalez DA (2014) Effects of massage therapy and occlusal splint therapy on electromyographic activity and the intensity of signs and symptoms in individuals with temporomandibular disorder and sleep bruxism: a randomized clinical trial. Chiropr Man Ther 22:43
Wolford LM, Reiche-Fischel O, Mehra P (2003) Changes in temporomandibular joint dysfunction after orthognathic surgery. J Oral Maxillofacc Surg 61:655–660
Kato T, Masuda Y, Yoshida A, Morimoto T (2011) Masseter EMG activity during sleep and sleep bruxism. Arch Ital Biol 149:478–491
Singh PK, Alvi HA, Singh BP, Singh RD, Kant S, Jurel DA (2015) Evaluation of various treatment modalities in sleep bruxism. J Prosthet Dent 114:426–431
Mude AH, Kawakami S, Kato S, Minagi S (2018) Properties of tonic episodes of masseter muscle activity during waking hours and sleep in subjects with and without history of orofacial pain. J Prosthodont Res 62:234–238
Funding
None to declare.
Author information
Authors and Affiliations
Contributions
Y. F. and K. O. designed most of the experiments and wrote the main manuscript text and prepared all figures and tables. R. J. and S. T. are the primary person responsible for carrying out all experimental procedures. M. M. and Y. N. analyzed the data. K. K. and S. T. are the person who made the final approval of the article.
Corresponding author
Ethics declarations
Conflict of interest
The author declare that they have no conflict of interest.
Ethical Approval
This study was approved by Kanazawa University Hospital Research Ethical Committee (Ref. No. 1765-1).
Informed Consent
All patients were informed about the research purpose and agreed to use their clinical data for this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Futani, Y., Ooi, K., Jokaji, R. et al. Evaluation of Rhythmic Masseter Muscle Activity during Sleep and Awake in Patients with Dentofacial Deformity. J. Maxillofac. Oral Surg. 21, 481–486 (2022). https://doi.org/10.1007/s12663-020-01467-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12663-020-01467-z